Tuesday Poster Session
Category: IBD
P5522 - Vedolizumab-Induced Remission in Adult-Onset Autoimmune Enteropathy Complicated by Fibrotic Stricture
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Isaac Giovannie, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Award: ACG Presidential Poster Award
Giovannie Isaac-Coss, MD1, Zoe Post, MD, MSc1, Aryanna Sousa, MD1, Shriram Jakate, MD1, Joseph Frasca, MD1, Ali Keshavarzian, MD, MACG2
1Rush University Medical Center, Chicago, IL; 2Rush University Medical Center; Rush Center for Integrated Microbiome and Chronobiology Research, Chicago, IL
Introduction: Autoimmune enteropathy (AIE) is a rare immune-mediated disorder marked by chronic diarrhea and malabsorption, most commonly described in children but increasingly recognized in adults. Adult-onset AIE presents diagnostic challenges due to overlap with celiac disease, inflammatory bowel disease, and infectious enteritis. We report a rare case of adult-onset AIE in a 74-year-old woman, highlighting its diagnostic complexity and the therapeutic success of vedolizumab in sustaining remission.
Case Description/
Methods: A 74-year-old woman with migraines, HTN, and allergies presented with six weeks of nausea, vomiting, and profuse diarrhea following travel. Initial evaluation suggested gastroenteritis, but symptoms persisted. EGD revealed diffuse granular mucosa; colonoscopy showed terminal ileal cobblestoning and exudates. Duodenal and ileal biopsies demonstrated patchy chronic enteritis with crypt loss, cryptitis, regenerative changes, and increased lamina propria inflammation, without granulomas or intraepithelial lymphocytosis—findings favoring AIE over celiac or Crohn’s disease. Infectious workup was negative; celiac serologies, ANA, and anti-enterocyte antibodies were normal. Elevated fecal calprotectin and CRP indicated active inflammation. The patient improved on corticosteroids but developed steroid dependence, prompting vedolizumab initiation, which normalized inflammatory markers and induced histologic remission. Weeks later, she was readmitted with intractable vomiting and was found to have small bowel obstruction. After nasogastric decompression and discharge, outpatient EGD, colonoscopy, and VCE were performed. Capsule retention due to a fibrotic stricture required surgical resection. Pathology showed chronic active enteritis with villous blunting, cryptitis, crypt abscesses, increased apoptosis, and reduced goblet and Paneth cells, without granulomas or malignancy, consistent with AIE. She remains clinically stable on vedolizumab, with normal calprotectin and no disease recurrence.
Discussion: Adult-onset AIE remains underrecognized. Diagnosis requires integration of clinical symptoms, characteristic histology, exclusion of mimics, and therapeutic response. Although anti-enterocyte antibodies may support diagnosis, they are often absent in adults. This case demonstrates vedolizumab’s efficacy in steroid-refractory AIE and suggests that chronic subclinical inflammation may result in irreversible structural complications. Early diagnosis and long-term surveillance are essential.
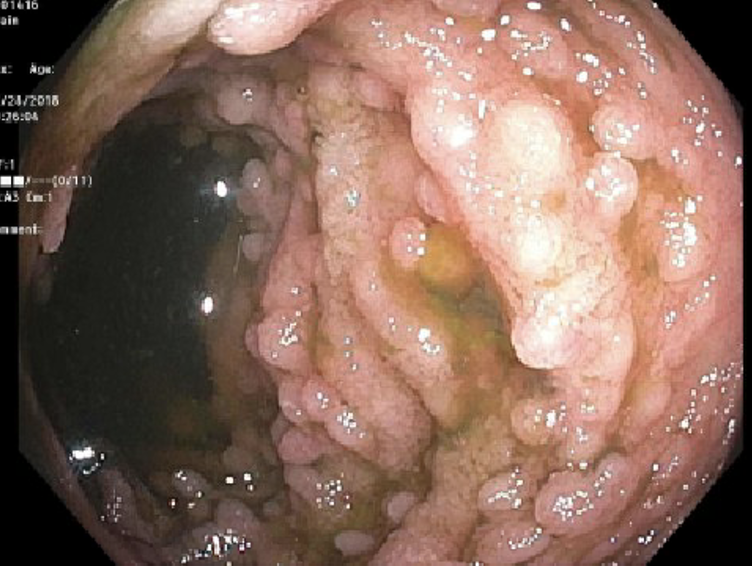
Figure: Image 1: Colonoscopy showing cobblestoning, granularity, whitish exudates and lymphoid nodules in the terminal ileum, suspicious for autoimmune enteritis
