Tuesday Poster Session
Category: IBD
P5544 - Signet-Ring Cell Carcinoma Masquerading as Crohn’s Disease: A Diagnostic Challenge in a Young Woman With Colonic Strictures and Ascites
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ishan Antony, MD
Beth Israel Lahey Health
Burlington, MA
Presenting Author(s)
Ishan Antony, MD1, Samantha Zullow, MD2
1Beth Israel Lahey Health, Burlington, MA; 2Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Colonic strictures with multifocal gastrointestinal inflammation often raise suspicion for Crohn’s disease. However, mimics such as malignancy can elude diagnosis when mucosal biopsies are inconclusive. We present a rare case of metastatic signet-ring cell carcinoma initially presumed to be Crohn’s disease based on imaging and clinical presentation.
Case Description/
Methods: A 39-year-old woman with a history of gastritis and hiatal hernia presented with weeks of worsening abdominal pain, nausea, bilious vomiting, and inability to tolerate solid food. She had recently been treated for “colitis” with ciprofloxacin/metronidazole during a prior hospitalization. She reported a 34 lb unintentional weight loss over six months and increased stool frequency without blood or urgency.
CT imaging revealed gastric wall thickening, terminal ileitis, ascending colitis, and a focal descending colon lesion with upstream transverse colonic dilation. MR enterography confirmed a chronic-appearing stricture near the splenic flexure and active inflammation in the ileocecal region and appendix, with moderate-volume pelvic ascites. Colonoscopy showed normal mucosa to 45 cm, beyond which the lumen was severely narrowed and edematous, precluding scope passage. The stricture appeared extrinsically compressed; biopsies were nonspecific. EGD revealed severe gastric edema and erosions without ulceration or malignancy. Extensive infectious and autoimmune workup, including stool pathogens, celiac serologies, TB, and Entamoeba histolytica, was negative. Ascitic fluid analysis revealed exudative neutrophilic ascites without organisms or malignant cells.
Given progressive obstructive symptoms and diagnostic uncertainty, the patient underwent laparoscopic-assisted subtotal colectomy. Intraoperatively, dense fibrotic adhesions, multiple strictures, and a thickened stomach were noted. Pathology revealed infiltrative signet-ring cell carcinoma involving the colon, appendix, and terminal ileum. The final diagnosis was stage IV signet-ring cell carcinoma with peritoneal carcinomatosis.
Discussion: This case illustrates how diffuse-type gastric cancer can mimic IBD. The submucosal spread pattern explains the negative mucosal biopsies. While Crohn’s disease was the initial leading diagnosis, the absence of endoscopic inflammation, ascites, and fixed stricture morphology prompted reconsideration. In this patient, timely colectomy provided both therapeutic relief and a definitive diagnosis, allowing appropriate oncologic management.
