Tuesday Poster Session
Category: Infections and Microbiome
P5615 - Bile and Error: A Fungal Twist in Hepatic Abscess Formation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Arman Bahmani, MD
Loma Linda University Medical Center - Murrieta
Murrieta, CA
Presenting Author(s)
Arman Bahmani, MD
Loma Linda University Medical Center - Murrieta, Murrieta, CA
Introduction: Fungal liver abscesses, though rare, are increasingly recognized beyond the traditionally immunocompromised demographic. While pyogenic liver abscesses remain more common, fungal infections are gaining attention, especially in patients undergoing multiple endoscopic retrograde cholangiopancreatography (ERCP) procedures.1 ERCP can inadvertently facilitate gut flora translocation to the biliary tree and liver, particularly if there is poor outflow, leading to abscess formation.
Case Description/
Methods: A 50-year-old female with chronic pancreatitis, metabolic-associated fatty liver disease, and prior cholecystectomy presented with a 3-day history of epigastric pain. She previously underwent ERCP with sphincterotomy and biliary stent placement in the common bile duct (CBD). A subsequent ERCP for stent removal revealed significant filling defects with soft stones and sludge. At presentation, vital signs were significant for tachycardia (106 beats/min). Physical examination showed mild epigastric tenderness. Labs indicated a leukocytosis of 15.05 bil/L, lactate of 4 mMol/L, aspartate aminotransferase of 44 u/L, alanine transaminase of 37 u/L, alkaline phosphatase of 259 u/L, and an unremarkable total bilirubin, lipase and cardiac troponin. HIV serology was negative, and ECG showed sinus rhythm. A contrast abdominal CT scan revealed a 5.4 x 2.9 x 1.6-cm irregular rim-enhancing fluid collection in the caudate lobe of the liver and mild dilation of the CBD (Figure 1). CT-guided aspiration yielded 9cc of purulent fluid, culturing Candida albicans. Blood cultures were negative. Initial broad-spectrum antibiotics were transitioned to Fluconazole after culture results. A repeat CT abdomen was scheduled for 6 weeks post-discharge.
Discussion: Traditionally, Candida-related hepatic infections have been linked to severe immunocompromise. However, recent observations suggest that immunocompetent patients undergoing multiple ERCPs and biliary sphincterotomy also face increased risk for fungal liver abscesses.2,3 While bacterial infections are common post-ERCP complications, with cholangitis and sepsis occurring in 0.5% to 3% of cases, studies on the connection between multiple biliary interventions and fungal infections are lacking.4 Our case highlights the importance of considering fungal infections in atypical presentations, especially when antibacterial therapy fails and traditional immunosuppressive factors are absent. This suggests the need for further research to identify high risk individuals.
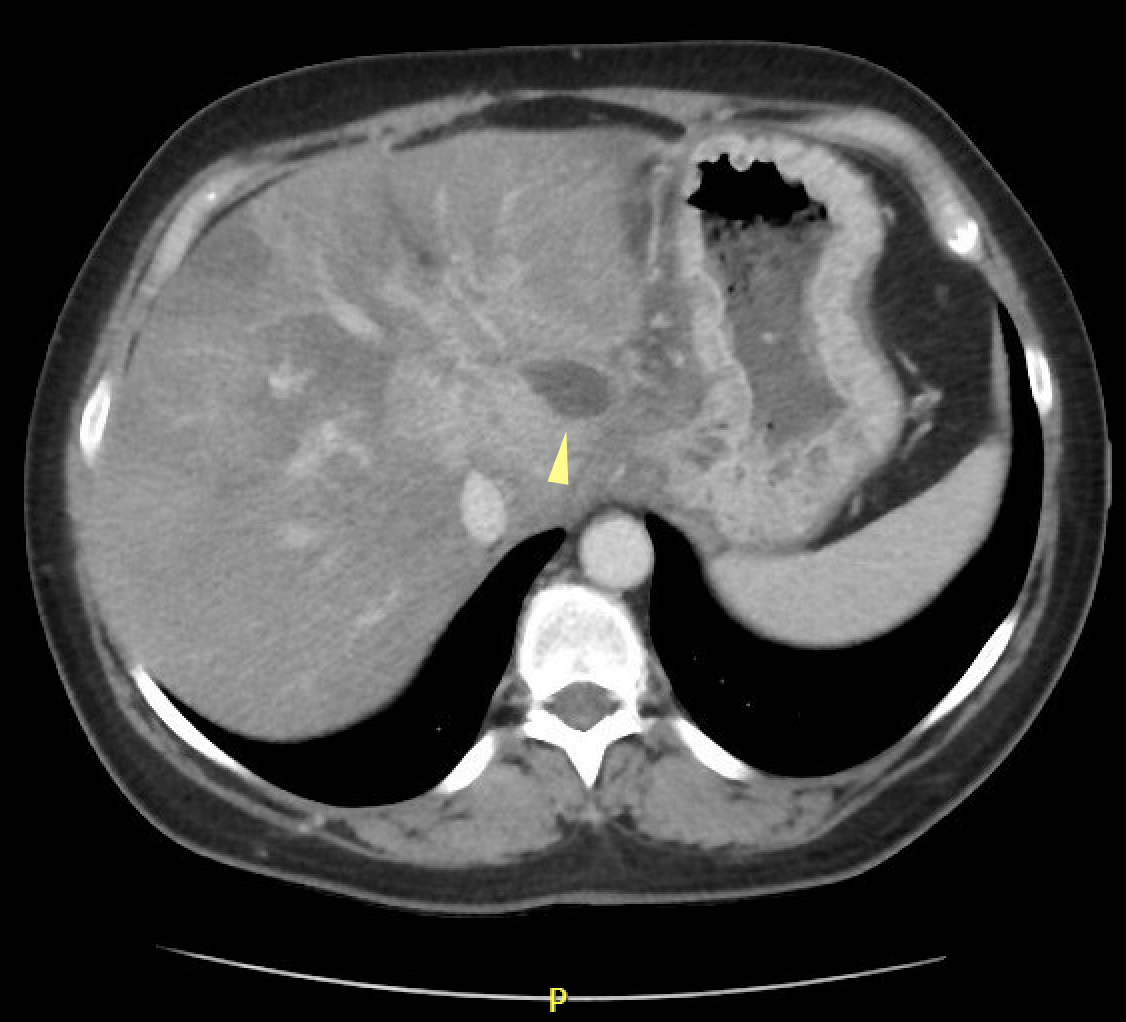
