Tuesday Poster Session
Category: IBD
P5481 - The Prevalence of Psychiatric Comorbidities in Inflammatory Bowel Disease: A Stratified Analysis With a National Database
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sydney R. Donohue, MD (she/her/hers)
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Sydney R. Donohue, MD1, Alekhya Mannava, MD, MBA1, Jaime A. Perez, PhD1, Vu Nguyen, MD1, Preetika Sinh, MD2, Fabio Cominelli, MD, PhD1, Jeffry A.. Katz, MD1, Gregory S. Cooper, MD3, Miguel Regueiro, MD4, Emad Mansoor, MD1
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Medical College of Wisconsin, Milwaukee, WI; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 4Cleveland Clinic, Cleveland, OH
Introduction: Patients with Inflammatory Bowel Disease (IBD) have a higher psychiatric disease burden as the prevalence of psychiatric comorbidities is increased in this population. Currently, there is limited data on the classification of patients affected by both IBD and psychiatric comorbidities. Here, we evaluated the prevalence of psychiatric disorders in IBD patients actively receiving treatment and their epidemiologic characteristics.
Methods: An observational study was performed using a national database with over 113 million patients (TriNetX Research Network, Cambridge, MA; accessed 11/27/2024; IRB exempt). We identified all adult patients (≥18 years) diagnosed with IBD (ICD-10; K50, K51) using IBD-specific medication on/after 01/01/2014. We examined the outcomes of psychiatric diagnoses, including major depressive disorder (MDD), generalized anxiety disorder (GAD), bipolar disorder, schizophrenia, post-traumatic stress disorder (PTSD), obsessive compulsive disorder (OCD), attention-deficit hyperactivity disorder (ADHD), alcohol (AUD) and opiate use disorder (OUD) and suicide attempts, using ICD-10 codes. Patients who had an instance of the event of interest during this period were considered a prevalent case. We calculated the prevalence of each condition and stratified based on age, sex, race, and ethnicity.
Results: We identified 196,438 IBD patients who had been prescribed IBD specific medications. The overall psychiatric diagnosis prevalence was 20.9%. Female patients had a higher prevalence of MDD (7.89% vs. 4.41%) and GAD (10.4% vs. 5.81%). The prevalence was higher in female patients than males in all conditions except schizophrenia, ADHD, and AUD. Native Hawaiians/Pacific Islanders had the highest prevalence of GAD, bipolar disorder, OUD, OCD, and schizophrenia. American Indians/Alaska Natives had the highest prevalence of PTSD, ADHD, AUD, and suicide attempts. Regarding ethnicity, patients who were not Hispanic/Latino had a higher prevalence for majority of the conditions compared to Hispanic/Latino patients. By age, the prevalence was higher in the younger ages for GAD, bipolar disorder, PTSD, OCD, ADHD, and OUD.
Discussion: To our knowledge, this is one of the largest multi-institutional, epidemiologic studies on the association between IBD and psychiatric disease burden. This highlights the need for more in-depth mental health screening in IBD patients and can help alert physicians to potential at risk subgroups for mental health intervention.
