Tuesday Poster Session
Category: IBD
P5514 - Ulcerative Colitis Unmasked by a Clostridioides difficile Infection: A Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mark Shokralla, DO
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Mark Shokralla, DO
University of Texas Health San Antonio, San Antonio, TX
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease affecting over 900,000 individuals in the United States, with an annual incidence of 9–20 cases per 100,000 people. While typically diagnosed in younger adults, up to 15% of cases present after age 60. Clostridioides difficile infection (CDI) is a known trigger for colonic inflammation and may unmask underlying IBD. Differentiating post-infectious colitis from new-onset UC can be challenging. We present a case of elderly-onset UC diagnosed following persistent diarrhea after CDI, highlighting the importance of considering IBD in refractory cases.
Case Description/
Methods: A 77-year-old male with CAD (post-CABG/PCI) and type 2 diabetes presented with two months of profuse green, watery diarrhea ( >20x/day), fecal incontinence, and a 40-pound weight loss. Symptoms began after completing a 7-day course of Cefdinir. He denied GI bleeding, fever, recent travel, or sick contacts. There was no prior history of IBD, IBS, celiac disease, or pancreatitis.
He initially tested positive for C. difficile and was treated with a 2-week course of oral vancomycin, with only brief symptom improvement. Due to ongoing weight loss and persistent diarrhea, he presented to the ED. He appeared pale but was stable. Abdominal exam revealed decreased bowel sounds; labs showed iron deficiency anemia, elevated ESR (98), CRP (54), fecal calprotectin >1200, positive FIT, and normal WBC and platelets.
CT abdomen/pelvis showed diffuse colonic wall thickening from the transverse colon to the rectum, consistent with proctocolitis. A colonoscopy revealed continuous severe inflammation from the rectum to the cecum with friability, granularity, and ulcerations—most pronounced in the left colon. Biopsies showed active colitis with chronic architectural changes.
He was started on IV methylprednisolone, transitioned to a prednisone taper, and initiated on vedolizumab. He reported symptom improvement, with CRP decreasing from 54 to 13, and he was referred to the IBD clinic for ongoing care.
Discussion: Persistent diarrhea after C. difficile treatment should prompt evaluation for underlying IBD. In this case, weight loss, elevated inflammatory markers, and chronic colitis on biopsy supported new-onset ulcerative colitis. C. difficile may unmask IBD, especially in older adults with atypical symptoms. Early colonoscopy is essential when symptoms persist. The patient improved with corticosteroids and vedolizumab, aligning with standard UC therapy.
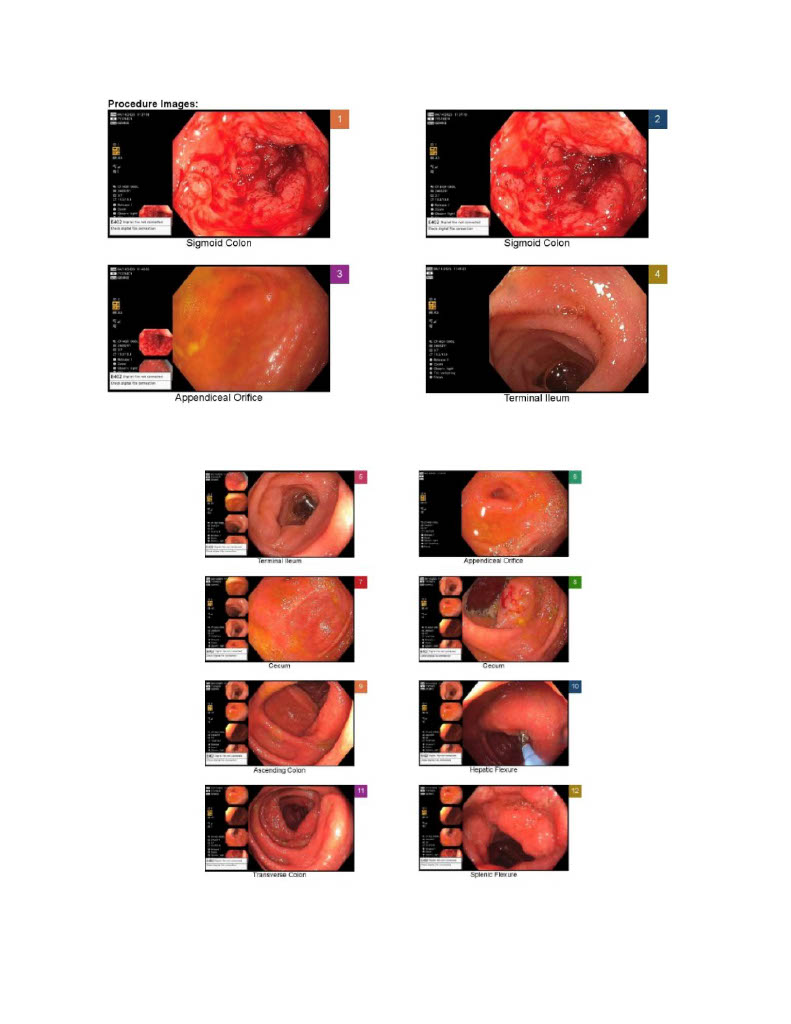
Figure: Colonoscopy images #1
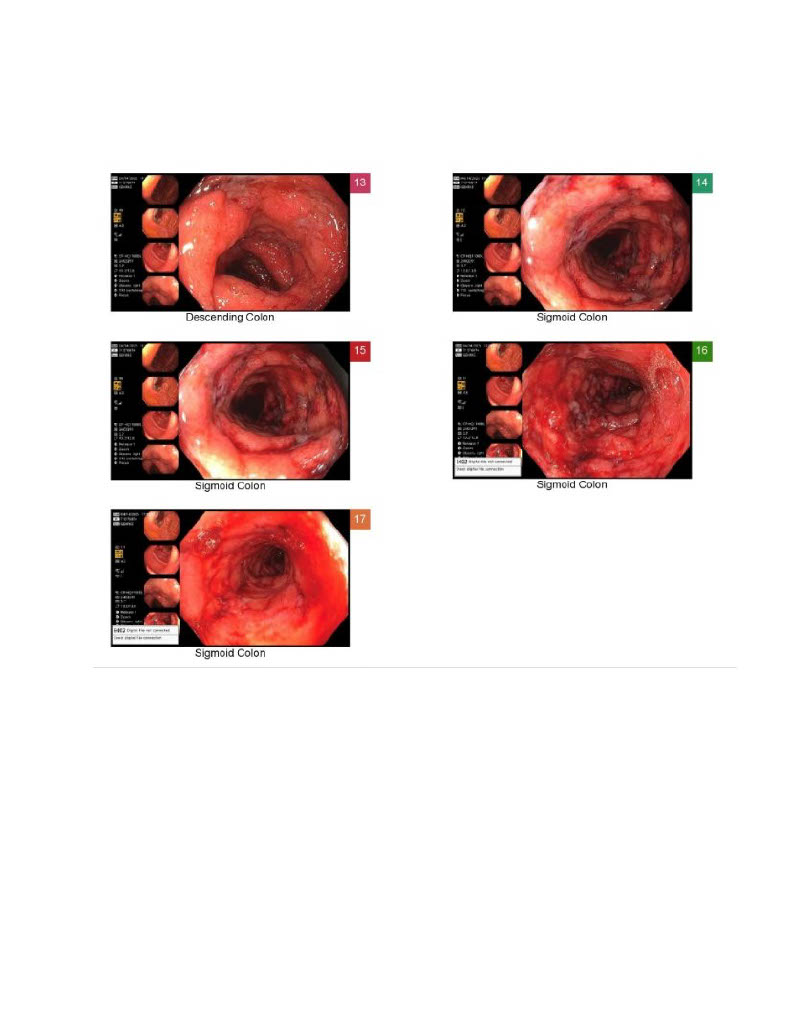
Figure: Colonoscopy images #2
Disclosures:
Mark Shokralla indicated no relevant financial relationships.
