Tuesday Poster Session
Category: Infections and Microbiome
P5630 - Herpes Simplex Virus Proctitis Mimicking IBD in an Immunocompetent Male: A Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DY
Daniel Yoon, MD
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Daniel Yoon, MD1, Pooja Patel, DO1, Liyan Xu, MD1, Berhanu Geme, MD2
1St. Luke's University Health Network, Bethlehem, PA; 2St Luke’s University Health Network, Center Valley, PA
Introduction: Herpes simplex virus (HSV) proctitis is an uncommon diagnosis in immunocompetent individuals and can be missed, especially when initial laboratory and serologic tests are negative. This case aims to show the importance of early endoscopic evaluation and tissue sampling in patients with persistent proctitis symptoms, rather than relying solely on empiric therapy or serologic testing.
Case Description/
Methods: A 29-year-old man with no significant medical history, but with a history of receptive anal intercourse, presented with a month of epigastric pain, nausea, and bloating following unprotected anal exposure. His symptoms soon worsened with rectal prolapse, bloody purulent discharge, and diarrhea. Despite negative STI screening at a sexual health clinic, his symptoms persisted.
Upon hospital admission, laboratory studies revealed a white blood cell count of 19,000. CT imaging showed small bowel intussusception, rectal wall thickening, and extensive lymphadenopathy. He was started on empiric antibiotics—ceftriaxone, doxycycline, and metronidazole—but was lost to follow-up before his symptoms resolved.
Nearly a year later, he returned with ongoing hematochezia and fever. Subsequent colonoscopy revealed edematous, friable, and ulcerated mucosa in the rectosigmoid region. Biopsies demonstrated marked cryptitis and ulceration with confirmation of both HSV-1 and HSV-2 on the immunohistochemical staining, while stains for CMV and Treponema pallidum were negative. Notably, HSV PCR testing was negative.
Discussion: This case highlights two important lessons for gastroenterologists. First, persistent proctitis symptoms should prompt early colonoscopic evaluation with tissue sampling. Relying solely on empiric treatment or serologic testing can delay diagnosis and prolong morbidity. Second, HSV proctitis can present with systemic features such as small bowel intussusception and extensive lymphadenopathy, closely mimicking inflammatory bowel disease or malignancy. Recognizing that HSV proctitis may be part of a broader inflammatory process is key to ensuring an accurate assessment and timely management.
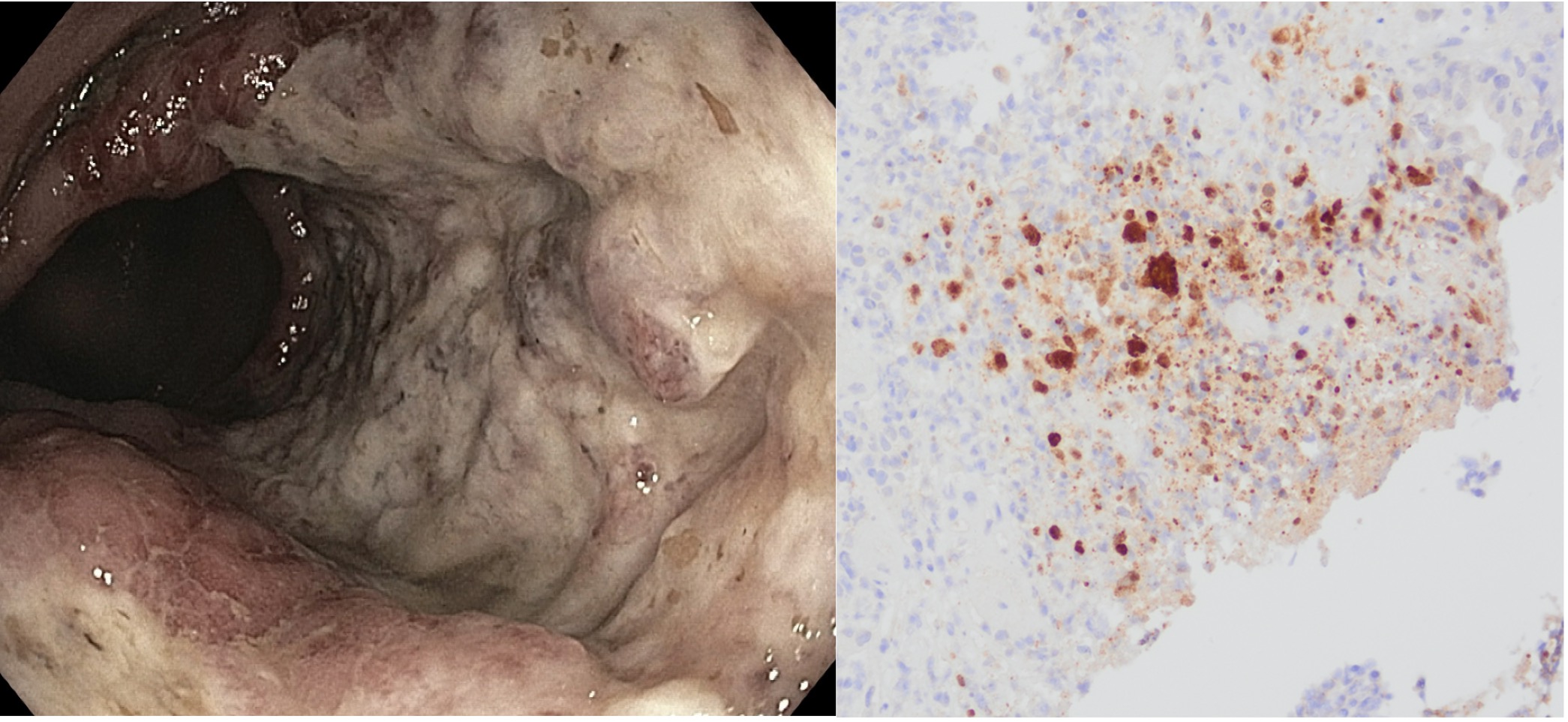
Figure: Figure 1: (A) Localized edematous, erythematous, friable and ulcerated mucosa in the rectosigmoid and rectum; performed cold forceps biopsy to rule out colitis and IBD. (B) Immunohistochemistry stain for herpes simplex 1 & 2.
Disclosures:
Daniel Yoon indicated no relevant financial relationships.
Pooja Patel indicated no relevant financial relationships.
Liyan Xu indicated no relevant financial relationships.
Berhanu Geme indicated no relevant financial relationships.
