Tuesday Poster Session
Category: Infections and Microbiome
P5642 - Gastrointestinal Tuberculosis: An Uncommon Case
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Giri Movva, MD
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Giri Movva, MD1, Saki Kawaguchi, MD2, Edward Butt, MD, MPH1, Keita Hibako, MD3, Tetsuya Hoshi, MD2, Norman M. Farr, MD, MPH1, Brooke Corning, MD1
1University of Texas Medical Branch, Galveston, TX; 2Teine Keijinkai Hospital, Teine Ward, Sapporo, Hokkaido, Japan; 3Shirakaba Zaitaku Clinic, Shiroishi-ku, Sapporo, Hokkaido, Japan
Introduction: Tuberculosis (TB), caused by Mycobacterium tuberculosis, was the most prevalent infectious disease globally before the COVID-19 pandemic, with pulmonary TB being the primary presentation. Extrapulmonary TB (EXPTB) can also occur, with gastrointestinal TB (GITB) being the most frequent infection. Here, we present a case of abdominal TB.
Case Description/
Methods: A 34-year-old male with no past medical history presented with seven days of abdominal distension. He had recently moved to Japan 9 months ago from Nepal. Symptoms include early satiety, cough, subjective fevers, and unintentional 20 lbs weight loss over nine months. He denied abdominal pain or hemoptysis. His vital exams were unremarkable, and physical exam revealed a distended but non-tender abdomen. Pertinent labs are summarized in Table 1. No pathogenic organisms were isolated from 3 sputum cultures.
Abdominal CT scan revealed bilateral pleural effusion and large volume ascites with peritoneal thickening (Figure 1A), raising concern for peritoneal carcinomatosis or disseminated malignancy. Paracentesis was performed (results in Table 1).
The patient underwent esophagogastroduodenoscopy (EGD) and colonoscopy. EGD showed gastric mucosal erosions with gastric biopsy revealing inflamed gastric mucosa. Colonoscopy revealed a ring-like ulcer in the ascending colon (Figure 1B). Biopsy of the ulcer was positive on Ziehl-Neelsen staining, polymerase chain reaction (PCR), and culture confirming Mycobacterium tuberculosis. The patient was diagnosed with tuberculous peritonitis and intestinal tuberculosis. He was started on a four-drug TB regimen. Follow-up sputum cultures at two weeks remained negative.
Discussion: Abdominal TB accounts for 1%-3% of all TB cases worldwide. While TB can affect any part of the gastrointestinal tract, the ileocecal region is the most commonly involved site, with some studies also highlighting the ascending colon as a frequent site. Diagnosis of GITB is challenging due to its non-specific symptoms. Ascitic fluid is typically straw-colored, with a white cell count of 500-1500 cells/mm3, protein >2.5 g/dL, and serum-ascites albumin gradient < 11 g/L. Adenosine Deaminase levels >30 U/L have a 94% sensitivity for diagnosis. Imaging may show peritoneal involvement, ascites, lymphadenopathy, and bowel wall thickening; however, microbiological diagnosis via endoscopic biopsy has a 100% specificity and positive predictive value. Treatment is a six-month course of standard anti-TB therapy.
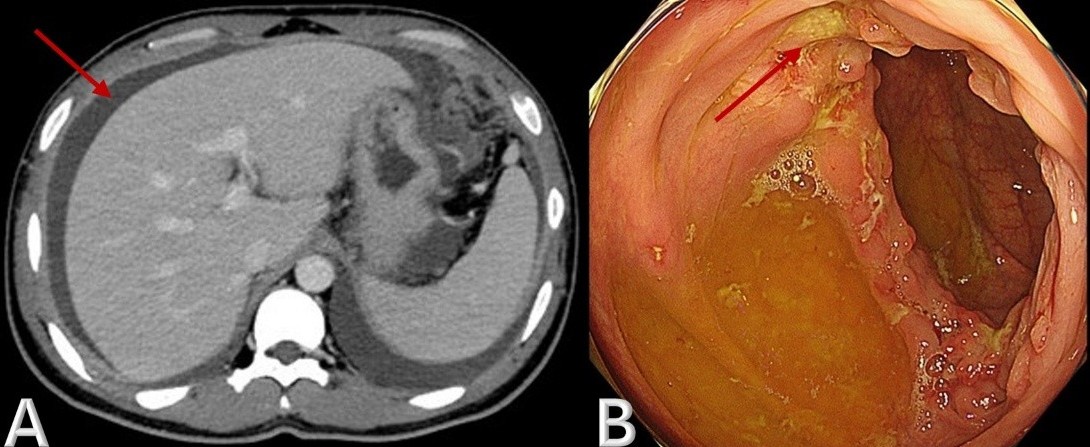
Figure: Figure 1. A) CT Abdomen (Axial)- shows large volume ascites (red arrow) with peritoneal thickening. B) EGD showing ring ulcer (red arrow) in the ascending colon.
