Tuesday Poster Session
Category: IBD
P5515 - An Uncommon Culprit: CMV Pouchitis Mimicking Crohn's-Like Disease of the Pouch
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Priscila Santiago, MD
University of Utah
Salt Lake City, UT
Presenting Author(s)
Priscila Santiago, MD1, Mina Awadallah, MD, MSc1, John Erikson Yap, MD, MBA2, Maria Pletneva, MD, PhD1
1University of Utah, Salt Lake City, UT; 2University of Utah School of Medicine, Salt Lake City, UT
Introduction: Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the surgical procedure of choice for patients with medically refractory ulcerative colitis (UC). Pouchitis is the most common complication after IPAA, affecting up to 48% of patients within the first 2 years. Infectious pouchitis with cytomegalovirus (CMV) has been described as a rare secondary cause of pouchitis, and its characteristics remain poorly understood. We present a rare case of CMV pouchitis in an immunosuppressed patient who is being treated for Crohn’s like disease of pouch (CLDP).
Case Description/
Methods: A 21-year-old female with medically refractory UC status post total proctocolectomy and IPAA in 2018, and CLDP in 2023, presented for a second opinion on CLDP. In 2023, she was treated with Risankizumab for CLDP with primary non-response. A pouchoscopy in 2024 showed persistent pre-pouch ulcerations, with biopsies negative for CMV. She was referred to our institution on Ustekinumab every 4 weeks and Azathioprine 125 mg daily. Clinically, she reported 10-12 bowel movements during the day, with additional 3-4 during the night, liquid consistency, with blood, urgency and constant lower abdominal pain. Denied fevers/chills.
A pouchoscopy in our institution showed erosions, erythema and shallow ulcerations in the pouch body, moderate inflammation with deep and shallow ulcerations in the pouch inlet, and patchy severe inflammation with erythema, mucus, confluent and deep ulcerations in the pre pouch ileum. The rectal cuff had ulcerations and scarring. Pathology of the pre pouch ileum showed CMV ileitis with ulcer, confirmed by immunostain. Biopsies also showed CMV in the pouch body and CMV cuffitis. Plasma CMV by quantitative nucleic acid amplification test was detected at 3.41 log IU/mL. Patient required hospitalization locally and is currently being treated with intravenous ganciclovir with improvement of symptoms.
Discussion: A high index of suspicion is needed to diagnose CMV pouchitis, especially in patients who are immunosuppressed and have not responded to conventional therapies. The symptoms and endoscopic features can be similar to idiopathic pouchitis or CLDP. However, febrile episodes and deep/large ulcers are more common with CMV. Other case reports have also shown extensive involvement of the pre pouch ileum. A repeat endoscopic exam after antiviral treatment is recommended to document mucosal healing, CMV eradication, and exclude Crohn’s disease.
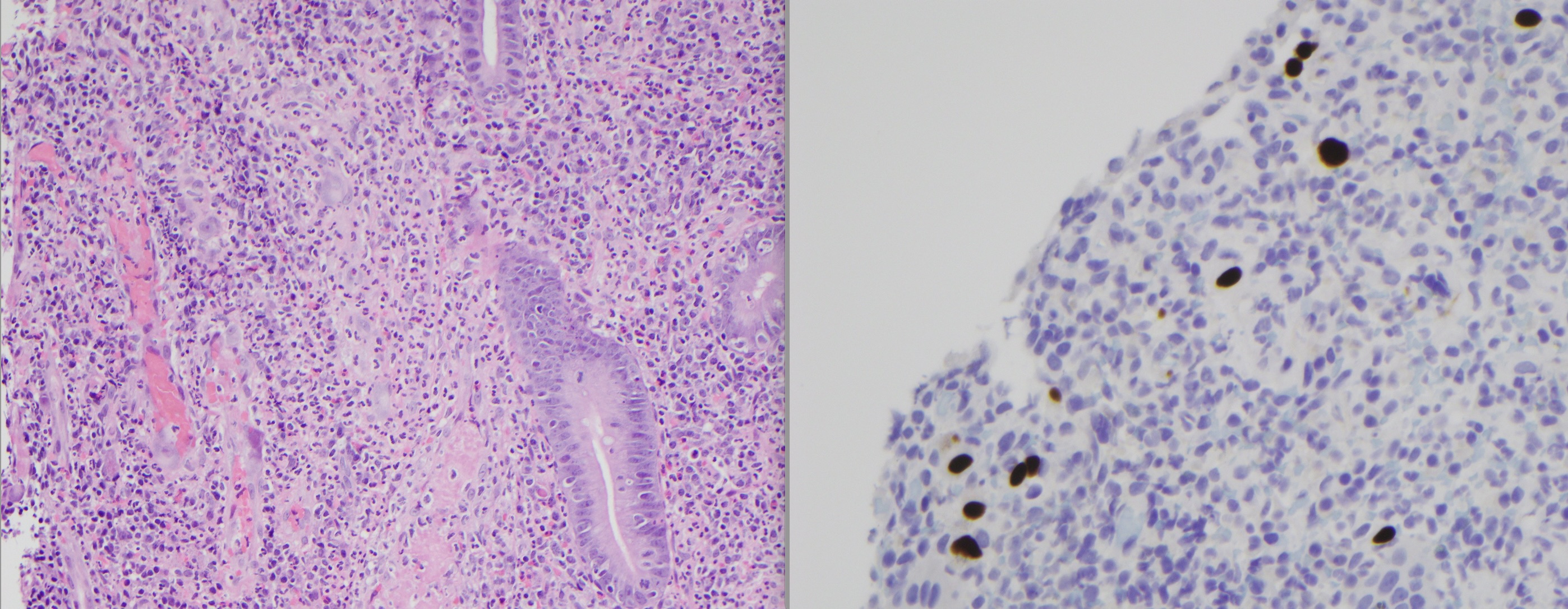