Figure: Figure 1. Contrasted CT Abdomen showing an irregular peripheral fluid density lesion in the caudate lobe of the liver (yellow arrow).
Disclosures:
Arman Bahmani indicated no relevant financial relationships.
Arman Bahmani, MD. P5615 - Bile and Error: A Fungal Twist in Hepatic Abscess Formation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Loma Linda University Medical Center - Murrieta, Murrieta, CA
Introduction: Fungal liver abscesses, though rare, are increasingly recognized beyond the traditionally immunocompromised demographic. While pyogenic liver abscesses remain more common, fungal infections are gaining attention, especially in patients undergoing multiple endoscopic retrograde cholangiopancreatography (ERCP) procedures.1 ERCP can inadvertently facilitate gut flora translocation to the biliary tree and liver, particularly if there is poor outflow, leading to abscess formation.
Case Description/
Methods: A 50-year-old female with chronic pancreatitis, metabolic-associated fatty liver disease, and prior cholecystectomy presented with a 3-day history of epigastric pain. She previously underwent ERCP with sphincterotomy and biliary stent placement in the common bile duct (CBD). A subsequent ERCP for stent removal revealed significant filling defects with soft stones and sludge. At presentation, vital signs were significant for tachycardia (106 beats/min). Physical examination showed mild epigastric tenderness. Labs indicated a leukocytosis of 15.05 bil/L, lactate of 4 mMol/L, aspartate aminotransferase of 44 u/L, alanine transaminase of 37 u/L, alkaline phosphatase of 259 u/L, and an unremarkable total bilirubin, lipase and cardiac troponin. HIV serology was negative, and ECG showed sinus rhythm. A contrast abdominal CT scan revealed a 5.4 x 2.9 x 1.6-cm irregular rim-enhancing fluid collection in the caudate lobe of the liver and mild dilation of the CBD (Figure 1). CT-guided aspiration yielded 9cc of purulent fluid, culturing Candida albicans. Blood cultures were negative. Initial broad-spectrum antibiotics were transitioned to Fluconazole after culture results. A repeat CT abdomen was scheduled for 6 weeks post-discharge.
Discussion: Traditionally, Candida-related hepatic infections have been linked to severe immunocompromise. However, recent observations suggest that immunocompetent patients undergoing multiple ERCPs and biliary sphincterotomy also face increased risk for fungal liver abscesses.2,3 While bacterial infections are common post-ERCP complications, with cholangitis and sepsis occurring in 0.5% to 3% of cases, studies on the connection between multiple biliary interventions and fungal infections are lacking.4 Our case highlights the importance of considering fungal infections in atypical presentations, especially when antibacterial therapy fails and traditional immunosuppressive factors are absent. This suggests the need for further research to identify high risk individuals.