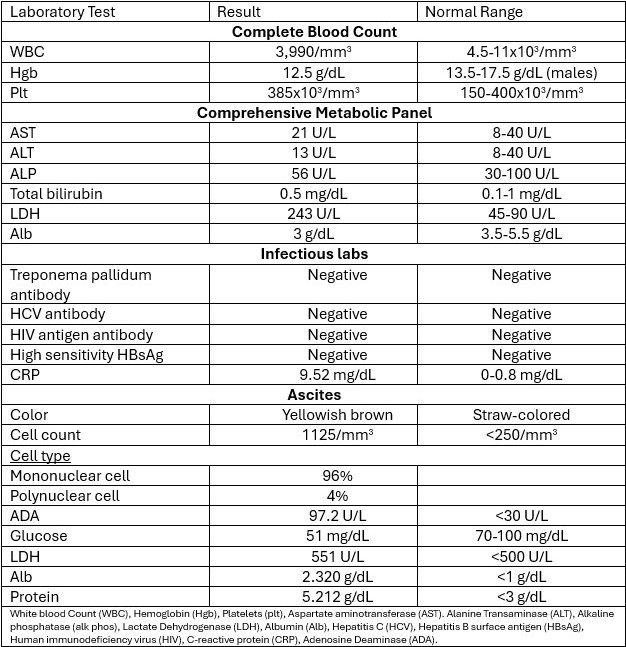
Figure: Table 1: Laboratory Values
Disclosures:
Giri Movva indicated no relevant financial relationships.
Saki Kawaguchi indicated no relevant financial relationships.
Edward Butt indicated no relevant financial relationships.
Keita Hibako indicated no relevant financial relationships.
Tetsuya Hoshi indicated no relevant financial relationships.
Norman Farr indicated no relevant financial relationships.
Brooke Corning indicated no relevant financial relationships.
Giri Movva, MD1, Saki Kawaguchi, MD2, Edward Butt, MD, MPH1, Keita Hibako, MD3, Tetsuya Hoshi, MD2, Norman M. Farr, MD, MPH1, Brooke Corning, MD1. P5642 - Gastrointestinal Tuberculosis: An Uncommon Case, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2Teine Keijinkai Hospital, Teine Ward, Sapporo, Hokkaido, Japan; 3Shirakaba Zaitaku Clinic, Shiroishi-ku, Sapporo, Hokkaido, Japan
Introduction: Tuberculosis (TB), caused by Mycobacterium tuberculosis, was the most prevalent infectious disease globally before the COVID-19 pandemic, with pulmonary TB being the primary presentation. Extrapulmonary TB (EXPTB) can also occur, with gastrointestinal TB (GITB) being the most frequent infection. Here, we present a case of abdominal TB.
Case Description/
Methods: A 34-year-old male with no past medical history presented with seven days of abdominal distension. He had recently moved to Japan 9 months ago from Nepal. Symptoms include early satiety, cough, subjective fevers, and unintentional 20 lbs weight loss over nine months. He denied abdominal pain or hemoptysis. His vital exams were unremarkable, and physical exam revealed a distended but non-tender abdomen. Pertinent labs are summarized in Table 1. No pathogenic organisms were isolated from 3 sputum cultures.
Abdominal CT scan revealed bilateral pleural effusion and large volume ascites with peritoneal thickening (Figure 1A), raising concern for peritoneal carcinomatosis or disseminated malignancy. Paracentesis was performed (results in Table 1).
The patient underwent esophagogastroduodenoscopy (EGD) and colonoscopy. EGD showed gastric mucosal erosions with gastric biopsy revealing inflamed gastric mucosa. Colonoscopy revealed a ring-like ulcer in the ascending colon (Figure 1B). Biopsy of the ulcer was positive on Ziehl-Neelsen staining, polymerase chain reaction (PCR), and culture confirming Mycobacterium tuberculosis. The patient was diagnosed with tuberculous peritonitis and intestinal tuberculosis. He was started on a four-drug TB regimen. Follow-up sputum cultures at two weeks remained negative.
