Tuesday Poster Session
Category: IBD
P5537 - Isolated Jejunal Stenosis as a Rare Presentation of Crohn’s Disease in the Setting of Latent Tuberculosis Infection
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sarah Herrera Mercedes, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Sarah Herrera Mercedes, MD, Jessica Strzepka, MD, Atsushi Sakuraba, MD, PhD, Dauris Rosario, MD
Rush University Medical Center, Chicago, IL
Introduction: Of the many possible etiologies of intestinal strictures, one of the most common in North America is Crohn’s Disease (CD). Isolated jejunal strictures are a rare presentation of CD in around 1% of cases. Ruling out alternate etiologies such as infections (including tuberculosis (TB)), ischemia, among others, is essential. We present a rare case of CD as an isolated jejunal stricture in the setting of untreated latent TB infection (LTBI).
Case Description/
Methods: A 62-year-old female, presented with a three-month history of abdominal pain, nausea, vomiting and weight loss. She was hemodynamically stable. Laboratory values were significant for leukocytosis at 12K/uL elevated C-reactive protein at 8mg/L, normal lactate and a positive QuantiFERON gold TB test. CT angiography revealed left lower quadrant enteritis and patent abdominal vasculature. Upper endoscopy and colonoscopy were unremarkable. Single balloon enteroscopy revealed deep ulcerations in the mid-jejunum with severe intrinsic stenosis. Biopsies showed mildly active enteritis and ulceration, and was negative for granulomas or acid-fast bacilli, and mycobacterium TB polymerase chain reaction testing. Chest imaging was normal.
A 6-month course of 300mg isoniazid daily was initiated for LTBI. After two weeks, prednisone taper was initiated at 40mg. After four weeks, 300mg vedolizumab (VDZ) was started at 0, 2 and 6 weeks then every 8 weeks, later increased to every 4 weeks. C-reactive protein was 5.7mg/L at 3 months and 2.9mg/L at 8 months. Repeat enteroscopy was completed at 16 months and showed mild jejunal narrowing, pale mucosa and previous scarring, otherwise normal mucosa. Additionally, pathology showed focal erosion but otherwise normal mucosa.
Discussion: This case highlights the diagnostic and management complexities of an isolated jejunal stricture diagnosed as CD and untreated LTBI. Active TB was ruled out, followed by initiation of LTBI therapy prior to immunosuppression (IS). Despite nonspecific histologic findings, ruling out of alternate etiologies determined CD diagnosis. CD is further supported by adequate treatment response. Guidelines recommend LTBI treatment before IS, exact time course recommendations are limited. In our case, steroids were initiated after two weeks and VDZ was initiated after 4 weeks of LTBI therapy. VDZ was chosen over anti-Tumor Necrosis Factor therapy to minimize LTBI reactivation risk. We emphasize the importance of personalized treatment regimens and careful consideration of risks and benefits.
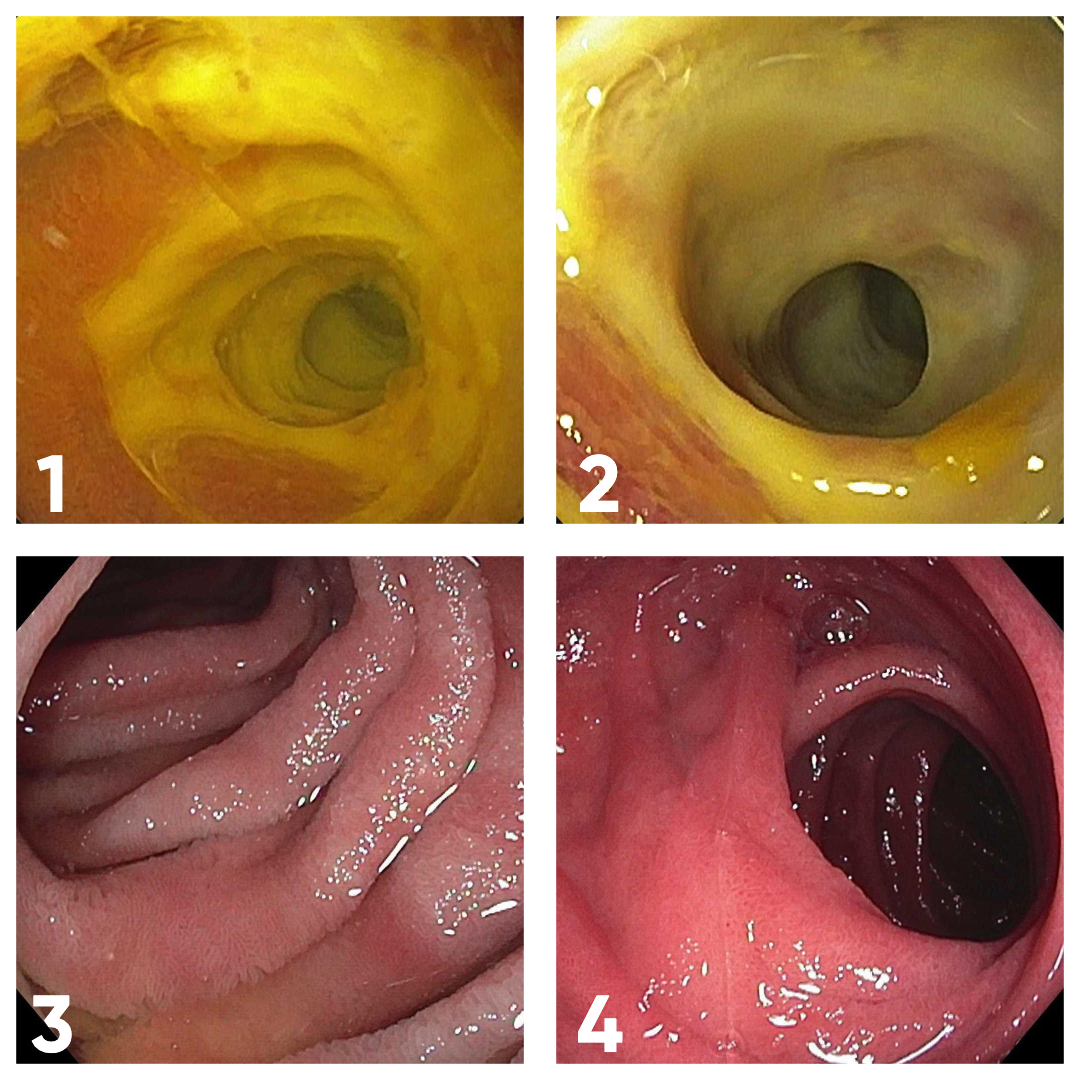
Figure: Images 1-2: Circumferential, deep confluent ulceration in the mid-jejunum causing a severe intrinsic stenosis.