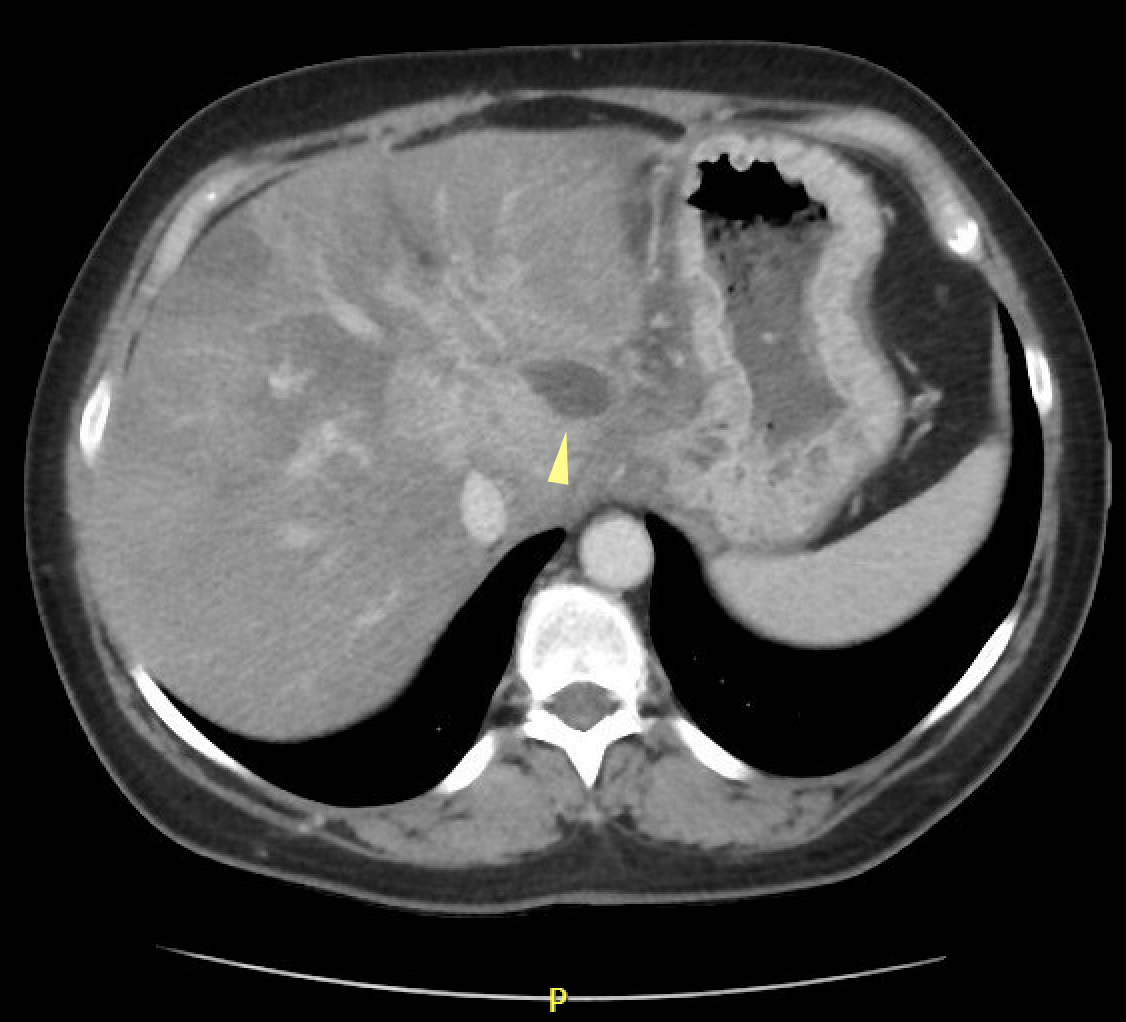
Figure: Figure 1. Contrasted CT Abdomen showing an irregular peripheral fluid density lesion in the caudate lobe of the liver (yellow arrow).
Disclosures:
Arman Bahmani indicated no relevant financial relationships.
Arman Bahmani, MD. P5615 - Bile and Error: A Fungal Twist in Hepatic Abscess Formation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
