Tuesday Poster Session
Category: IBD
P5528 - Schistosomiasis or Ulcerative Colitis? Unraveling the Overlap Between Parasitic Infection and IBD
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Dimo Dimitrov, MD
St. Elizabeth's Medical Center, Boston University School of Medicine
Boston, MA
Presenting Author(s)
Dimo Dimitrov, MD, Hind El Naamani, MD, Narisara Tribuddharat, MD, Sandeep Krishnan, MBBS, PhD, Jorge Fleisher, MD
St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA
Introduction: The hygiene hypothesis suggests that limited early-life exposure to microbes and parasites in modern, sanitized environments may increase the risk of inflammatory bowel disease (IBD). Helminth infections and IBD can coexist and often resemble each other, with parasites mimicking flares or emerging after immunosuppressive therapy. Misdiagnosing can lead to inappropriate treatment, sometimes with severe or even fatal consequences.
Case Description/
Methods: We present the case of a 34-year-old Brazilian with no medical history who initially presented with one month of blood-tinged stools, mild rectal pain, and nausea. Colonoscopy showed proctosigmoid colitis (Mayo 2), with biopsies revealing surface ulcerations, crypt abscesses, and eosinophilic microabscesses, raising suspicion for IBD. He was started on mesalamine and prednisone. A month later, he returned with fever, hematochezia, and severe abdominal pain, unaware that a parasite ova/larvae had been noted on histology. Steroids were stopped, and a parasitic workup was initiated. Ivermectin was given empirically for suspected Strongyloides however, symptoms continued, prompting steroid reinitiation. Serology later confirmed Schistosoma infection, treated with praziquantel and albendazole, leading to improvement while still on steroids.
Discussion: This case highlights the importance of considering parasitic infections in the differential diagnosis of IBD, particularly in patients from endemic regions. The patient’s symptoms and endoscopic findings of proctosigmoid colitis led to empiric IBD treatment. Histology supported IBD by revealing crypt abscesses and eosinophilic microabscesses, however, it also unexpectedly showed parasite larvae/ova. Immunosuppression with prednisone in the setting of undiagnosed parasitic infection posed a risk of severe complications, such as Strongyloides hyperinfection or exacerbation of schistosomiasis-related inflammation, possibly avoided due to poor steroid adherence by the patient. Symptom improvement following praziquantel and albendazole may reflect parasite clearance, but concurrent steroid use makes it unclear whether recovery was due to anti-parasitic therapy, immunosuppression, or both. The case underscores the need for timely communication of pathology findings, as delays can impact outcomes. It also illustrates the clinical and histologic overlap between helminth infections and IBD, the risk of misdiagnosis, and the need for detailed history-taking and targeted parasitic workup in high-risk patients.
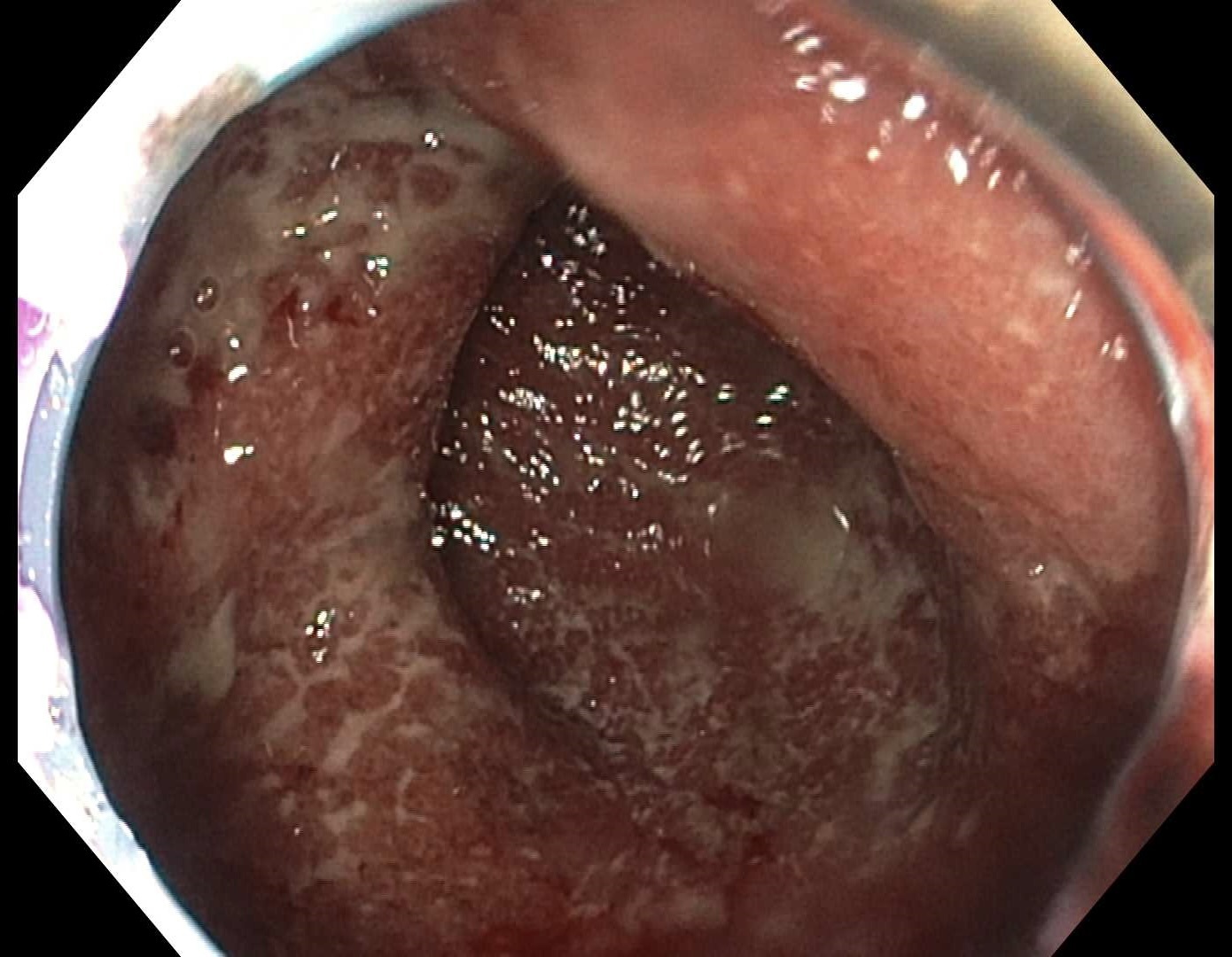
Figure: Figure 1. Endoscopic image of the rectum showing continuous moderate inflammation consistent with ulcerative colitis, with loss of vascular pattern, erythema, friability, and superficial ulcerations (Mayo 2).