Mark Shokralla, DO. P5514 - Ulcerative Colitis Unmasked by a Clostridioides difficile Infection: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Texas Health San Antonio, San Antonio, TX
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease affecting over 900,000 individuals in the United States, with an annual incidence of 9–20 cases per 100,000 people. While typically diagnosed in younger adults, up to 15% of cases present after age 60. Clostridioides difficile infection (CDI) is a known trigger for colonic inflammation and may unmask underlying IBD. Differentiating post-infectious colitis from new-onset UC can be challenging. We present a case of elderly-onset UC diagnosed following persistent diarrhea after CDI, highlighting the importance of considering IBD in refractory cases.
Case Description/
Methods: A 77-year-old male with CAD (post-CABG/PCI) and type 2 diabetes presented with two months of profuse green, watery diarrhea ( >20x/day), fecal incontinence, and a 40-pound weight loss. Symptoms began after completing a 7-day course of Cefdinir. He denied GI bleeding, fever, recent travel, or sick contacts. There was no prior history of IBD, IBS, celiac disease, or pancreatitis.
He initially tested positive for C. difficile and was treated with a 2-week course of oral vancomycin, with only brief symptom improvement. Due to ongoing weight loss and persistent diarrhea, he presented to the ED. He appeared pale but was stable. Abdominal exam revealed decreased bowel sounds; labs showed iron deficiency anemia, elevated ESR (98), CRP (54), fecal calprotectin >1200, positive FIT, and normal WBC and platelets.
