Tuesday Poster Session
Category: Infections and Microbiome
P5601 - Diverticulitis in the Setting of Heart Failure: A Gut–Heart Axis Manifestation Driven by Mucosal Edema and Systemic Congestion
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Syed Fazal Rizvi, MD (he/him/his)
Chicago Medical School at Rosalind Franklin University of Medicine and Science
Chicago, IL
Presenting Author(s)
Syed Fazal Rizvi, MD1, Jonathan Daniels, MD2
1Chicago Medical School at Rosalind Franklin University of Medicine and Science, Chicago, IL; 2Chicago Medical School at Rosalind Franklin University of Medicine and Science, North Chicago, IL
Introduction: Diverticular disease is a common GI condition, with diverticulitis representing its inflammatory complication. While typically viewed as a localized colonic disorder, diverticulitis can emerge from systemic hemodynamic and inflammatory disturbances. Heart failure (HF), particularly in its decompensated form, induces splanchnic congestion and bowel wall edema, which may predispose patients to diverticular inflammation. The bidirectional relationship between HF and these systems is intricate and not fully understood. Bowel wall edema and malabsorption are prevalent and lead to worse patient outcomes.
Case Description/
Methods: A 70 year old male with HFpEF, diabetes, diverticulosis and CKD presented with progressive abdominal pain, bloating, and vague discomfort. Symptoms worsened over a week and were associated with nausea, reduced appetite, and constipation. OTC medications provided no relief. Examination revealed a distended abdomen with diminished bowel sounds and LLQ tenderness. Initial labs were unremarkable except for rising bicarbonate and bilirubin. Imaging showed borderline splenomegaly, increased central pulmonary markings, EF 60-65%. Despite appropriate diuretics the patient developed worsening LLQ pain, fever, leukocytosis, and worsening labs (K 2.9, Cr 2.33). A CT abdomen revealed focal diverticulitis with bowel wall edema. Management included NPO and IV medication (Diuretics, Ceftriaxone, Electrolyte replacement). On day 3 started on MiraLAX and SGLT2 inhibitor. On Day 5 repeat CT scan demonstrated resolution of bowel wall/mesenteric edema and diverticulitis.
Discussion: This case illustrates how HF-induced bowel edema, impaired peristalsis, and systemic inflammation can facilitate bacterial overgrowth, vascular compromise, and luminal obstruction in diverticula. increase in weight without typical symptoms of HF, strongly indicate Gut edema. Additionally, mucosal edema alters pharmacokinetics, reducing drug efficacy and perpetuating congestion. Emerging article showed SGLT2 inhibitors and short-interval osmotic laxatives, helps in improving gut perfusion, GUT microbiota and reducing intraluminal pressure. Diverticulitis in HF patients may represent a manifestation of the gut–heart axis, driven by mucosal edema, venous congestion, and systemic inflammation. Early recognition and integrated HF-GI management are essential for improving outcomes and reducing recurrent admissions. Bowel rest and transition to IV medication is management of choice in this setting.
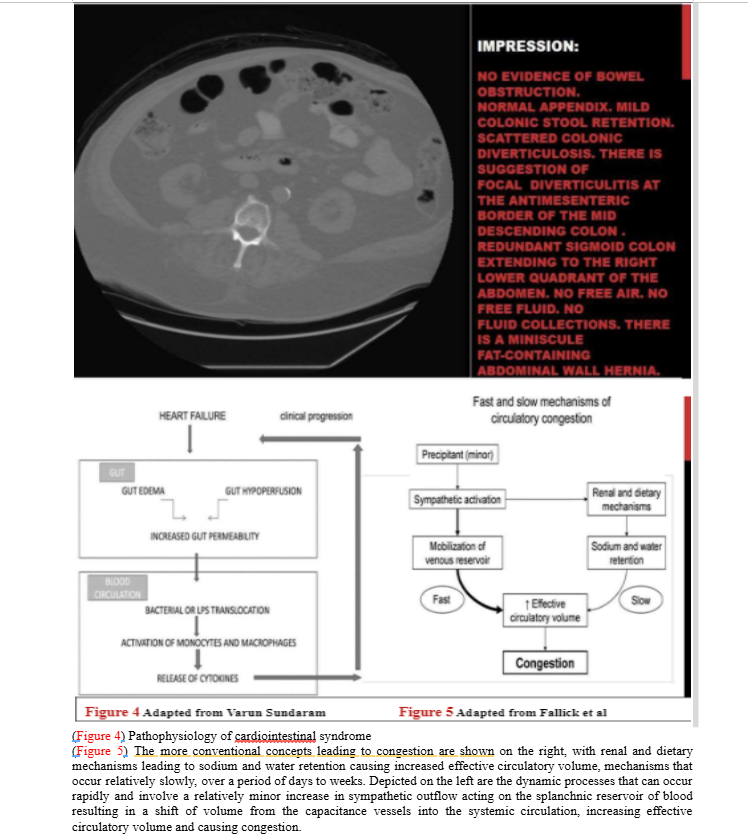
Figure: Gut edema with diverticulitis and mechanism
Disclosures:
Syed Fazal Rizvi indicated no relevant financial relationships.
Jonathan Daniels indicated no relevant financial relationships.
