Tuesday Poster Session
Category: Infections and Microbiome
P5603 - A Rare Case of Disseminated Tuberculosis Presenting as Abdominal Pain, Diarrhea, and Periprostatic Venous Thrombosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sarah Stewart, BA (she/her/hers)
Weill Cornell Medicine
New York City, NY
Presenting Author(s)
Sarah Stewart, BA1, Danielle Morelli, MD2, David Wan, MD2
1Weill Cornell Medicine, New York City, NY; 2NewYork-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY
Introduction: Disseminated tuberculosis (TB) occurs in < 2% of immunocompetent TB patients and often mimics malignancy or IBD, particularly when accompanied by gastrointestinal (GI) symptoms or TB-associated hypercoagulability (Khan, 2019). The condition may arise as unresolving or recurrent pneumonia, delaying diagnosis. Late recognition increases morbidity, as shown by the ileocecal and thrombotic complications in this case.
Case Description/
Methods: A 45-year-old Haitian male with recent influenza-associated pneumonia presented to the ED with three weeks of productive cough, dyspnea and fevers accompanied by abdominal pain, non-bloody diarrhea and recent 50-pound unintentional weight loss. He denied recent travel or immunosuppression. He works as hospital custodial staff. On exam, he was afebrile but tachycardic and hypotensive with decreased left breath sounds. Labs showed hemoglobin 8.3g/dL, MCV 84, platelets of 542x109/L, and elevated inflammatory markers (procalcitonin 1.47ng/mL, CRP 141mg/L, and ferritin 3151 ng/mL) with negative HIV test. Imaging revealed left lung consolidation, terminal ileal thickening (Figure 1A) and a periprostatic venous thrombus, confirmed on CT venogram (Figure 1B).
Despite antibiotics, he developed recurrent hypotension, tachycardia and fever. AFB culture confirmed TB. He improved on RIPE, ceftriaxone, and LMWH (avoiding DOACs due to rifampin interactions). Endoscopy and GI/hematologic follow-up were deferred to outpatient until TB therapy completion.
Discussion: Disseminated TB is uncommon in immunocompetent individuals and mimics chronic inflammatory or neoplastic processes. Disseminated TB can present with non-resolving pneumonia, particularly in patients from endemic regions and should be considered when symptoms persist. It can mimic GI conditions like IBD (ileal thickening, weight loss, diarrhea with elevated calprotectin) and malignancy (unprovoked thrombosis). TB ileitis lacks the deep transverse ulcerations seen in Crohn’s disease. TB-associated hypercoagulability, seen in up to 2% of TB patients (Dentan et al., 2014), involves TNF-alpha, tissue factor upregulation, and impaired anticoagulation (Mitroi et al., 2025) as illustrated by this rare periprostatic thrombosis without traditional risk factors. High suspicion is required in patients from endemic regions with unexplained thrombosis, GI, and pulmonary symptoms. Multidisciplinary management involves early initiation of RIPE and anticoagulation to decrease morbidity and mortality, then malignancy evaluation.