Figure: Figure 1: A, B, and C: Pouchoscopy findings of pre pouch ileum inflammation, demonstrating deep and confluent ulcerations, consistent with cytomegalovirus infection. D: Rectal cuff with ulcerations, which was also affected by cytomegalovirus infection.

Figure: Figure 2: Sections of ulcerated pre pouch ileum, with visible viral cytopathic effect within endothelial cells in H&E (40x), and positive CMV immunohistochemistry with clusters of infected cells.
Disclosures:
Priscila Santiago indicated no relevant financial relationships.
Mina Awadallah indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Maria Pletneva: Allakos – Consultant. Regeneron – Advisor or Review Panel Member.
Priscila Santiago, MD1, Mina Awadallah, MD, MSc1, John Erikson Yap, MD, MBA2, Maria Pletneva, MD, PhD1. P5515 - An Uncommon Culprit: CMV Pouchitis Mimicking Crohn's-Like Disease of the Pouch, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Utah, Salt Lake City, UT; 2University of Utah School of Medicine, Salt Lake City, UT
Introduction: Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is the surgical procedure of choice for patients with medically refractory ulcerative colitis (UC). Pouchitis is the most common complication after IPAA, affecting up to 48% of patients within the first 2 years. Infectious pouchitis with cytomegalovirus (CMV) has been described as a rare secondary cause of pouchitis, and its characteristics remain poorly understood. We present a rare case of CMV pouchitis in an immunosuppressed patient who is being treated for Crohn’s like disease of pouch (CLDP).
Case Description/
Methods: A 21-year-old female with medically refractory UC status post total proctocolectomy and IPAA in 2018, and CLDP in 2023, presented for a second opinion on CLDP. In 2023, she was treated with Risankizumab for CLDP with primary non-response. A pouchoscopy in 2024 showed persistent pre-pouch ulcerations, with biopsies negative for CMV. She was referred to our institution on Ustekinumab every 4 weeks and Azathioprine 125 mg daily. Clinically, she reported 10-12 bowel movements during the day, with additional 3-4 during the night, liquid consistency, with blood, urgency and constant lower abdominal pain. Denied fevers/chills.
A pouchoscopy in our institution showed erosions, erythema and shallow ulcerations in the pouch body, moderate inflammation with deep and shallow ulcerations in the pouch inlet, and patchy severe inflammation with erythema, mucus, confluent and deep ulcerations in the pre pouch ileum. The rectal cuff had ulcerations and scarring. Pathology of the pre pouch ileum showed CMV ileitis with ulcer, confirmed by immunostain. Biopsies also showed CMV in the pouch body and CMV cuffitis. Plasma CMV by quantitative nucleic acid amplification test was detected at 3.41 log IU/mL. Patient required hospitalization locally and is currently being treated with intravenous ganciclovir with improvement of symptoms.