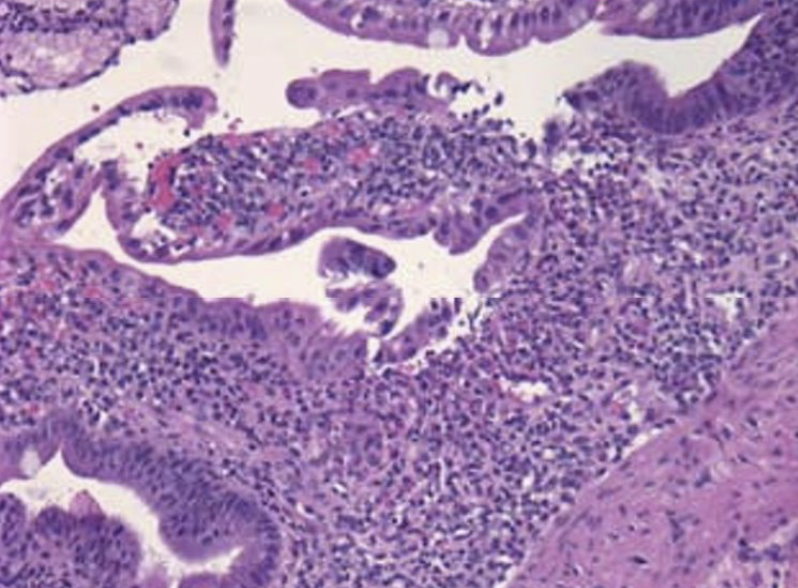
Figure: Image 2: Duodenal mucosa showing severe chronic duodenitis with marked increase in chronic inflammatory cells is the duodenal mucosa (H & E stain, x 200 magnification).
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Zoe Post indicated no relevant financial relationships.
Aryanna Sousa indicated no relevant financial relationships.
Shriram Jakate indicated no relevant financial relationships.
Joseph Frasca indicated no relevant financial relationships.
Ali Keshavarzian indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Zoe Post, MD, MSc1, Aryanna Sousa, MD1, Shriram Jakate, MD1, Joseph Frasca, MD1, Ali Keshavarzian, MD, MACG2. P5522 - Vedolizumab-Induced Remission in Adult-Onset Autoimmune Enteropathy Complicated by Fibrotic Stricture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Giovannie Isaac-Coss, MD1, Zoe Post, MD, MSc1, Aryanna Sousa, MD1, Shriram Jakate, MD1, Joseph Frasca, MD1, Ali Keshavarzian, MD, MACG2
1Rush University Medical Center, Chicago, IL; 2Rush University Medical Center; Rush Center for Integrated Microbiome and Chronobiology Research, Chicago, IL
Introduction: Autoimmune enteropathy (AIE) is a rare immune-mediated disorder marked by chronic diarrhea and malabsorption, most commonly described in children but increasingly recognized in adults. Adult-onset AIE presents diagnostic challenges due to overlap with celiac disease, inflammatory bowel disease, and infectious enteritis. We report a rare case of adult-onset AIE in a 74-year-old woman, highlighting its diagnostic complexity and the therapeutic success of vedolizumab in sustaining remission.
Case Description/
Methods: A 74-year-old woman with migraines, HTN, and allergies presented with six weeks of nausea, vomiting, and profuse diarrhea following travel. Initial evaluation suggested gastroenteritis, but symptoms persisted. EGD revealed diffuse granular mucosa; colonoscopy showed terminal ileal cobblestoning and exudates. Duodenal and ileal biopsies demonstrated patchy chronic enteritis with crypt loss, cryptitis, regenerative changes, and increased lamina propria inflammation, without granulomas or intraepithelial lymphocytosis—findings favoring AIE over celiac or Crohn’s disease. Infectious workup was negative; celiac serologies, ANA, and anti-enterocyte antibodies were normal. Elevated fecal calprotectin and CRP indicated active inflammation. The patient improved on corticosteroids but developed steroid dependence, prompting vedolizumab initiation, which normalized inflammatory markers and induced histologic remission. Weeks later, she was readmitted with intractable vomiting and was found to have small bowel obstruction. After nasogastric decompression and discharge, outpatient EGD, colonoscopy, and VCE were performed. Capsule retention due to a fibrotic stricture required surgical resection. Pathology showed chronic active enteritis with villous blunting, cryptitis, crypt abscesses, increased apoptosis, and reduced goblet and Paneth cells, without granulomas or malignancy, consistent with AIE. She remains clinically stable on vedolizumab, with normal calprotectin and no disease recurrence.