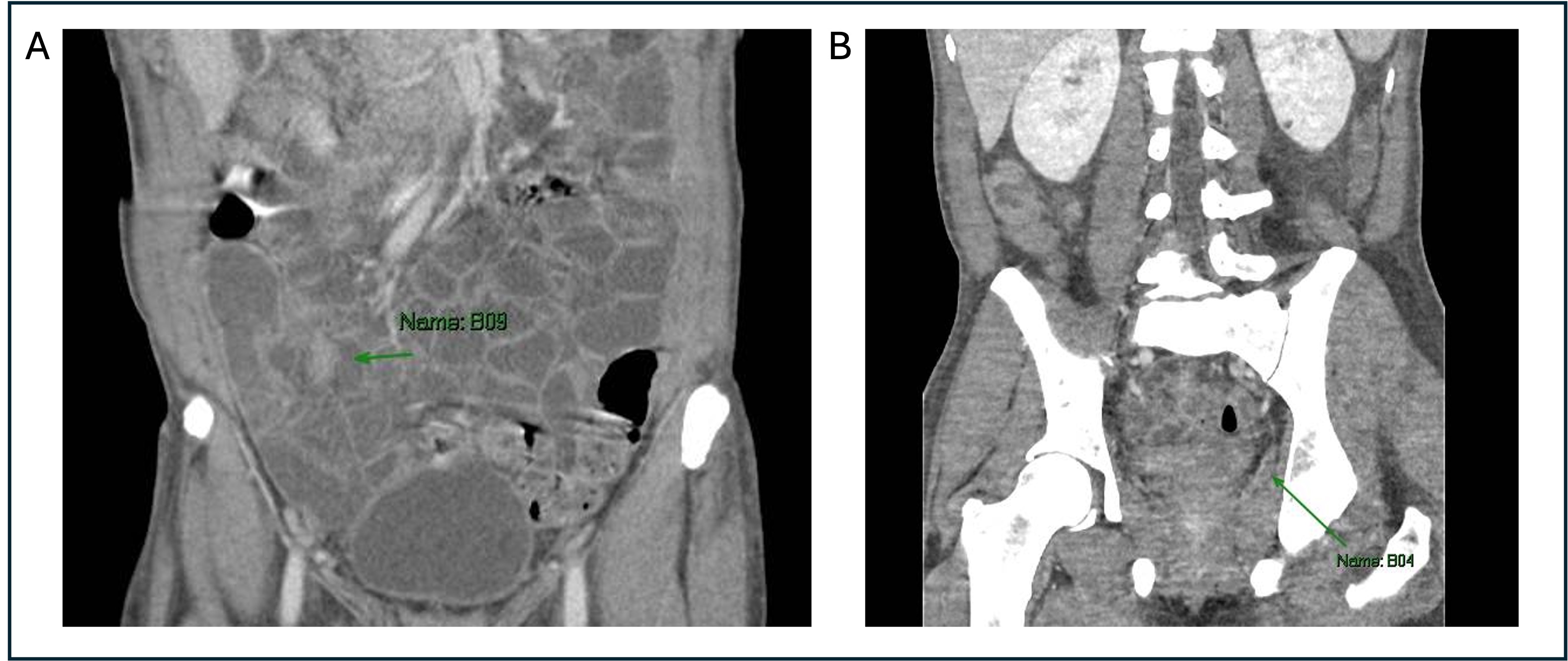
Figure: Figure 1: A. CT of distal ileal wall thickening and enhancement/stricture; B. CT venography of filling defect in branch of left internal iliac vein, superolateral to prostate.
Disclosures:
Sarah Stewart indicated no relevant financial relationships.
Danielle Morelli indicated no relevant financial relationships.
David Wan: Medtronic – Data Monitoring Committee.
Sarah Stewart, BA1, Danielle Morelli, MD2, David Wan, MD2. P5603 - A Rare Case of Disseminated Tuberculosis Presenting as Abdominal Pain, Diarrhea, and Periprostatic Venous Thrombosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Weill Cornell Medicine, New York City, NY; 2NewYork-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY
Introduction: Disseminated tuberculosis (TB) occurs in < 2% of immunocompetent TB patients and often mimics malignancy or IBD, particularly when accompanied by gastrointestinal (GI) symptoms or TB-associated hypercoagulability (Khan, 2019). The condition may arise as unresolving or recurrent pneumonia, delaying diagnosis. Late recognition increases morbidity, as shown by the ileocecal and thrombotic complications in this case.
Case Description/
Methods: A 45-year-old Haitian male with recent influenza-associated pneumonia presented to the ED with three weeks of productive cough, dyspnea and fevers accompanied by abdominal pain, non-bloody diarrhea and recent 50-pound unintentional weight loss. He denied recent travel or immunosuppression. He works as hospital custodial staff. On exam, he was afebrile but tachycardic and hypotensive with decreased left breath sounds. Labs showed hemoglobin 8.3g/dL, MCV 84, platelets of 542x109/L, and elevated inflammatory markers (procalcitonin 1.47ng/mL, CRP 141mg/L, and ferritin 3151 ng/mL) with negative HIV test. Imaging revealed left lung consolidation, terminal ileal thickening (Figure 1A) and a periprostatic venous thrombus, confirmed on CT venogram (Figure 1B).
Despite antibiotics, he developed recurrent hypotension, tachycardia and fever. AFB culture confirmed TB. He improved on RIPE, ceftriaxone, and LMWH (avoiding DOACs due to rifampin interactions). Endoscopy and GI/hematologic follow-up were deferred to outpatient until TB therapy completion.