Figure: Figure 2. Left colon biopsy: Colonic mucosa with increased lamina propria eosinophils, eosinophilic microabscess, and parasite ova/larva.
Disclosures:
Dimo Dimitrov indicated no relevant financial relationships.
Hind El Naamani indicated no relevant financial relationships.
Narisara Tribuddharat indicated no relevant financial relationships.
Sandeep Krishnan indicated no relevant financial relationships.
Jorge Fleisher indicated no relevant financial relationships.
Dimo Dimitrov, MD, Hind El Naamani, MD, Narisara Tribuddharat, MD, Sandeep Krishnan, MBBS, PhD, Jorge Fleisher, MD. P5528 - Schistosomiasis or Ulcerative Colitis? Unraveling the Overlap Between Parasitic Infection and IBD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA
Introduction: The hygiene hypothesis suggests that limited early-life exposure to microbes and parasites in modern, sanitized environments may increase the risk of inflammatory bowel disease (IBD). Helminth infections and IBD can coexist and often resemble each other, with parasites mimicking flares or emerging after immunosuppressive therapy. Misdiagnosing can lead to inappropriate treatment, sometimes with severe or even fatal consequences.
Case Description/
Methods: We present the case of a 34-year-old Brazilian with no medical history who initially presented with one month of blood-tinged stools, mild rectal pain, and nausea. Colonoscopy showed proctosigmoid colitis (Mayo 2), with biopsies revealing surface ulcerations, crypt abscesses, and eosinophilic microabscesses, raising suspicion for IBD. He was started on mesalamine and prednisone. A month later, he returned with fever, hematochezia, and severe abdominal pain, unaware that a parasite ova/larvae had been noted on histology. Steroids were stopped, and a parasitic workup was initiated. Ivermectin was given empirically for suspected Strongyloides however, symptoms continued, prompting steroid reinitiation. Serology later confirmed Schistosoma infection, treated with praziquantel and albendazole, leading to improvement while still on steroids.
Discussion: This case highlights the importance of considering parasitic infections in the differential diagnosis of IBD, particularly in patients from endemic regions. The patient’s symptoms and endoscopic findings of proctosigmoid colitis led to empiric IBD treatment. Histology supported IBD by revealing crypt abscesses and eosinophilic microabscesses, however, it also unexpectedly showed parasite larvae/ova. Immunosuppression with prednisone in the setting of undiagnosed parasitic infection posed a risk of severe complications, such as Strongyloides hyperinfection or exacerbation of schistosomiasis-related inflammation, possibly avoided due to poor steroid adherence by the patient. Symptom improvement following praziquantel and albendazole may reflect parasite clearance, but concurrent steroid use makes it unclear whether recovery was due to anti-parasitic therapy, immunosuppression, or both. The case underscores the need for timely communication of pathology findings, as delays can impact outcomes. It also illustrates the clinical and histologic overlap between helminth infections and IBD, the risk of misdiagnosis, and the need for detailed history-taking and targeted parasitic workup in high-risk patients.