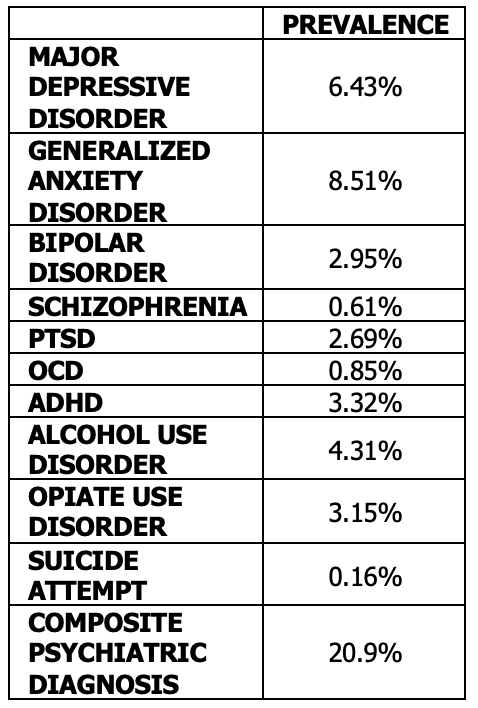
Figure: Table 1: General prevalence of psychiatric conditions in patients with IBD receiving treatment
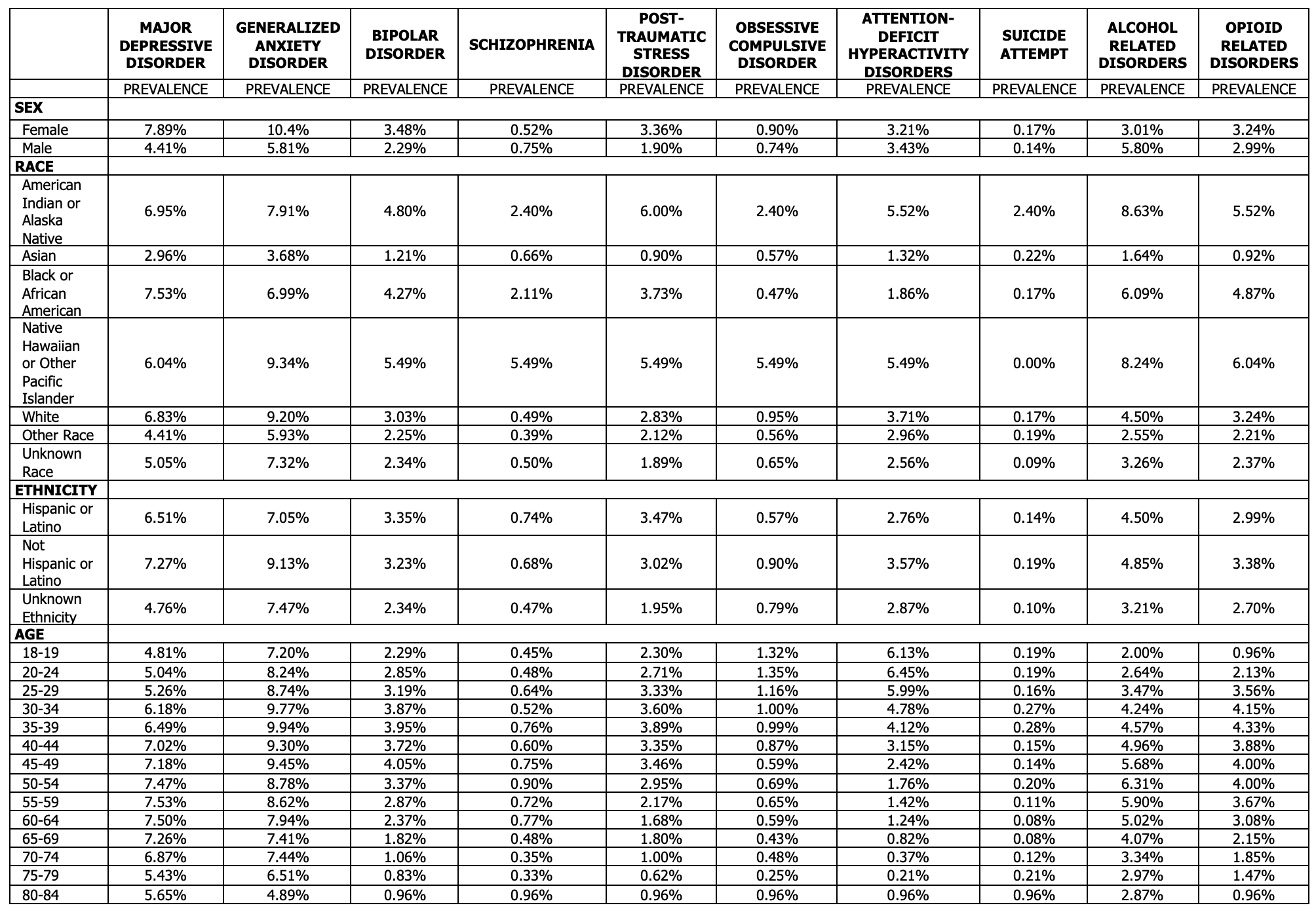
Figure: Table 2: Prevalence of psychiatric conditions in patients with IBD receiving treatment by sex, race, ethnicity, and age
Disclosures:
Sydney Donohue indicated no relevant financial relationships.