Discussion: Disseminated TB is uncommon in immunocompetent individuals and mimics chronic inflammatory or neoplastic processes. Disseminated TB can present with non-resolving pneumonia, particularly in patients from endemic regions and should be considered when symptoms persist. It can mimic GI conditions like IBD (ileal thickening, weight loss, diarrhea with elevated calprotectin) and malignancy (unprovoked thrombosis). TB ileitis lacks the deep transverse ulcerations seen in Crohn’s disease. TB-associated hypercoagulability, seen in up to 2% of TB patients (Dentan et al., 2014), involves TNF-alpha, tissue factor upregulation, and impaired anticoagulation (Mitroi et al., 2025) as illustrated by this rare periprostatic thrombosis without traditional risk factors. High suspicion is required in patients from endemic regions with unexplained thrombosis, GI, and pulmonary symptoms. Multidisciplinary management involves early initiation of RIPE and anticoagulation to decrease morbidity and mortality, then malignancy evaluation.
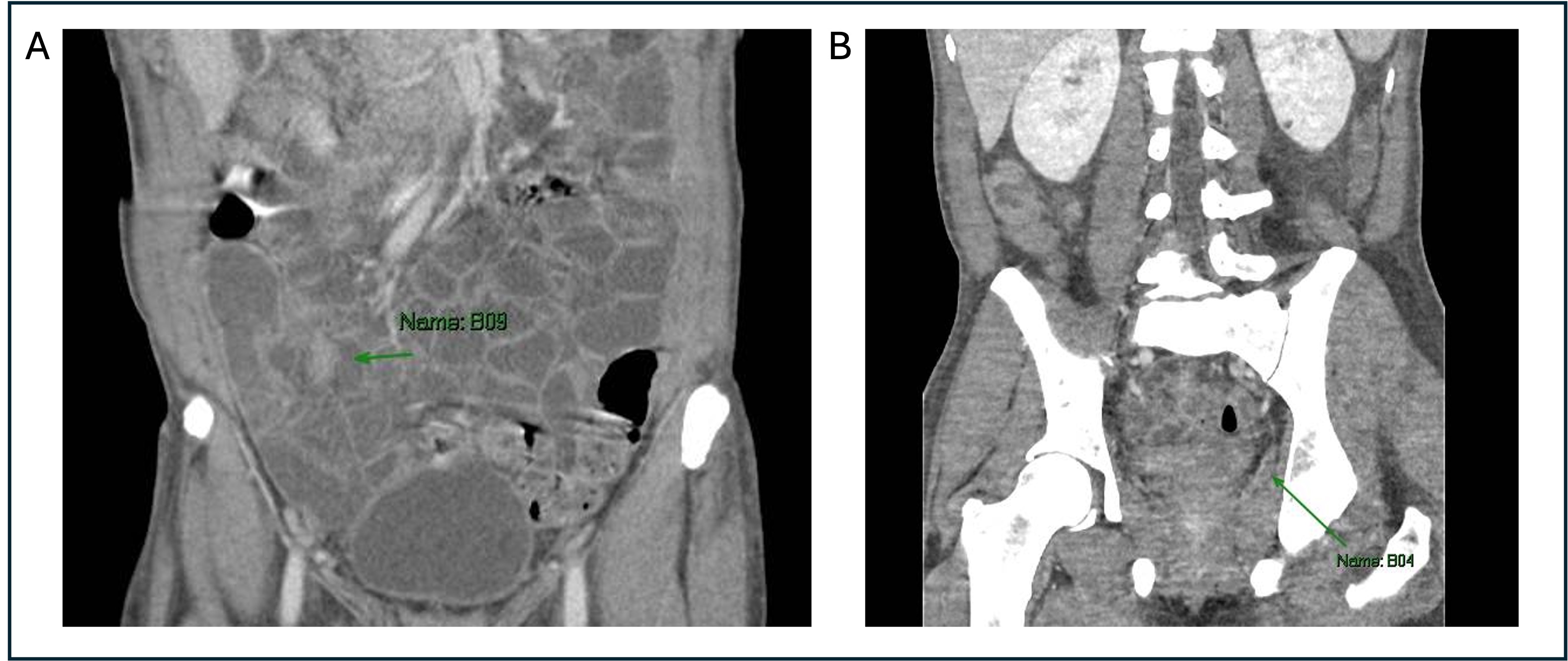
Figure: Figure 1: A. CT of distal ileal wall thickening and enhancement/stricture; B. CT venography of filling defect in branch of left internal iliac vein, superolateral to prostate.
Disclosures:
Sarah Stewart indicated no relevant financial relationships.
Danielle Morelli indicated no relevant financial relationships.
David Wan: Medtronic – Data Monitoring Committee.
Sarah Stewart, BA1, Danielle Morelli, MD2, David Wan, MD2. P5603 - A Rare Case of Disseminated Tuberculosis Presenting as Abdominal Pain, Diarrhea, and Periprostatic Venous Thrombosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