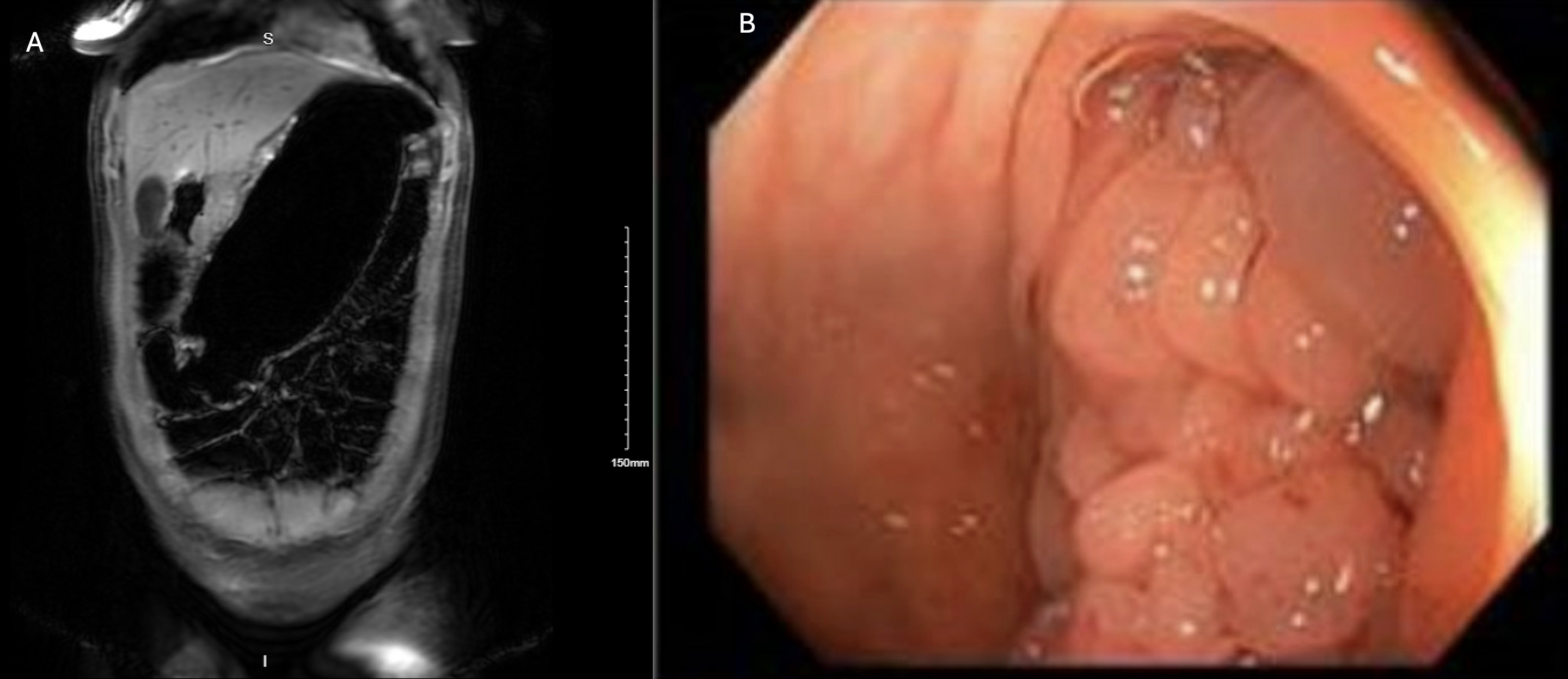
Figure: Figure 1: A) MR enterography showing descending colon stricture and upstream dilation. B) Colonoscopic image at 45 cm: edematous, bulbous, congested tissue.
Disclosures:
Ishan Antony indicated no relevant financial relationships.
Samantha Zullow: Johnson & Johnson – Advisory Committee/Board Member.
Ishan Antony, MD1, Samantha Zullow, MD2. P5544 - Signet-Ring Cell Carcinoma Masquerading as Crohn’s Disease: A Diagnostic Challenge in a Young Woman With Colonic Strictures and Ascites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Beth Israel Lahey Health, Burlington, MA; 2Beth Israel Deaconess Medical Center, Boston, MA
Introduction: Colonic strictures with multifocal gastrointestinal inflammation often raise suspicion for Crohn’s disease. However, mimics such as malignancy can elude diagnosis when mucosal biopsies are inconclusive. We present a rare case of metastatic signet-ring cell carcinoma initially presumed to be Crohn’s disease based on imaging and clinical presentation.
Case Description/
Methods: A 39-year-old woman with a history of gastritis and hiatal hernia presented with weeks of worsening abdominal pain, nausea, bilious vomiting, and inability to tolerate solid food. She had recently been treated for “colitis” with ciprofloxacin/metronidazole during a prior hospitalization. She reported a 34 lb unintentional weight loss over six months and increased stool frequency without blood or urgency.
CT imaging revealed gastric wall thickening, terminal ileitis, ascending colitis, and a focal descending colon lesion with upstream transverse colonic dilation. MR enterography confirmed a chronic-appearing stricture near the splenic flexure and active inflammation in the ileocecal region and appendix, with moderate-volume pelvic ascites. Colonoscopy showed normal mucosa to 45 cm, beyond which the lumen was severely narrowed and edematous, precluding scope passage. The stricture appeared extrinsically compressed; biopsies were nonspecific. EGD revealed severe gastric edema and erosions without ulceration or malignancy. Extensive infectious and autoimmune workup, including stool pathogens, celiac serologies, TB, and Entamoeba histolytica, was negative. Ascitic fluid analysis revealed exudative neutrophilic ascites without organisms or malignant cells.
Given progressive obstructive symptoms and diagnostic uncertainty, the patient underwent laparoscopic-assisted subtotal colectomy. Intraoperatively, dense fibrotic adhesions, multiple strictures, and a thickened stomach were noted. Pathology revealed infiltrative signet-ring cell carcinoma involving the colon, appendix, and terminal ileum. The final diagnosis was stage IV signet-ring cell carcinoma with peritoneal carcinomatosis.
