Tuesday Poster Session
Category: IBD
P5521 - Biologic-Refractory GI Behçet’s Disease Requiring Hemicolectomy: An 8-Year Follow-Up Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Isaac Giovannie, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Award: ACG Presidential Poster Award
Giovannie Isaac-Coss, MD1, Zoe Post, MD, MSc1, Aryanna Sousa, MD1, Aje T. Kent, MD1, Shriram Jakate, MD1, Ali Keshavarzian, MD, MACG2
1Rush University Medical Center, Chicago, IL; 2Rush University Medical Center; Rush Center for Integrated Microbiome and Chronobiology Research, Chicago, IL
Introduction: Behçet’s disease is a multisystem vasculitis marked by recurrent mucocutaneous, ocular, and systemic involvement. Gastrointestinal (GI) manifestations are uncommon, affecting 3–16% of patients, and often mimic inflammatory bowel disease (IBD), especially Crohn’s disease.Differentiating GI Behçet’s from Crohn’s is challenging due to overlapping clinical and histologic features. Severe, refractory GI Behçet’s requiring surgery and multiple biologics is rare and presents significant management challenges.
Case Description/
Methods: A 56-year-old woman with recurrent oral and vaginal ulcers was hospitalized with abdominal pain and diarrhea. Fecal calprotectin was 665 mcg/g (ref < 163); stool studies were negative. Colonoscopy revealed severe right-sided colitis. Biopsies showed deep ulcerations with eosinophilia and no granulomas, favoring Behçet’s disease (Image 1). She was started on adalimumab (ADA) and prednisone, with partial improvement. Despite weekly ADA and colchicine, she remained steroid-dependent with persistent ischemic-appearing ulcers. Due to concern for perforation, she underwent right hemicolectomy. Pathology showed discrete ulcers with perivascular lymphoid infiltrates and no granulomas—consistent with Behçet’s colitis. Postoperatively, she remained on ADA with clinical and endoscopic remission for four