CT abdomen/pelvis showed diffuse colonic wall thickening from the transverse colon to the rectum, consistent with proctocolitis. A colonoscopy revealed continuous severe inflammation from the rectum to the cecum with friability, granularity, and ulcerations—most pronounced in the left colon. Biopsies showed active colitis with chronic architectural changes.
He was started on IV methylprednisolone, transitioned to a prednisone taper, and initiated on vedolizumab. He reported symptom improvement, with CRP decreasing from 54 to 13, and he was referred to the IBD clinic for ongoing care.
Discussion: Persistent diarrhea after C. difficile treatment should prompt evaluation for underlying IBD. In this case, weight loss, elevated inflammatory markers, and chronic colitis on biopsy supported new-onset ulcerative colitis. C. difficile may unmask IBD, especially in older adults with atypical symptoms. Early colonoscopy is essential when symptoms persist. The patient improved with corticosteroids and vedolizumab, aligning with standard UC therapy.
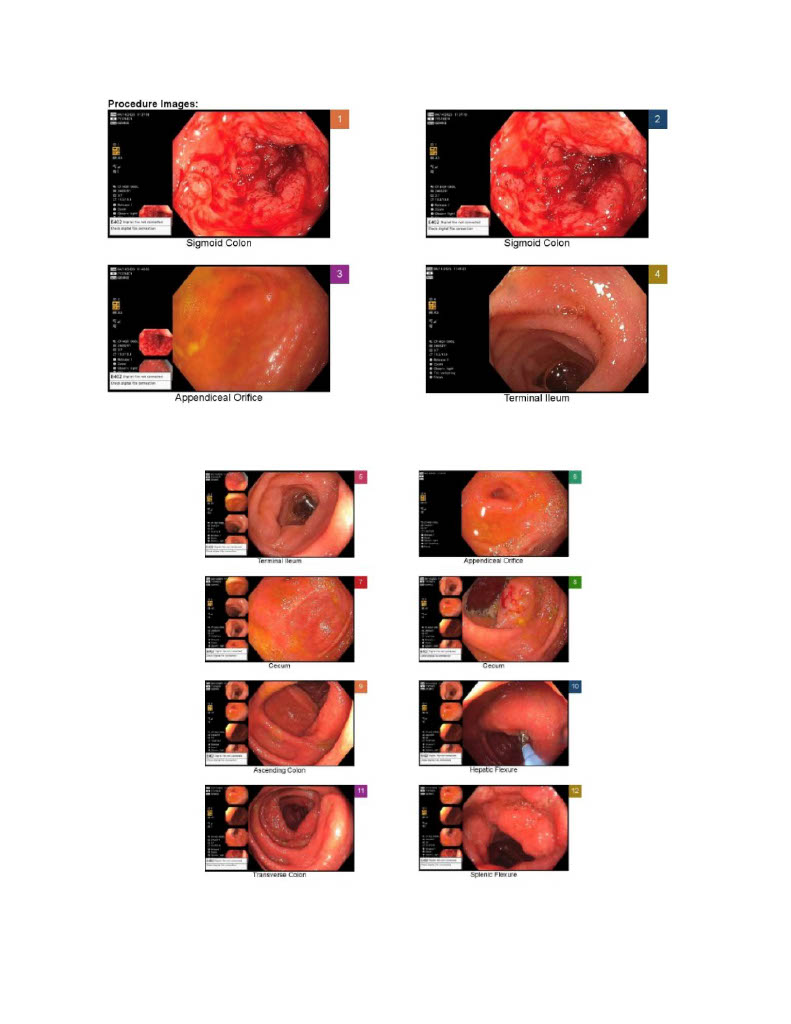
Figure: Colonoscopy images #1
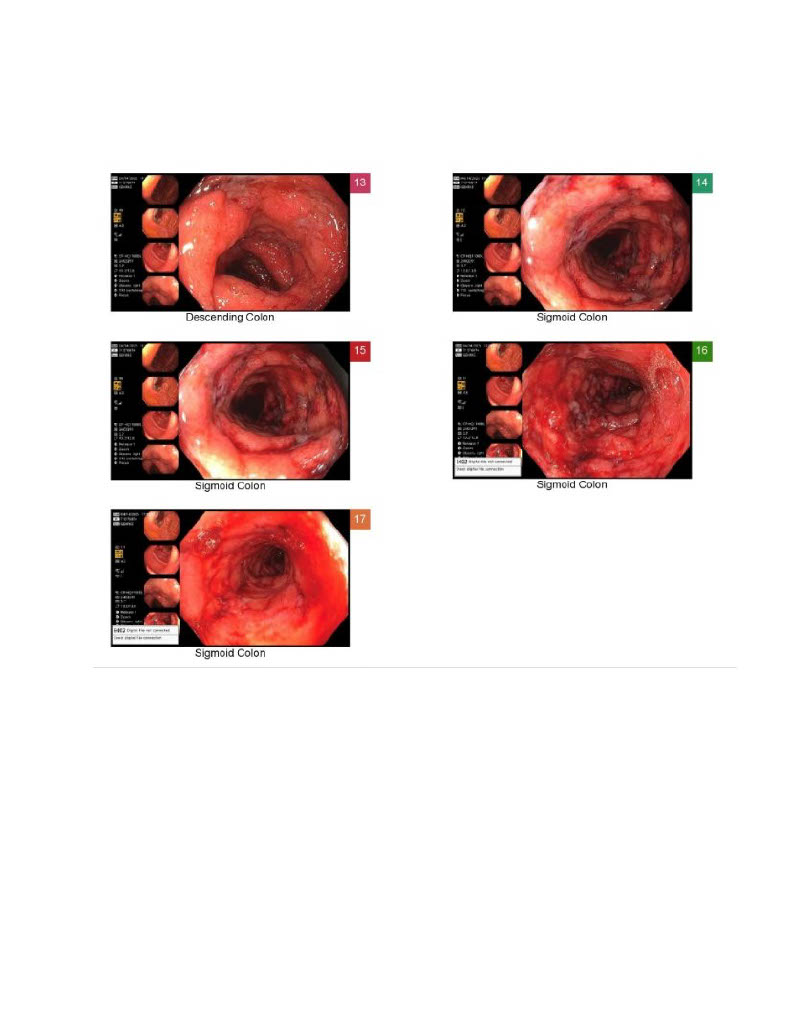
Figure: Colonoscopy images #2
Disclosures:
Mark Shokralla indicated no relevant financial relationships.
Mark Shokralla, DO. P5514 - Ulcerative Colitis Unmasked by a Clostridioides difficile Infection: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