Images 3-4: Mild jejunal narrowing with pale mucosa and previous scarring.
Disclosures:
Sarah Herrera Mercedes indicated no relevant financial relationships.
Jessica Strzepka indicated no relevant financial relationships.
Atsushi Sakuraba indicated no relevant financial relationships.
Dauris Rosario indicated no relevant financial relationships.
Sarah Herrera Mercedes, MD, Jessica Strzepka, MD, Atsushi Sakuraba, MD, PhD, Dauris Rosario, MD. P5537 - Isolated Jejunal Stenosis as a Rare Presentation of Crohn’s Disease in the Setting of Latent Tuberculosis Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Rush University Medical Center, Chicago, IL
Introduction: Of the many possible etiologies of intestinal strictures, one of the most common in North America is Crohn’s Disease (CD). Isolated jejunal strictures are a rare presentation of CD in around 1% of cases. Ruling out alternate etiologies such as infections (including tuberculosis (TB)), ischemia, among others, is essential. We present a rare case of CD as an isolated jejunal stricture in the setting of untreated latent TB infection (LTBI).
Case Description/
Methods: A 62-year-old female, presented with a three-month history of abdominal pain, nausea, vomiting and weight loss. She was hemodynamically stable. Laboratory values were significant for leukocytosis at 12K/uL elevated C-reactive protein at 8mg/L, normal lactate and a positive QuantiFERON gold TB test. CT angiography revealed left lower quadrant enteritis and patent abdominal vasculature. Upper endoscopy and colonoscopy were unremarkable. Single balloon enteroscopy revealed deep ulcerations in the mid-jejunum with severe intrinsic stenosis. Biopsies showed mildly active enteritis and ulceration, and was negative for granulomas or acid-fast bacilli, and mycobacterium TB polymerase chain reaction testing. Chest imaging was normal.
A 6-month course of 300mg isoniazid daily was initiated for LTBI. After two weeks, prednisone taper was initiated at 40mg. After four weeks, 300mg vedolizumab (VDZ) was started at 0, 2 and 6 weeks then every 8 weeks, later increased to every 4 weeks. C-reactive protein was 5.7mg/L at 3 months and 2.9mg/L at 8 months. Repeat enteroscopy was completed at 16 months and showed mild jejunal narrowing, pale mucosa and previous scarring, otherwise normal mucosa. Additionally, pathology showed focal erosion but otherwise normal mucosa.
Discussion: This case highlights the diagnostic and management complexities of an isolated jejunal stricture diagnosed as CD and untreated LTBI. Active TB was ruled out, followed by initiation of LTBI therapy prior to immunosuppression (IS). Despite nonspecific histologic findings, ruling out of alternate etiologies determined CD diagnosis. CD is further supported by adequate treatment response. Guidelines recommend LTBI treatment before IS, exact time course recommendations are limited. In our case, steroids were initiated after two weeks and VDZ was initiated after 4 weeks of LTBI therapy. VDZ was chosen over anti-Tumor Necrosis Factor therapy to minimize LTBI reactivation risk. We emphasize the importance of personalized treatment regimens and careful consideration of risks and benefits.
Figure: Images 1-2: Circumferential, deep confluent ulceration in the mid-jejunum causing a severe intrinsic stenosis.
Images 3-4: Mild jejunal narrowing with pale mucosa and previous scarring.
Disclosures:
Sarah Herrera Mercedes indicated no relevant financial relationships.
Jessica Strzepka indicated no relevant financial relationships.
Atsushi Sakuraba indicated no relevant financial relationships.
Dauris Rosario indicated no relevant financial relationships.
Sarah Herrera Mercedes, MD, Jessica Strzepka, MD, Atsushi Sakuraba, MD, PhD, Dauris Rosario, MD. P5537 - Isolated Jejunal Stenosis as a Rare Presentation of Crohn’s Disease in the Setting of Latent Tuberculosis Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