years. She later relapsed despite a therapeutic ADA level and no anti-drug antibodies. She required escalation to infliximab, risankizumab, certolizumab pegol, and most recently is set to start guselkumab. Despite sequential biologics, she continues to have active disease (Image 2) and was referred to colorectal surgery.
Discussion: This case highlights the therapeutic challenges of GI Behçet’s, especially in biologic-refractory disease. Histologic features—deep ulcers without granulomas, perivascular inflammation, and absence of transmural lymphoid aggregates—help differentiate Behçet’s from Crohn’s. Anti-TNF agents, particularly infliximab and adalimumab, are first-line therapies and remain the most effective biologics for GI involvement. However, sustained remission is often elusive. Limited data on alternative biologics suggest lower response rates. This patient’s relapse despite multiple biologics reflects a truly refractory phenotype.Early recognition, multidisciplinary care, and individualized strategies are essential. Further research is needed to identify predictors of response, determine the most effective biologics, and define the role of surgery in refractory GI Behçet’s.
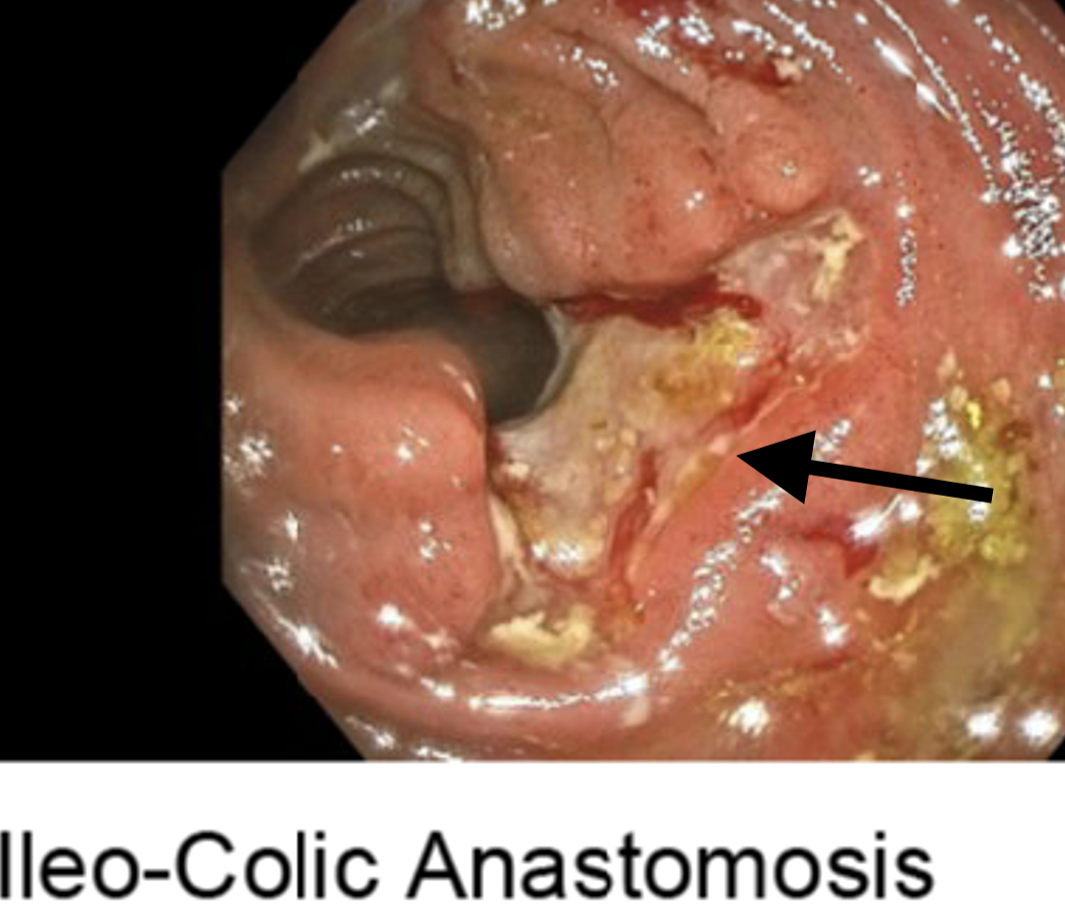
Figure: Image 1: Active ileal Behcet with deep ischemic appearing ulcers (black arrow) starting at the anastomotic ring and extending to 5 cm proximal to the anastomotic ring, wide open side to side ileocolonic anastomosis.
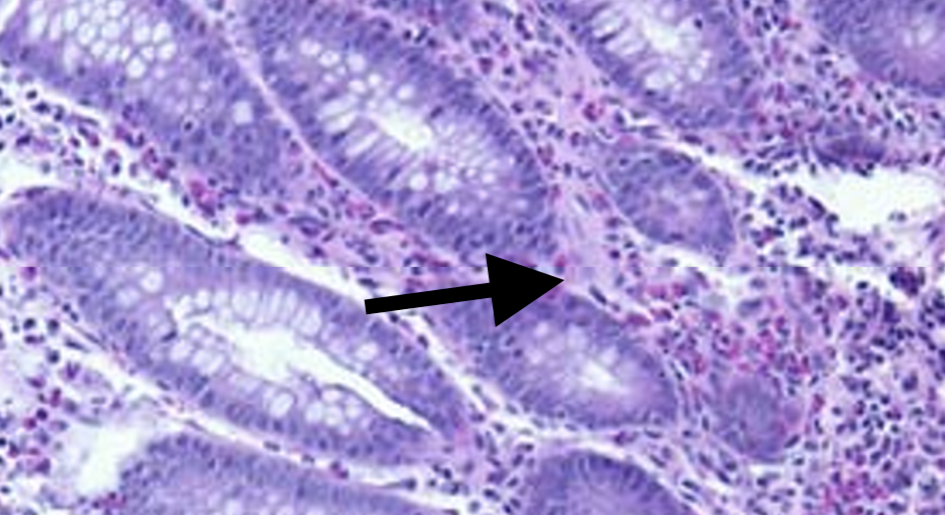
Figure: Image 2: Colonic mucosa showing patchy chronic colitis with focally increased eosinophils (H & E stain, x 400 magnification).
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Zoe Post indicated no relevant financial relationships.
Aryanna Sousa indicated no relevant financial relationships.
Aje Kent indicated no relevant financial relationships.
Shriram Jakate indicated no relevant financial relationships.