Discussion: Abdominal TB accounts for 1%-3% of all TB cases worldwide. While TB can affect any part of the gastrointestinal tract, the ileocecal region is the most commonly involved site, with some studies also highlighting the ascending colon as a frequent site. Diagnosis of GITB is challenging due to its non-specific symptoms. Ascitic fluid is typically straw-colored, with a white cell count of 500-1500 cells/mm3, protein >2.5 g/dL, and serum-ascites albumin gradient < 11 g/L. Adenosine Deaminase levels >30 U/L have a 94% sensitivity for diagnosis. Imaging may show peritoneal involvement, ascites, lymphadenopathy, and bowel wall thickening; however, microbiological diagnosis via endoscopic biopsy has a 100% specificity and positive predictive value. Treatment is a six-month course of standard anti-TB therapy.
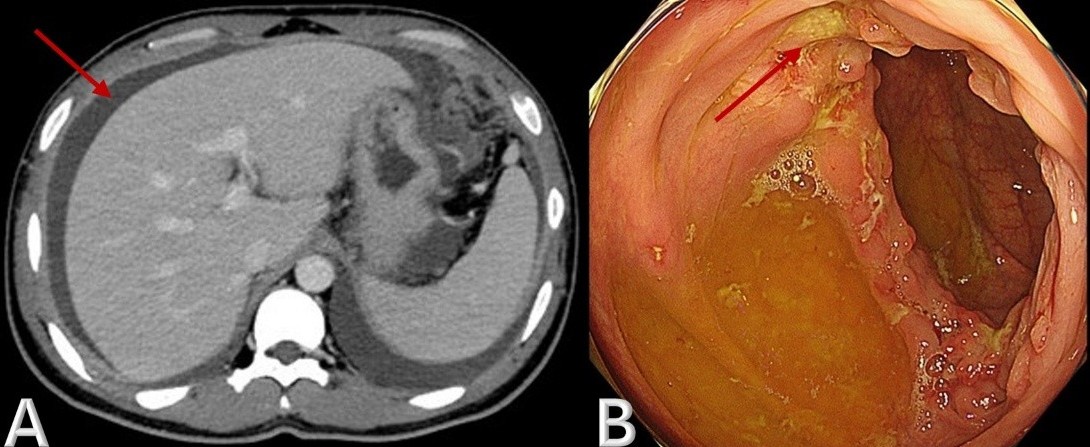
Figure: Figure 1. A) CT Abdomen (Axial)- shows large volume ascites (red arrow) with peritoneal thickening. B) EGD showing ring ulcer (red arrow) in the ascending colon.
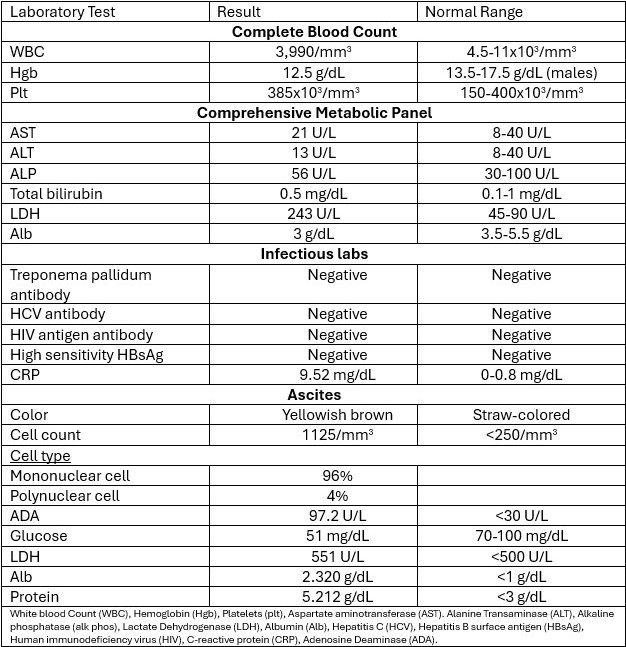
Figure: Table 1: Laboratory Values
Disclosures:
Giri Movva indicated no relevant financial relationships.
Saki Kawaguchi indicated no relevant financial relationships.
Edward Butt indicated no relevant financial relationships.
Keita Hibako indicated no relevant financial relationships.
Tetsuya Hoshi indicated no relevant financial relationships.
Norman Farr indicated no relevant financial relationships.
Brooke Corning indicated no relevant financial relationships.
Giri Movva, MD1, Saki Kawaguchi, MD2, Edward Butt, MD, MPH1, Keita Hibako, MD3, Tetsuya Hoshi, MD2, Norman M. Farr, MD, MPH1, Brooke Corning, MD1. P5642 - Gastrointestinal Tuberculosis: An Uncommon Case, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
