Tuesday Poster Session
Category: Infections and Microbiome
P5607 - Unmasking CMV Colitis in an Immunocompetent Patient: A Case of Recurrent Melena and Hematochezia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- IT
Isra N. Taha, MD (she/her/hers)
SSM Health Saint Louis University Hospital
St. Louis, MO
Presenting Author(s)
Isra N. Taha, MD1, Nitin Desai, MD2, Spyridon Zouridis, MD1, Danielle Carpenter, MD1, Kelly Fan, MD1, Mike Giacaman, MD2
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2Saint Louis University, Saint Louis, MO
Introduction: While cytomegalovirus (CMV) seropositivity is common, the development of CMV infection is usually seen in patients with congenital or acquired immunocompromise. Presentation can be variable but can involve hematochezia, abdominal pain, or diarrhea. We describe a case of CMV colitis presenting in an immunocompetent host with no typical risk factors for CMV infection. Given the rarity of such cases and the potentially severe consequences of missed diagnosis, this case report offers insights towards diagnosis and management.
Case Description/
Methods: An 86-year-old woman with chronic obstructive pulmonary disease, hypertension, and pulmonary arterial hypertension presented with one week of dyspnea and fatigue. She was diagnosed with acute pulmonary embolism, and after starting anticoagulation (AC) she developed melena and hematochezia, prompting esophagogastroduodenoscopy (EGD). EGD showed non-bleeding duodenal ulcers with negative biopsies. Her bleeding stopped, but after resuming AC she had recurrent hematochezia and anemia. Subsequent colonoscopy showed bleeding rectal ulcers and colitis in the sigmoid and descending colon. Biopsies were taken; notably, granulomas were not present. Histopathologic analysis revealed ulcerated mucosa with reactive stromal and endothelial cells with inclusions concerning for CMV; positive CMV immunostaining confirmed the diagnosis. CMV DNA was detected by polymerase chain reaction (PCR), with a viral load of 536 IU/mL; HIV serology was negative. She was started on valganciclovir for 3 weeks and returned home in stable condition.
Discussion: This case is unusual in that the patient was found to have CMV colitis despite immunocompetent status. Some studies have suggested that CMV infection in immunocompetent patients can be related to relative immunodeficiency due to impaired cellular and humoral immune function in older age or with comorbidities like diabetes and chronic kidney disease. Diagnosis can be challenging, as serum testing and endoscopy alone do not always yield the diagnosis; endoscopic biopsy with immunohistochemistry staining is the gold standard. Spontaneous resolution is possible, but in severe cases colitis can progress to bowel perforation or necrosis, or death. Patients with risk factors for relative immunosuppression, including older age, chronic kidney disease, diabetes mellitus, untreated solid malignancies, and steroid use, are at risk for severe illness and should be treated with valganciclovir.
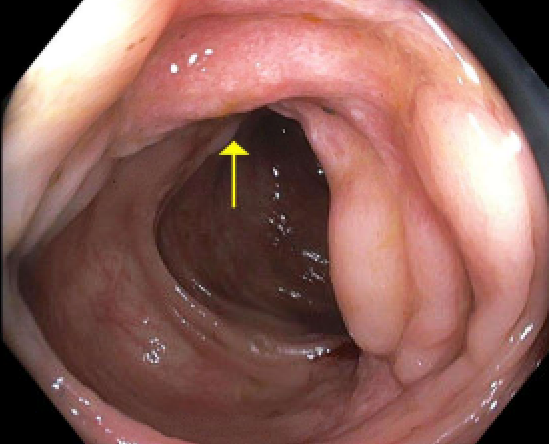
Figure: Endoscopic appearance of descending colon ulcer
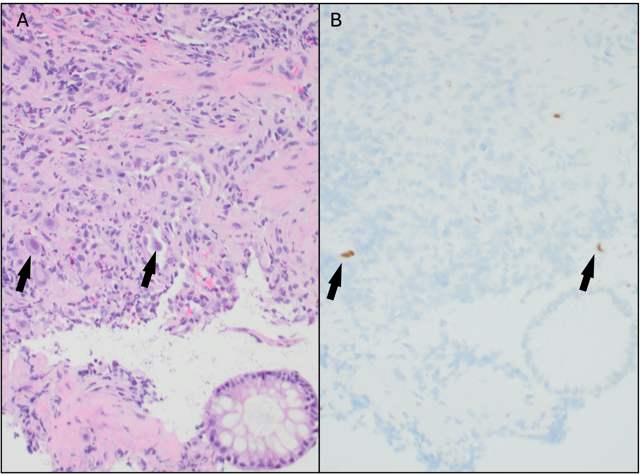
Figure: Ulcerated colonic mucosa sections with H&E stain (A), and CMV immunostain (B) showing viral inclusions (black arrows)
Disclosures:
Isra Taha indicated no relevant financial relationships.
Nitin Desai indicated no relevant financial relationships.
Spyridon Zouridis indicated no relevant financial relationships.
Danielle Carpenter indicated no relevant financial relationships.
Kelly Fan indicated no relevant financial relationships.
Mike Giacaman indicated no relevant financial relationships.