Ali Keshavarzian indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Zoe Post, MD, MSc1, Aryanna Sousa, MD1, Aje T. Kent, MD1, Shriram Jakate, MD1, Ali Keshavarzian, MD, MACG2. P5521 - Biologic-Refractory GI Behçet’s Disease Requiring Hemicolectomy: An 8-Year Follow-Up Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Giovannie Isaac-Coss, MD1, Zoe Post, MD, MSc1, Aryanna Sousa, MD1, Aje T. Kent, MD1, Shriram Jakate, MD1, Ali Keshavarzian, MD, MACG2
1Rush University Medical Center, Chicago, IL; 2Rush University Medical Center; Rush Center for Integrated Microbiome and Chronobiology Research, Chicago, IL
Introduction: Behçet’s disease is a multisystem vasculitis marked by recurrent mucocutaneous, ocular, and systemic involvement. Gastrointestinal (GI) manifestations are uncommon, affecting 3–16% of patients, and often mimic inflammatory bowel disease (IBD), especially Crohn’s disease.Differentiating GI Behçet’s from Crohn’s is challenging due to overlapping clinical and histologic features. Severe, refractory GI Behçet’s requiring surgery and multiple biologics is rare and presents significant management challenges.
Case Description/
Methods: A 56-year-old woman with recurrent oral and vaginal ulcers was hospitalized with abdominal pain and diarrhea. Fecal calprotectin was 665 mcg/g (ref < 163); stool studies were negative. Colonoscopy revealed severe right-sided colitis. Biopsies showed deep ulcerations with eosinophilia and no granulomas, favoring Behçet’s disease (Image 1). She was started on adalimumab (ADA) and prednisone, with partial improvement. Despite weekly ADA and colchicine, she remained steroid-dependent with persistent ischemic-appearing ulcers. Due to concern for perforation, she underwent right hemicolectomy. Pathology showed discrete ulcers with perivascular lymphoid infiltrates and no granulomas—consistent with Behçet’s colitis. Postoperatively, she remained on ADA with clinical and endoscopic remission for four years. She later relapsed despite a therapeutic ADA level and no anti-drug antibodies. She required escalation to infliximab, risankizumab, certolizumab pegol, and most recently is set to start guselkumab. Despite sequential biologics, she continues to have active disease (Image 2) and was referred to colorectal surgery.