Syed Fazal Rizvi, MD1, Jonathan Daniels, MD2. P5601 - Diverticulitis in the Setting of Heart Failure: A Gut–Heart Axis Manifestation Driven by Mucosal Edema and Systemic Congestion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Chicago Medical School at Rosalind Franklin University of Medicine and Science, Chicago, IL; 2Chicago Medical School at Rosalind Franklin University of Medicine and Science, North Chicago, IL
Introduction: Diverticular disease is a common GI condition, with diverticulitis representing its inflammatory complication. While typically viewed as a localized colonic disorder, diverticulitis can emerge from systemic hemodynamic and inflammatory disturbances. Heart failure (HF), particularly in its decompensated form, induces splanchnic congestion and bowel wall edema, which may predispose patients to diverticular inflammation. The bidirectional relationship between HF and these systems is intricate and not fully understood. Bowel wall edema and malabsorption are prevalent and lead to worse patient outcomes.
Case Description/
Methods: A 70 year old male with HFpEF, diabetes, diverticulosis and CKD presented with progressive abdominal pain, bloating, and vague discomfort. Symptoms worsened over a week and were associated with nausea, reduced appetite, and constipation. OTC medications provided no relief. Examination revealed a distended abdomen with diminished bowel sounds and LLQ tenderness. Initial labs were unremarkable except for rising bicarbonate and bilirubin. Imaging showed borderline splenomegaly, increased central pulmonary markings, EF 60-65%. Despite appropriate diuretics the patient developed worsening LLQ pain, fever, leukocytosis, and worsening labs (K 2.9, Cr 2.33). A CT abdomen revealed focal diverticulitis with bowel wall edema. Management included NPO and IV medication (Diuretics, Ceftriaxone, Electrolyte replacement). On day 3 started on MiraLAX and SGLT2 inhibitor. On Day 5 repeat CT scan demonstrated resolution of bowel wall/mesenteric edema and diverticulitis.
Discussion: This case illustrates how HF-induced bowel edema, impaired peristalsis, and systemic inflammation can facilitate bacterial overgrowth, vascular compromise, and luminal obstruction in diverticula. increase in weight without typical symptoms of HF, strongly indicate Gut edema. Additionally, mucosal edema alters pharmacokinetics, reducing drug efficacy and perpetuating congestion. Emerging article showed SGLT2 inhibitors and short-interval osmotic laxatives, helps in improving gut perfusion, GUT microbiota and reducing intraluminal pressure. Diverticulitis in HF patients may represent a manifestation of the gut–heart axis, driven by mucosal edema, venous congestion, and systemic inflammation. Early recognition and integrated HF-GI management are essential for improving outcomes and reducing recurrent admissions. Bowel rest and transition to IV medication is management of choice in this setting.
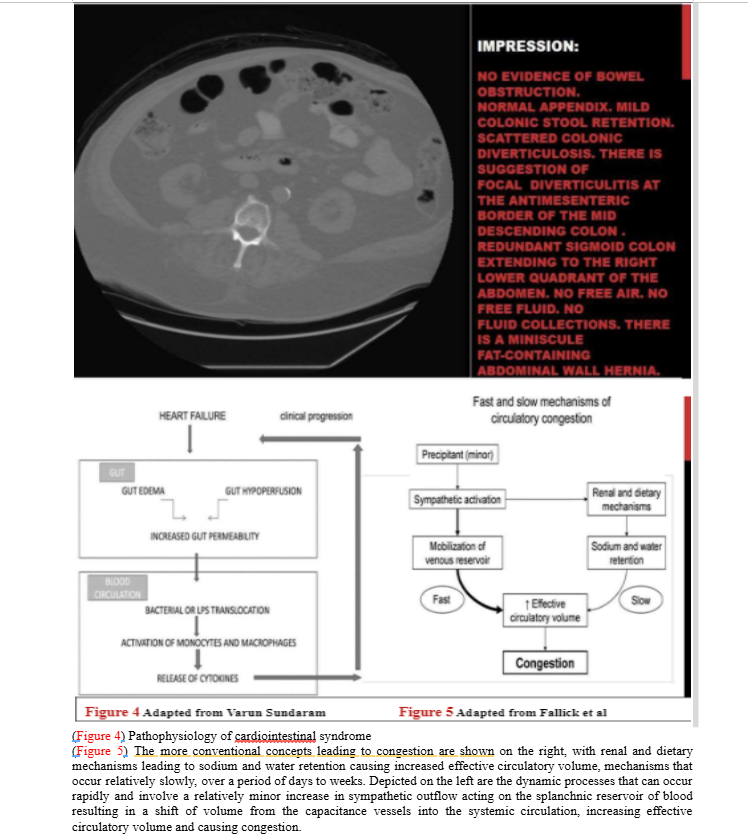
Figure: Gut edema with diverticulitis and mechanism
Disclosures:
Syed Fazal Rizvi indicated no relevant financial relationships.
Jonathan Daniels indicated no relevant financial relationships.
Syed Fazal Rizvi, MD1, Jonathan Daniels, MD2. P5601 - Diverticulitis in the Setting of Heart Failure: A Gut–Heart Axis Manifestation Driven by Mucosal Edema and Systemic Congestion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