Isra N. Taha, MD1, Nitin Desai, MD2, Spyridon Zouridis, MD1, Danielle Carpenter, MD1, Kelly Fan, MD1, Mike Giacaman, MD2. P5607 - Unmasking CMV Colitis in an Immunocompetent Patient: A Case of Recurrent Melena and Hematochezia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2Saint Louis University, Saint Louis, MO
Introduction: While cytomegalovirus (CMV) seropositivity is common, the development of CMV infection is usually seen in patients with congenital or acquired immunocompromise. Presentation can be variable but can involve hematochezia, abdominal pain, or diarrhea. We describe a case of CMV colitis presenting in an immunocompetent host with no typical risk factors for CMV infection. Given the rarity of such cases and the potentially severe consequences of missed diagnosis, this case report offers insights towards diagnosis and management.
Case Description/
Methods: An 86-year-old woman with chronic obstructive pulmonary disease, hypertension, and pulmonary arterial hypertension presented with one week of dyspnea and fatigue. She was diagnosed with acute pulmonary embolism, and after starting anticoagulation (AC) she developed melena and hematochezia, prompting esophagogastroduodenoscopy (EGD). EGD showed non-bleeding duodenal ulcers with negative biopsies. Her bleeding stopped, but after resuming AC she had recurrent hematochezia and anemia. Subsequent colonoscopy showed bleeding rectal ulcers and colitis in the sigmoid and descending colon. Biopsies were taken; notably, granulomas were not present. Histopathologic analysis revealed ulcerated mucosa with reactive stromal and endothelial cells with inclusions concerning for CMV; positive CMV immunostaining confirmed the diagnosis. CMV DNA was detected by polymerase chain reaction (PCR), with a viral load of 536 IU/mL; HIV serology was negative. She was started on valganciclovir for 3 weeks and returned home in stable condition.
Discussion: This case is unusual in that the patient was found to have CMV colitis despite immunocompetent status. Some studies have suggested that CMV infection in immunocompetent patients can be related to relative immunodeficiency due to impaired cellular and humoral immune function in older age or with comorbidities like diabetes and chronic kidney disease. Diagnosis can be challenging, as serum testing and endoscopy alone do not always yield the diagnosis; endoscopic biopsy with immunohistochemistry staining is the gold standard. Spontaneous resolution is possible, but in severe cases colitis can progress to bowel perforation or necrosis, or death. Patients with risk factors for relative immunosuppression, including older age, chronic kidney disease, diabetes mellitus, untreated solid malignancies, and steroid use, are at risk for severe illness and should be treated with valganciclovir.
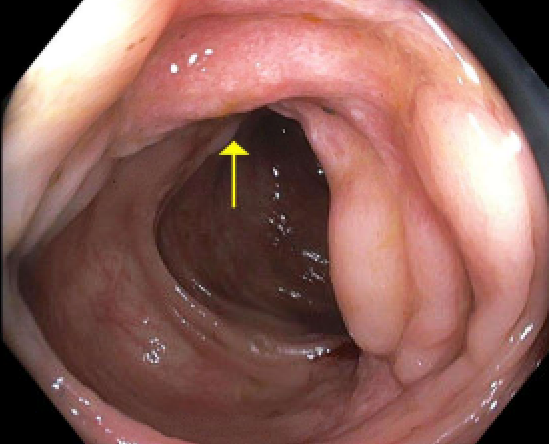
Figure: Endoscopic appearance of descending colon ulcer
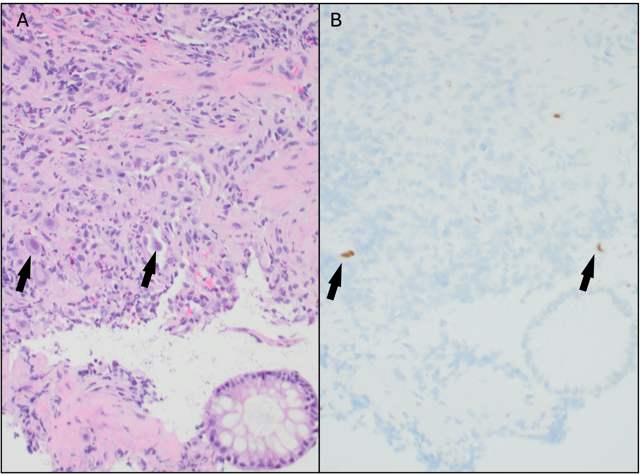
Figure: Ulcerated colonic mucosa sections with H&E stain (A), and CMV immunostain (B) showing viral inclusions (black arrows)
Disclosures:
Isra Taha indicated no relevant financial relationships.
Nitin Desai indicated no relevant financial relationships.
Spyridon Zouridis indicated no relevant financial relationships.
Danielle Carpenter indicated no relevant financial relationships.
Kelly Fan indicated no relevant financial relationships.
Mike Giacaman indicated no relevant financial relationships.
Isra N. Taha, MD1, Nitin Desai, MD2, Spyridon Zouridis, MD1, Danielle Carpenter, MD1, Kelly Fan, MD1, Mike Giacaman, MD2. P5607 - Unmasking CMV Colitis in an Immunocompetent Patient: A Case of Recurrent Melena and Hematochezia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