Discussion: This case highlights the therapeutic challenges of GI Behçet’s, especially in biologic-refractory disease. Histologic features—deep ulcers without granulomas, perivascular inflammation, and absence of transmural lymphoid aggregates—help differentiate Behçet’s from Crohn’s. Anti-TNF agents, particularly infliximab and adalimumab, are first-line therapies and remain the most effective biologics for GI involvement. However, sustained remission is often elusive. Limited data on alternative biologics suggest lower response rates. This patient’s relapse despite multiple biologics reflects a truly refractory phenotype.Early recognition, multidisciplinary care, and individualized strategies are essential. Further research is needed to identify predictors of response, determine the most effective biologics, and define the role of surgery in refractory GI Behçet’s.
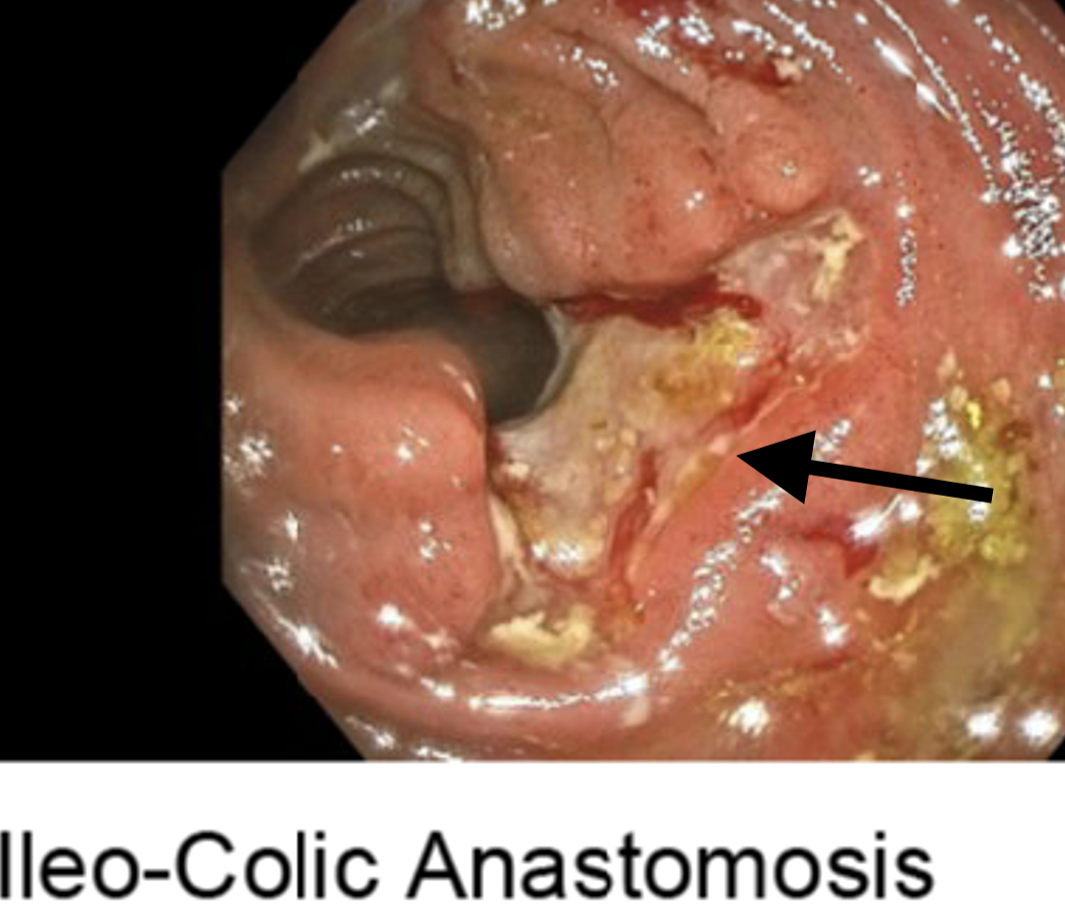
Figure: Image 1: Active ileal Behcet with deep ischemic appearing ulcers (black arrow) starting at the anastomotic ring and extending to 5 cm proximal to the anastomotic ring, wide open side to side ileocolonic anastomosis.
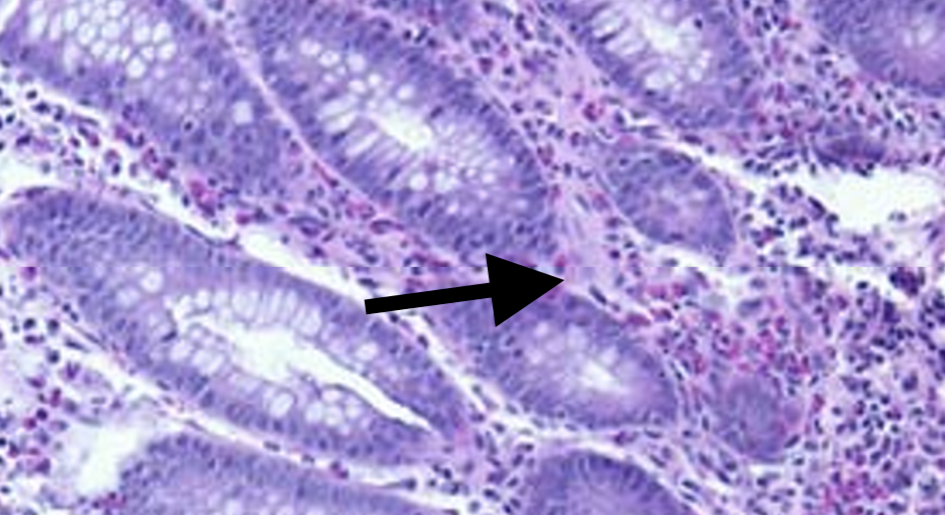
Figure: Image 2: Colonic mucosa showing patchy chronic colitis with focally increased eosinophils (H & E stain, x 400 magnification).
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Zoe Post indicated no relevant financial relationships.
Aryanna Sousa indicated no relevant financial relationships.
Aje Kent indicated no relevant financial relationships.
Shriram Jakate indicated no relevant financial relationships.
Ali Keshavarzian indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Zoe Post, MD, MSc1, Aryanna Sousa, MD1, Aje T. Kent, MD1, Shriram Jakate, MD1, Ali Keshavarzian, MD, MACG2. P5521 - Biologic-Refractory GI Behçet’s Disease Requiring Hemicolectomy: An 8-Year Follow-Up Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