Discussion: A high index of suspicion is needed to diagnose CMV pouchitis, especially in patients who are immunosuppressed and have not responded to conventional therapies. The symptoms and endoscopic features can be similar to idiopathic pouchitis or CLDP. However, febrile episodes and deep/large ulcers are more common with CMV. Other case reports have also shown extensive involvement of the pre pouch ileum. A repeat endoscopic exam after antiviral treatment is recommended to document mucosal healing, CMV eradication, and exclude Crohn’s disease.
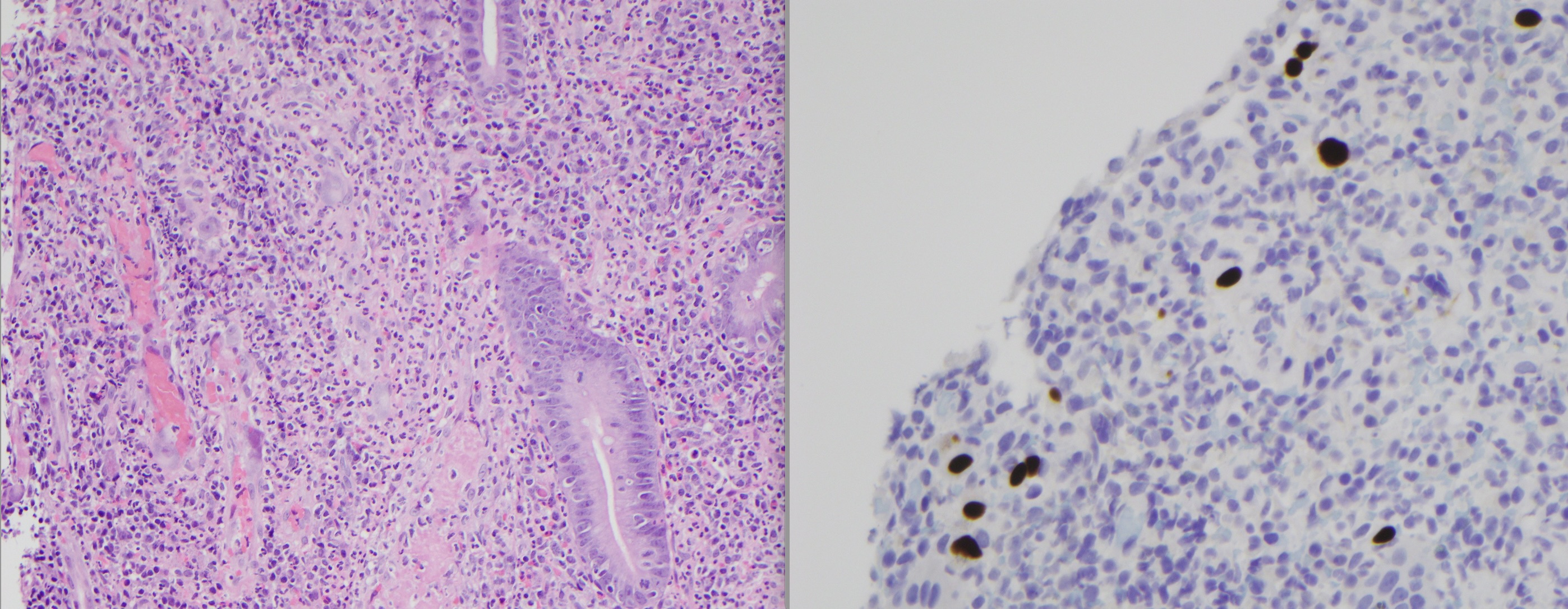
Figure: Figure 1: A, B, and C: Pouchoscopy findings of pre pouch ileum inflammation, demonstrating deep and confluent ulcerations, consistent with cytomegalovirus infection. D: Rectal cuff with ulcerations, which was also affected by cytomegalovirus infection.

Figure: Figure 2: Sections of ulcerated pre pouch ileum, with visible viral cytopathic effect within endothelial cells in H&E (40x), and positive CMV immunohistochemistry with clusters of infected cells.
Disclosures:
Priscila Santiago indicated no relevant financial relationships.
Mina Awadallah indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Maria Pletneva: Allakos – Consultant. Regeneron – Advisor or Review Panel Member.
Priscila Santiago, MD1, Mina Awadallah, MD, MSc1, John Erikson Yap, MD, MBA2, Maria Pletneva, MD, PhD1. P5515 - An Uncommon Culprit: CMV Pouchitis Mimicking Crohn's-Like Disease of the Pouch, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
