Tuesday Poster Session
Category: Interventional Endoscopy
P5645 - Outcomes of Dual Antiplatelet Therapy versus Anticoagulation Plus Aspirin in Upper Endoscopic GI Dilation: A TriNetX Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- OA
Osama Alshakhatreh, MD (he/him/his)
Albany Medical Center
Norfolk, VA
Presenting Author(s)
Omar Arman, MD, MPH1, Osama Alshakhatreh, MD2, Tarick Ahmad, BS2, Tejash E. Sikka, BS3, Ibrahim Mohammed, MD2, Shunsa Tarar, DO2, Seth Richter, MD, FACG2
1University at Buffalo, Buffalo, NY; 2Albany Medical Center, Albany, NY; 3Albany Medical College, Albany, NY
Introduction: Upper gastrointestinal (GI) endoscopic dilation is a procedure with a moderate risk for bleeding, yet limited insight exists to guide antithrombotic management peri-procedurally. While current gastroenterology guidelines provide recommendations for holding P2Y12 inhibitors or anticoagulation (AC), the safety of continuing dual antiplatelet therapy (DAPT) or AC plus aspirin remains uncertain. Prior studies have not directly compared these regimens in the context of endoscopic dilation. This study presents real-world comparative data on post-procedural outcomes in patients receiving DAPT versus AC plus aspirin.
Methods: A retrospective cohort study was conducted using a TriNetX which is a large, federated health research network. Individuals undergoing upper GI endoscopic dilation were determined using CPT and ICD-10-PCS codes. Patients with antithrombotic use within 7 days prior to the procedure were divided into two groups: DAPT (aspirin + P2Y12 inhibitor), and AC + aspirin (including apixaban, rivaroxaban, dabigatran, edoxaban, or warfarin). A 1:1 propensity score match was performed, balancing demographics and comorbidities including CKD, CAD, and PPI use. Outcomes included GI bleeding, transfusion, and hospitalization. Falsification endpoints were analyzed to assess residual confounding.
Results: A total of 2,324 patients were included after 1:1 propensity score matching (1,162 per group). Patients receiving DAPT had a non-significantly higher rate of gastrointestinal bleeding compared to those on AC plus aspirin (11.5% vs 9.9%, p = 0.203). Similarly, transfusion requirements were slightly higher in the DAPT group (7.8% vs 6.3%, p = 0.145). In contrast, hospitalization rates were significantly lower in the DAPT group compared to the AC plus aspirin group (49.1% vs 54.2%, p = 0.013).
Falsification endpoints were similar between groups, supporting the internal validity of the comparison.
Discussion: In this propensity-matched analysis, patients receiving DAPT had lower hospitalization rates and comparable risks of bleeding, and transfusions compared to those receiving AC plus aspirin. Although AC plus aspirin is often perceived as the higher-risk regimen, our findings highlight that the bleeding risk associated with DAPT remains clinically significant and should not be underestimated. This study provides the first direct comparative data between these two antithrombotic strategies in the setting of endoscopic dilation and helps address a key gap in procedural safety guidance.
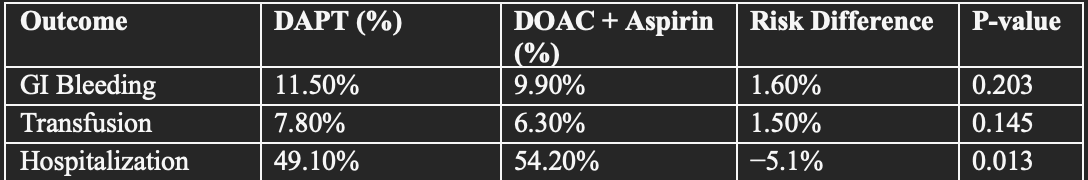
Figure: Table 1 Comparative Risk of Adverse Outcomes After Upper GI Endoscopic Dilation in Patients on DAPT vs AC Plus Aspirin
Disclosures:
Omar Arman indicated no relevant financial relationships.
Osama Alshakhatreh indicated no relevant financial relationships.
Tarick Ahmad indicated no relevant financial relationships.
Tejash Sikka indicated no relevant financial relationships.
Ibrahim Mohammed indicated no relevant financial relationships.