Daniel Yoon, MD1, Pooja Patel, DO1, Liyan Xu, MD1, Berhanu Geme, MD2. P5630 - Herpes Simplex Virus Proctitis Mimicking IBD in an Immunocompetent Male: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Luke's University Health Network, Bethlehem, PA; 2St Luke’s University Health Network, Center Valley, PA
Introduction: Herpes simplex virus (HSV) proctitis is an uncommon diagnosis in immunocompetent individuals and can be missed, especially when initial laboratory and serologic tests are negative. This case aims to show the importance of early endoscopic evaluation and tissue sampling in patients with persistent proctitis symptoms, rather than relying solely on empiric therapy or serologic testing.
Case Description/
Methods: A 29-year-old man with no significant medical history, but with a history of receptive anal intercourse, presented with a month of epigastric pain, nausea, and bloating following unprotected anal exposure. His symptoms soon worsened with rectal prolapse, bloody purulent discharge, and diarrhea. Despite negative STI screening at a sexual health clinic, his symptoms persisted.
Upon hospital admission, laboratory studies revealed a white blood cell count of 19,000. CT imaging showed small bowel intussusception, rectal wall thickening, and extensive lymphadenopathy. He was started on empiric antibiotics—ceftriaxone, doxycycline, and metronidazole—but was lost to follow-up before his symptoms resolved.
Nearly a year later, he returned with ongoing hematochezia and fever. Subsequent colonoscopy revealed edematous, friable, and ulcerated mucosa in the rectosigmoid region. Biopsies demonstrated marked cryptitis and ulceration with confirmation of both HSV-1 and HSV-2 on the immunohistochemical staining, while stains for CMV and Treponema pallidum were negative. Notably, HSV PCR testing was negative.
Discussion: This case highlights two important lessons for gastroenterologists. First, persistent proctitis symptoms should prompt early colonoscopic evaluation with tissue sampling. Relying solely on empiric treatment or serologic testing can delay diagnosis and prolong morbidity. Second, HSV proctitis can present with systemic features such as small bowel intussusception and extensive lymphadenopathy, closely mimicking inflammatory bowel disease or malignancy. Recognizing that HSV proctitis may be part of a broader inflammatory process is key to ensuring an accurate assessment and timely management.
Figure: Figure 1: (A) Localized edematous, erythematous, friable and ulcerated mucosa in the rectosigmoid and rectum; performed cold forceps biopsy to rule out colitis and IBD. (B) Immunohistochemistry stain for herpes simplex 1 & 2.
Disclosures:
Daniel Yoon indicated no relevant financial relationships.
Pooja Patel indicated no relevant financial relationships.
Liyan Xu indicated no relevant financial relationships.
Berhanu Geme indicated no relevant financial relationships.
Daniel Yoon, MD1, Pooja Patel, DO1, Liyan Xu, MD1, Berhanu Geme, MD2. P5630 - Herpes Simplex Virus Proctitis Mimicking IBD in an Immunocompetent Male: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