Discussion: Adult-onset AIE remains underrecognized. Diagnosis requires integration of clinical symptoms, characteristic histology, exclusion of mimics, and therapeutic response. Although anti-enterocyte antibodies may support diagnosis, they are often absent in adults. This case demonstrates vedolizumab’s efficacy in steroid-refractory AIE and suggests that chronic subclinical inflammation may result in irreversible structural complications. Early diagnosis and long-term surveillance are essential.
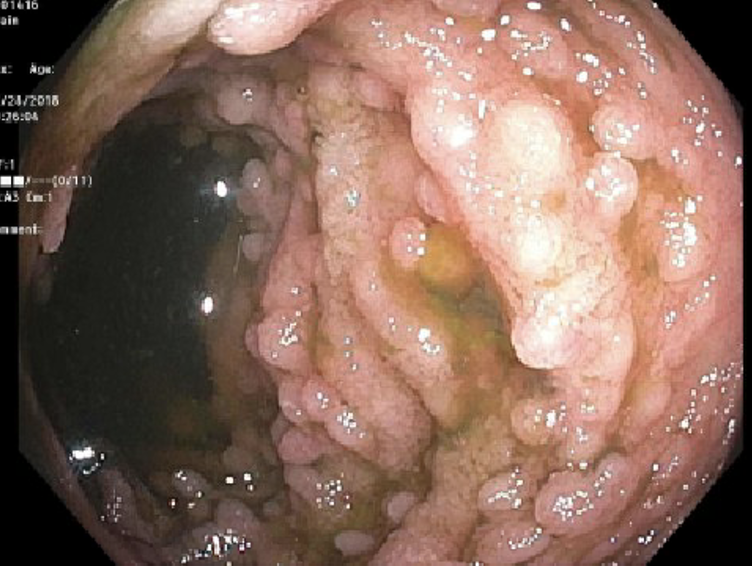
Figure: Image 1: Colonoscopy showing cobblestoning, granularity, whitish exudates and lymphoid nodules in the terminal ileum, suspicious for autoimmune enteritis
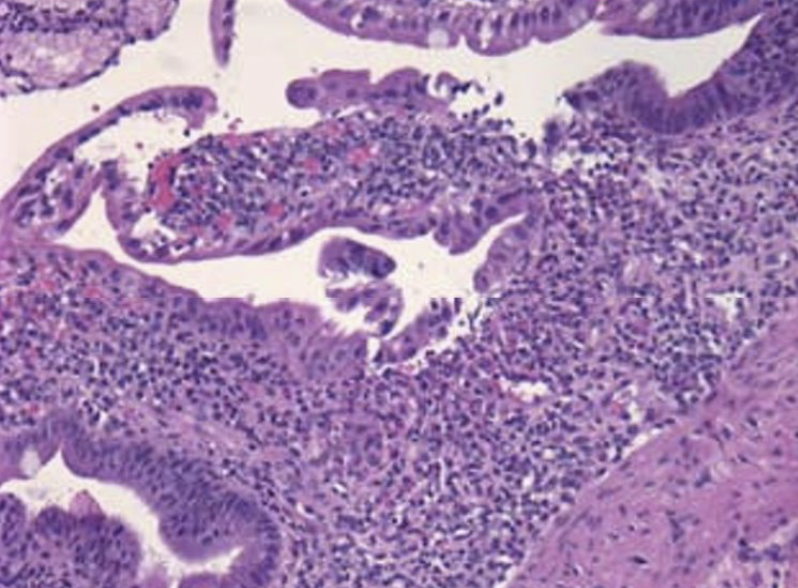
Figure: Image 2: Duodenal mucosa showing severe chronic duodenitis with marked increase in chronic inflammatory cells is the duodenal mucosa (H & E stain, x 200 magnification).
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Zoe Post indicated no relevant financial relationships.
Aryanna Sousa indicated no relevant financial relationships.
Shriram Jakate indicated no relevant financial relationships.
Joseph Frasca indicated no relevant financial relationships.
Ali Keshavarzian indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Zoe Post, MD, MSc1, Aryanna Sousa, MD1, Shriram Jakate, MD1, Joseph Frasca, MD1, Ali Keshavarzian, MD, MACG2. P5522 - Vedolizumab-Induced Remission in Adult-Onset Autoimmune Enteropathy Complicated by Fibrotic Stricture, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

