Tuesday Poster Session
Category: IBD
P5510 - Drug-Induced Colitis in a Patient With Rheumatoid Arthritis on Abatacept Therapy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MA
Maryam Aslani, MD
.
Hoboken, NJ
Presenting Author(s)
Maryam Aslani, MD1, Adwait Patel, MD2, Kovil Ramasamy, MD2
1., Hoboken, NJ; 2Bayonne Medical Center, Bayonne, NJ
Introduction: Drug-induced inflammatory colitis encompasses a range of colon disorders that can manifest microscopically or macroscopically. Medications prescribed for rheumatic conditions can trigger flare-ups of inflammatory bowel disease (IBD) or lead to de novo colitis. Therapeutic monoclonal anti-cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) antibodies are associated with immune-mediated enterocolitis. Abatacept, a fusion protein targeting CTLA-4, is commonly used for rheumatoid arthritis (RA) but has been associated with gastrointestinal adverse effects, including enterocolitis. While abatacept-induced colitis is rare, it can resemble Crohn's disease (CD) or ulcerative colitis (UC), with symptoms of colonic inflammation, sometimes complicated by fistula formation. This case highlights abatacept-induced colitis and offers guidance for physicians managing such cases—typically involving discontinuation of the suspected medication and treatment with steroids or immune-modulating therapies.
Case Description/
Methods: A 63-year-old female with a history of hypertension, hyperlipidemia, and rheumatoid arthritis (treated with leflunomide and abatacept) presented to the emergency department with 12 days of severe, diffuse, crampy abdominal pain and persistent watery diarrhea. Labs revealed leukocytosis (WBC 13 x 10^9/L), with elevated inflammatory markers and liver enzymes. CT imaging showed ileal and colonic thickening suggestive of IBD. Stool cultures and serologies were negative for Clostridium difficile and viral pathogens. Colonoscopy revealed sigmoid and rectal ulcers, with biopsies showing acute and chronic colitis with cryptitis. After excluding infectious causes, abatacept was identified as the likely trigger and was discontinued. The patient was started on Entocort, leading to symptom resolution at follow-up.
Discussion: This case highlights the rare but significant potential for abatacept to induce severe colitis in RA patients. The pathophysiology involves the suppression of regulatory T cells, which plays a crucial role in maintaining intestinal immune tolerance. Previous cases describe management with drug withdrawal and therapies like mesalamine, infliximab, or steroids. In this case, endoscopic findings and histology supported the diagnosis of abatacept-induced colitis, with improvement after drug cessation. Early colonoscopy and abatacept withdrawal are crucial for patients with suspected drug-induced colitis presenting with diarrhea or gastrointestinal bleeding.

Figure: Endoscopic image of the rectum demonstrating mucosal erythema and ulceration.
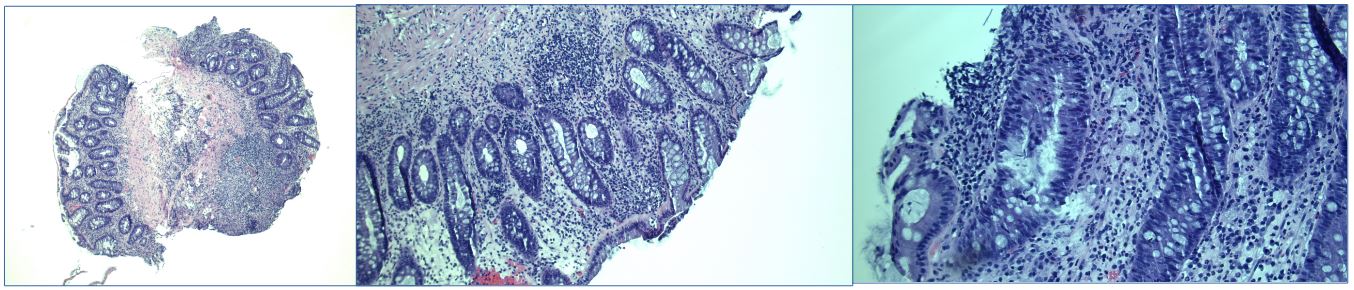
Figure: Low-power view reveals distortion of the crypt architecture along with focal areas of ulceration. Both low- and medium-power magnifications demonstrate features of chronic inflammation. High-power view highlights acute inflammatory changes, including cryptitis.
Disclosures:
Maryam Aslani indicated no relevant financial relationships.
Adwait Patel indicated no relevant financial relationships.
Kovil Ramasamy indicated no relevant financial relationships.