Shunsa Tarar indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Omar Arman, MD, MPH1, Osama Alshakhatreh, MD2, Tarick Ahmad, BS2, Tejash E. Sikka, BS3, Ibrahim Mohammed, MD2, Shunsa Tarar, DO2, Seth Richter, MD, FACG2. P5645 - Outcomes of Dual Antiplatelet Therapy versus Anticoagulation Plus Aspirin in Upper Endoscopic GI Dilation: A TriNetX Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2Albany Medical Center, Albany, NY; 3Albany Medical College, Albany, NY
Introduction: Upper gastrointestinal (GI) endoscopic dilation is a procedure with a moderate risk for bleeding, yet limited insight exists to guide antithrombotic management peri-procedurally. While current gastroenterology guidelines provide recommendations for holding P2Y12 inhibitors or anticoagulation (AC), the safety of continuing dual antiplatelet therapy (DAPT) or AC plus aspirin remains uncertain. Prior studies have not directly compared these regimens in the context of endoscopic dilation. This study presents real-world comparative data on post-procedural outcomes in patients receiving DAPT versus AC plus aspirin.
Methods: A retrospective cohort study was conducted using a TriNetX which is a large, federated health research network. Individuals undergoing upper GI endoscopic dilation were determined using CPT and ICD-10-PCS codes. Patients with antithrombotic use within 7 days prior to the procedure were divided into two groups: DAPT (aspirin + P2Y12 inhibitor), and AC + aspirin (including apixaban, rivaroxaban, dabigatran, edoxaban, or warfarin). A 1:1 propensity score match was performed, balancing demographics and comorbidities including CKD, CAD, and PPI use. Outcomes included GI bleeding, transfusion, and hospitalization. Falsification endpoints were analyzed to assess residual confounding.
Results: A total of 2,324 patients were included after 1:1 propensity score matching (1,162 per group). Patients receiving DAPT had a non-significantly higher rate of gastrointestinal bleeding compared to those on AC plus aspirin (11.5% vs 9.9%, p = 0.203). Similarly, transfusion requirements were slightly higher in the DAPT group (7.8% vs 6.3%, p = 0.145). In contrast, hospitalization rates were significantly lower in the DAPT group compared to the AC plus aspirin group (49.1% vs 54.2%, p = 0.013).
Falsification endpoints were similar between groups, supporting the internal validity of the comparison.
Discussion: In this propensity-matched analysis, patients receiving DAPT had lower hospitalization rates and comparable risks of bleeding, and transfusions compared to those receiving AC plus aspirin. Although AC plus aspirin is often perceived as the higher-risk regimen, our findings highlight that the bleeding risk associated with DAPT remains clinically significant and should not be underestimated. This study provides the first direct comparative data between these two antithrombotic strategies in the setting of endoscopic dilation and helps address a key gap in procedural safety guidance.
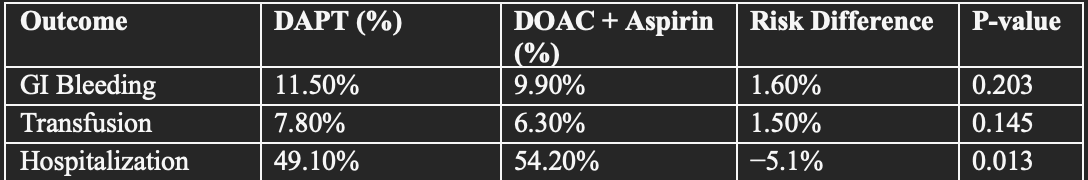
Figure: Table 1 Comparative Risk of Adverse Outcomes After Upper GI Endoscopic Dilation in Patients on DAPT vs AC Plus Aspirin
Disclosures:
Omar Arman indicated no relevant financial relationships.
Osama Alshakhatreh indicated no relevant financial relationships.
Tarick Ahmad indicated no relevant financial relationships.
Tejash Sikka indicated no relevant financial relationships.
Ibrahim Mohammed indicated no relevant financial relationships.
Shunsa Tarar indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Omar Arman, MD, MPH1, Osama Alshakhatreh, MD2, Tarick Ahmad, BS2, Tejash E. Sikka, BS3, Ibrahim Mohammed, MD2, Shunsa Tarar, DO2, Seth Richter, MD, FACG2. P5645 - Outcomes of Dual Antiplatelet Therapy versus Anticoagulation Plus Aspirin in Upper Endoscopic GI Dilation: A TriNetX Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
