Tuesday Poster Session
Category: Infections and Microbiome
P5619 - Diagnostic Detour: Colovesicular Fistula and Iliopsoas Abscess Masking Metastatic Squamous Cell Carcinoma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AV
Anirudh Vontela, MD (he/him/his)
University of Pittsburgh Medical Center
Pittsburgh, PA
Presenting Author(s)
Ariana R. Tagliaferri, MD1, Vishnu Yanamaladoddi, MD1, Anirudh Vontela, MD2, Amla Patel, MBBS3, Danlu Wang, DO1
1Creighton University School of Medicine, Phoenix, AZ; 2University of Pittsburgh Medical Center, Pittsburgh, PA; 3Creighton University, Phoenix, Phoenix, AZ
Introduction: Colovesicular fistulas (CVFs) are common in diverticular disease or invasive malignancies. When paired with constitutional symptoms and colonic narrowing, suspicion for colorectal cancer is high. Overlapping features may obscure less common etiologies. We present a patient with systemic symptoms initially evaluated for gastrointestinal malignancy, ultimately diagnosed with metastatic squamous cell carcinoma (SCC) of unknown origin via iliopsoas abscess drainage.This case highlights the diagnostic pitfalls due to anchoring bias.
Case Description/
Methods: A 68-year-old-woman with atrial fibrillation and heart failure presented with weight loss, lower abdominal pain, and fecal/urinary incontinence. Labs revealed leukocytosis, microcytic anemia and hypoalbuminemia. CT showed irregular bladder wall thickening, CVF, extensive diverticulosis, bilateral iliopsoas abscesses, necrotic pelvic and retroperitoneal lymphadenopathy, left femoral DVT, bilateral hydronephrosis, and lytic lesions of the sacrum and iliac crest. Bilateral nephrostomy tubes and percutaneous drains were placed for E.Coli bacteremia unresponsive to antibiotics. Bone biopsy showed inflammatory cells, suspicious but non-diagnostic for malignancy. Cultures from the abscess and nephrostomy tube grew VRE Enterococcus faecium and Candida tropicalis; cytology from 4 different samples was non-contributory. Anticoagulation was held due to anemia without bleeding. Endoscopic evaluation was negative for malignancy or bleeding. Despite concern for malignancy, the CVF was attributed to diverticulosis. The patient continued to worsen despite voriconazole and linezolid. Ultimately IR guided drain replacement yielded cytology diagnostic of metastatic SCC. Cystoscopy was deferred as the patient opted for hospice.
Discussion: This case highlights the diagnostic challenge of complex fistula formation. While diverticulosis was initially favored, constitutional symptoms, lymphadenopathy and lytic lesions pointed towards malignancy. Biopsy of the bone lesion was non-diagnostic.The presence of sigmoid strictures and colonic obstruction with ulcerated mucosa around the fistula warranted multiple exams with numerous biopsies, which were all negative.This delayed the diagnosis of metastatic SCC, ultimately diagnosed via cytology from the psoas abscess. Few such cases are reported, with primaries often in the bladder, cervix, or scrotum. A cystoscopy would have been an ideal next step for our patient.

Figure: Coronal CT abdomen showing urinary bladder thickening with wide open colovesicular fistula
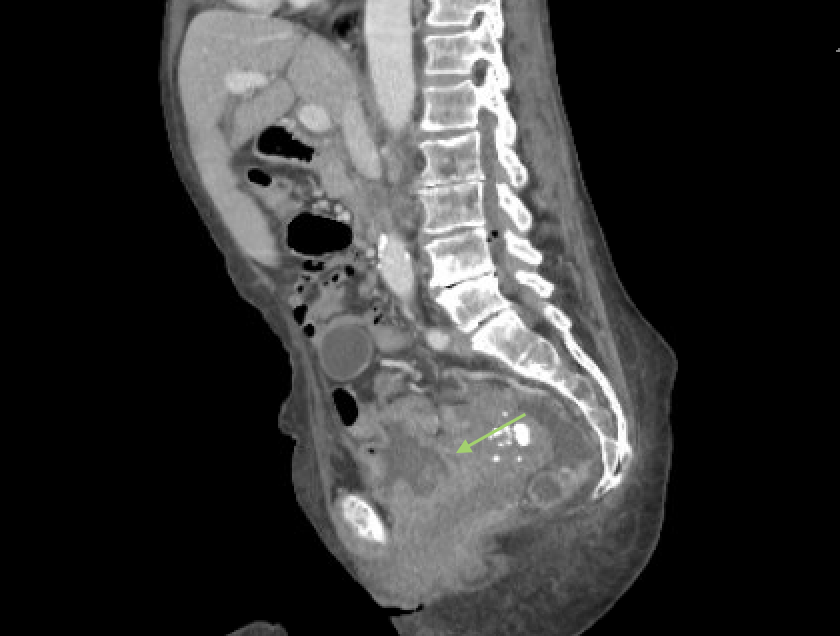
Figure: Sagittal CT showing wide open colovesicular fistula
Disclosures:
Ariana Tagliaferri indicated no relevant financial relationships.
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Anirudh Vontela indicated no relevant financial relationships.
Amla Patel indicated no relevant financial relationships.
Danlu Wang indicated no relevant financial relationships.