Maryam Aslani, MD1, Adwait Patel, MD2, Kovil Ramasamy, MD2. P5510 - Drug-Induced Colitis in a Patient With Rheumatoid Arthritis on Abatacept Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1., Hoboken, NJ; 2Bayonne Medical Center, Bayonne, NJ
Introduction: Drug-induced inflammatory colitis encompasses a range of colon disorders that can manifest microscopically or macroscopically. Medications prescribed for rheumatic conditions can trigger flare-ups of inflammatory bowel disease (IBD) or lead to de novo colitis. Therapeutic monoclonal anti-cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) antibodies are associated with immune-mediated enterocolitis. Abatacept, a fusion protein targeting CTLA-4, is commonly used for rheumatoid arthritis (RA) but has been associated with gastrointestinal adverse effects, including enterocolitis. While abatacept-induced colitis is rare, it can resemble Crohn's disease (CD) or ulcerative colitis (UC), with symptoms of colonic inflammation, sometimes complicated by fistula formation. This case highlights abatacept-induced colitis and offers guidance for physicians managing such cases—typically involving discontinuation of the suspected medication and treatment with steroids or immune-modulating therapies.
Case Description/
Methods: A 63-year-old female with a history of hypertension, hyperlipidemia, and rheumatoid arthritis (treated with leflunomide and abatacept) presented to the emergency department with 12 days of severe, diffuse, crampy abdominal pain and persistent watery diarrhea. Labs revealed leukocytosis (WBC 13 x 10^9/L), with elevated inflammatory markers and liver enzymes. CT imaging showed ileal and colonic thickening suggestive of IBD. Stool cultures and serologies were negative for Clostridium difficile and viral pathogens. Colonoscopy revealed sigmoid and rectal ulcers, with biopsies showing acute and chronic colitis with cryptitis. After excluding infectious causes, abatacept was identified as the likely trigger and was discontinued. The patient was started on Entocort, leading to symptom resolution at follow-up.
Discussion: This case highlights the rare but significant potential for abatacept to induce severe colitis in RA patients. The pathophysiology involves the suppression of regulatory T cells, which plays a crucial role in maintaining intestinal immune tolerance. Previous cases describe management with drug withdrawal and therapies like mesalamine, infliximab, or steroids. In this case, endoscopic findings and histology supported the diagnosis of abatacept-induced colitis, with improvement after drug cessation. Early colonoscopy and abatacept withdrawal are crucial for patients with suspected drug-induced colitis presenting with diarrhea or gastrointestinal bleeding.

Figure: Endoscopic image of the rectum demonstrating mucosal erythema and ulceration.
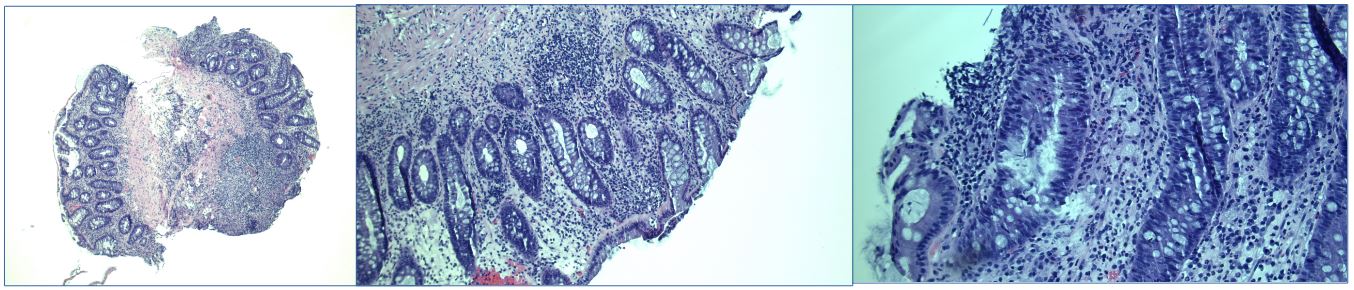
Figure: Low-power view reveals distortion of the crypt architecture along with focal areas of ulceration. Both low- and medium-power magnifications demonstrate features of chronic inflammation. High-power view highlights acute inflammatory changes, including cryptitis.
Disclosures:
Maryam Aslani indicated no relevant financial relationships.
Adwait Patel indicated no relevant financial relationships.
Kovil Ramasamy indicated no relevant financial relationships.
Maryam Aslani, MD1, Adwait Patel, MD2, Kovil Ramasamy, MD2. P5510 - Drug-Induced Colitis in a Patient With Rheumatoid Arthritis on Abatacept Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