Discussion: This case illustrates how diffuse-type gastric cancer can mimic IBD. The submucosal spread pattern explains the negative mucosal biopsies. While Crohn’s disease was the initial leading diagnosis, the absence of endoscopic inflammation, ascites, and fixed stricture morphology prompted reconsideration. In this patient, timely colectomy provided both therapeutic relief and a definitive diagnosis, allowing appropriate oncologic management.
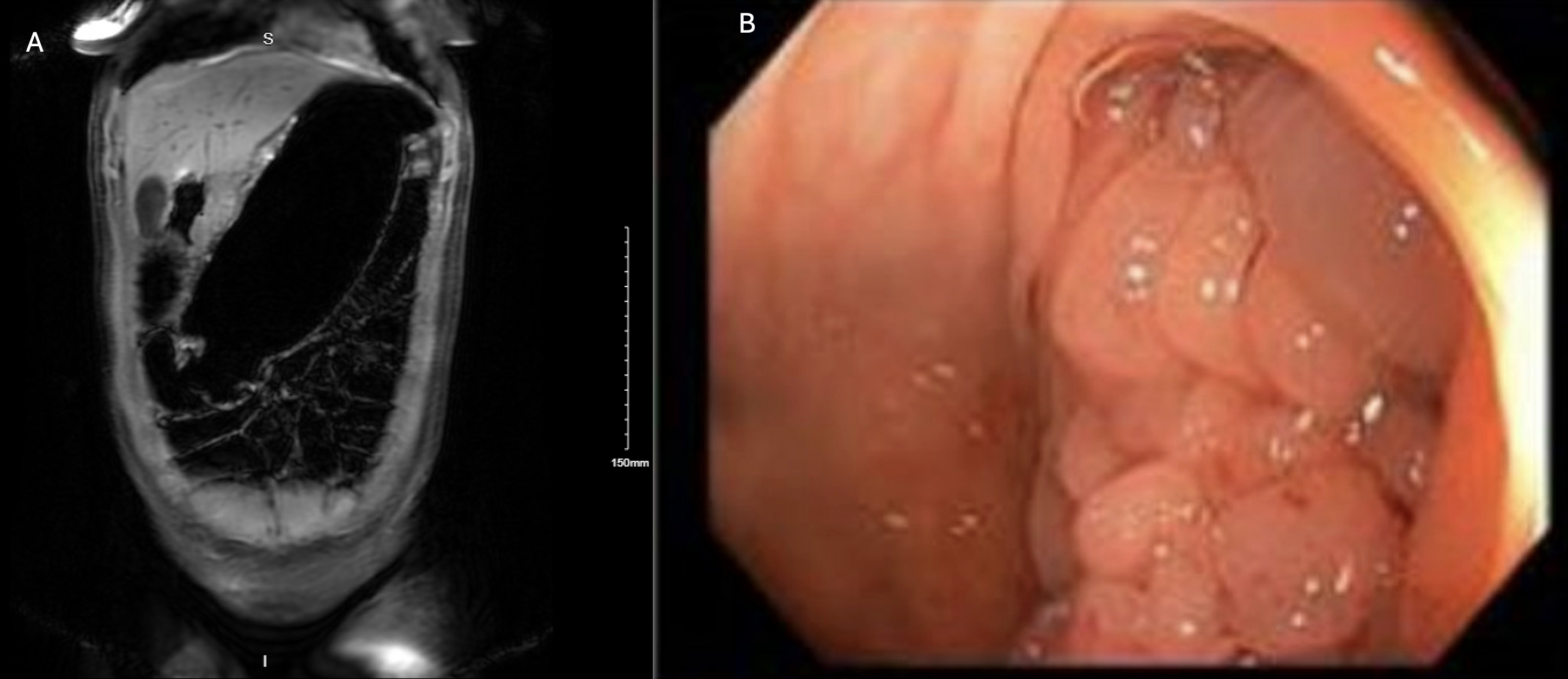
Figure: Figure 1: A) MR enterography showing descending colon stricture and upstream dilation. B) Colonoscopic image at 45 cm: edematous, bulbous, congested tissue.
Disclosures:
Ishan Antony indicated no relevant financial relationships.
Samantha Zullow: Johnson & Johnson – Advisory Committee/Board Member.
Ishan Antony, MD1, Samantha Zullow, MD2. P5544 - Signet-Ring Cell Carcinoma Masquerading as Crohn’s Disease: A Diagnostic Challenge in a Young Woman With Colonic Strictures and Ascites, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