Ariana R. Tagliaferri, MD1, Vishnu Yanamaladoddi, MD1, Anirudh Vontela, MD2, Amla Patel, MBBS3, Danlu Wang, DO1. P5619 - Diagnostic Detour: Colovesicular Fistula and Iliopsoas Abscess Masking Metastatic Squamous Cell Carcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2University of Pittsburgh Medical Center, Pittsburgh, PA; 3Creighton University, Phoenix, Phoenix, AZ
Introduction: Colovesicular fistulas (CVFs) are common in diverticular disease or invasive malignancies. When paired with constitutional symptoms and colonic narrowing, suspicion for colorectal cancer is high. Overlapping features may obscure less common etiologies. We present a patient with systemic symptoms initially evaluated for gastrointestinal malignancy, ultimately diagnosed with metastatic squamous cell carcinoma (SCC) of unknown origin via iliopsoas abscess drainage.This case highlights the diagnostic pitfalls due to anchoring bias.
Case Description/
Methods: A 68-year-old-woman with atrial fibrillation and heart failure presented with weight loss, lower abdominal pain, and fecal/urinary incontinence. Labs revealed leukocytosis, microcytic anemia and hypoalbuminemia. CT showed irregular bladder wall thickening, CVF, extensive diverticulosis, bilateral iliopsoas abscesses, necrotic pelvic and retroperitoneal lymphadenopathy, left femoral DVT, bilateral hydronephrosis, and lytic lesions of the sacrum and iliac crest. Bilateral nephrostomy tubes and percutaneous drains were placed for E.Coli bacteremia unresponsive to antibiotics. Bone biopsy showed inflammatory cells, suspicious but non-diagnostic for malignancy. Cultures from the abscess and nephrostomy tube grew VRE Enterococcus faecium and Candida tropicalis; cytology from 4 different samples was non-contributory. Anticoagulation was held due to anemia without bleeding. Endoscopic evaluation was negative for malignancy or bleeding. Despite concern for malignancy, the CVF was attributed to diverticulosis. The patient continued to worsen despite voriconazole and linezolid. Ultimately IR guided drain replacement yielded cytology diagnostic of metastatic SCC. Cystoscopy was deferred as the patient opted for hospice.
Discussion: This case highlights the diagnostic challenge of complex fistula formation. While diverticulosis was initially favored, constitutional symptoms, lymphadenopathy and lytic lesions pointed towards malignancy. Biopsy of the bone lesion was non-diagnostic.The presence of sigmoid strictures and colonic obstruction with ulcerated mucosa around the fistula warranted multiple exams with numerous biopsies, which were all negative.This delayed the diagnosis of metastatic SCC, ultimately diagnosed via cytology from the psoas abscess. Few such cases are reported, with primaries often in the bladder, cervix, or scrotum. A cystoscopy would have been an ideal next step for our patient.

Figure: Coronal CT abdomen showing urinary bladder thickening with wide open colovesicular fistula
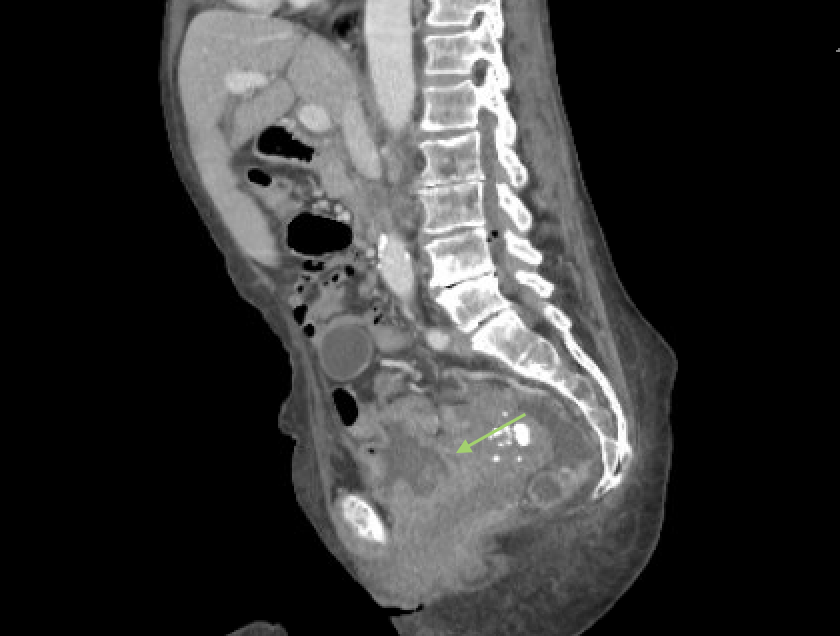
Figure: Sagittal CT showing wide open colovesicular fistula
Disclosures:
Ariana Tagliaferri indicated no relevant financial relationships.
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Anirudh Vontela indicated no relevant financial relationships.
Amla Patel indicated no relevant financial relationships.
Danlu Wang indicated no relevant financial relationships.
Ariana R. Tagliaferri, MD1, Vishnu Yanamaladoddi, MD1, Anirudh Vontela, MD2, Amla Patel, MBBS3, Danlu Wang, DO1. P5619 - Diagnostic Detour: Colovesicular Fistula and Iliopsoas Abscess Masking Metastatic Squamous Cell Carcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