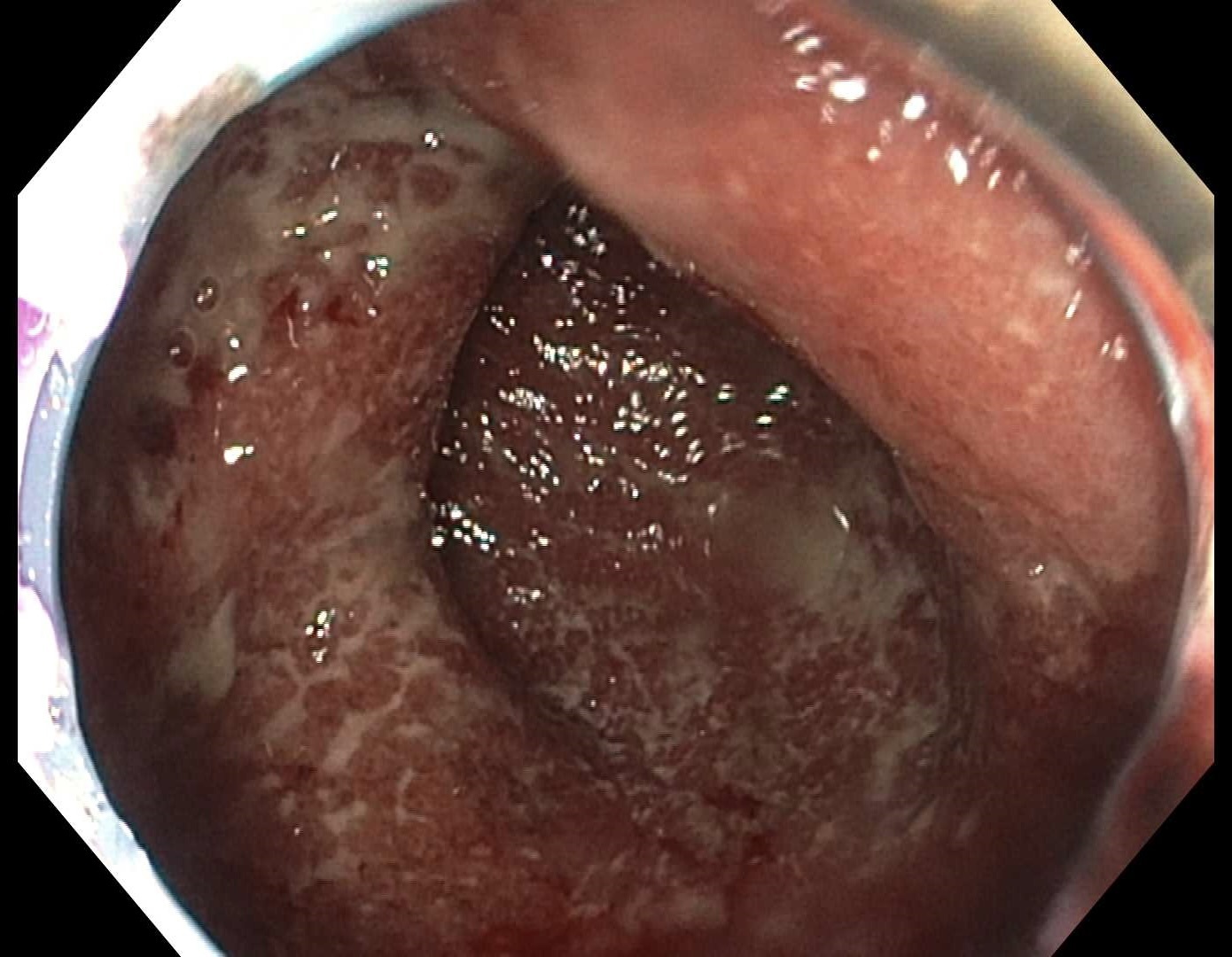
Figure: Figure 1. Endoscopic image of the rectum showing continuous moderate inflammation consistent with ulcerative colitis, with loss of vascular pattern, erythema, friability, and superficial ulcerations (Mayo 2).

Figure: Figure 2. Left colon biopsy: Colonic mucosa with increased lamina propria eosinophils, eosinophilic microabscess, and parasite ova/larva.
Disclosures:
Dimo Dimitrov indicated no relevant financial relationships.
Hind El Naamani indicated no relevant financial relationships.
Narisara Tribuddharat indicated no relevant financial relationships.
Sandeep Krishnan indicated no relevant financial relationships.
Jorge Fleisher indicated no relevant financial relationships.
Dimo Dimitrov, MD, Hind El Naamani, MD, Narisara Tribuddharat, MD, Sandeep Krishnan, MBBS, PhD, Jorge Fleisher, MD. P5528 - Schistosomiasis or Ulcerative Colitis? Unraveling the Overlap Between Parasitic Infection and IBD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