Alekhya Mannava indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Vu Nguyen: AbbVie – Consultant, Speakers Bureau. Johnson & Johnson – Consultant, Speakers Bureau.
Preetika Sinh: Bristol Myers Squibb – Advisory Committee/Board Member.
Fabio Cominelli indicated no relevant financial relationships.
Jeffry Katz indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Miguel Regueiro: AbbVie – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant. BMS – Advisory Committee/Board Member, Consultant. Boehringer Ingelheim Pharmaceuticals Inc. – Advisory Committee/Board Member, Consultant. Celegene – Advisory Committee/Board Member, Consultant. Eli Lilly and Company – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant. Organon – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant. Prometheus – Advisory Committee/Board Member, Consultant. Salix – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Sydney R. Donohue, MD1, Alekhya Mannava, MD, MBA1, Jaime A. Perez, PhD1, Vu Nguyen, MD1, Preetika Sinh, MD2, Fabio Cominelli, MD, PhD1, Jeffry A.. Katz, MD1, Gregory S. Cooper, MD3, Miguel Regueiro, MD4, Emad Mansoor, MD1. P5481 - The Prevalence of Psychiatric Comorbidities in Inflammatory Bowel Disease: A Stratified Analysis With a National Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Medical College of Wisconsin, Milwaukee, WI; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 4Cleveland Clinic, Cleveland, OH
Introduction: Patients with Inflammatory Bowel Disease (IBD) have a higher psychiatric disease burden as the prevalence of psychiatric comorbidities is increased in this population. Currently, there is limited data on the classification of patients affected by both IBD and psychiatric comorbidities. Here, we evaluated the prevalence of psychiatric disorders in IBD patients actively receiving treatment and their epidemiologic characteristics.
Methods: An observational study was performed using a national database with over 113 million patients (TriNetX Research Network, Cambridge, MA; accessed 11/27/2024; IRB exempt). We identified all adult patients (≥18 years) diagnosed with IBD (ICD-10; K50, K51) using IBD-specific medication on/after 01/01/2014. We examined the outcomes of psychiatric diagnoses, including major depressive disorder (MDD), generalized anxiety disorder (GAD), bipolar disorder, schizophrenia, post-traumatic stress disorder (PTSD), obsessive compulsive disorder (OCD), attention-deficit hyperactivity disorder (ADHD), alcohol (AUD) and opiate use disorder (OUD) and suicide attempts, using ICD-10 codes. Patients who had an instance of the event of interest during this period were considered a prevalent case. We calculated the prevalence of each condition and stratified based on age, sex, race, and ethnicity.
Results: We identified 196,438 IBD patients who had been prescribed IBD specific medications. The overall psychiatric diagnosis prevalence was 20.9%. Female patients had a higher prevalence of MDD (7.89% vs. 4.41%) and GAD (10.4% vs. 5.81%). The prevalence was higher in female patients than males in all conditions except schizophrenia, ADHD, and AUD. Native Hawaiians/Pacific Islanders had the highest prevalence of GAD, bipolar disorder, OUD, OCD, and schizophrenia. American Indians/Alaska Natives had the highest prevalence of PTSD, ADHD, AUD, and suicide attempts. Regarding ethnicity, patients who were not Hispanic/Latino had a higher prevalence for majority of the conditions compared to Hispanic/Latino patients. By age, the prevalence was higher in the younger ages for GAD, bipolar disorder, PTSD, OCD, ADHD, and OUD.
Discussion: To our knowledge, this is one of the largest multi-institutional, epidemiologic studies on the association between IBD and psychiatric disease burden. This highlights the need for more in-depth mental health screening in IBD patients and can help alert physicians to potential at risk subgroups for mental health intervention.
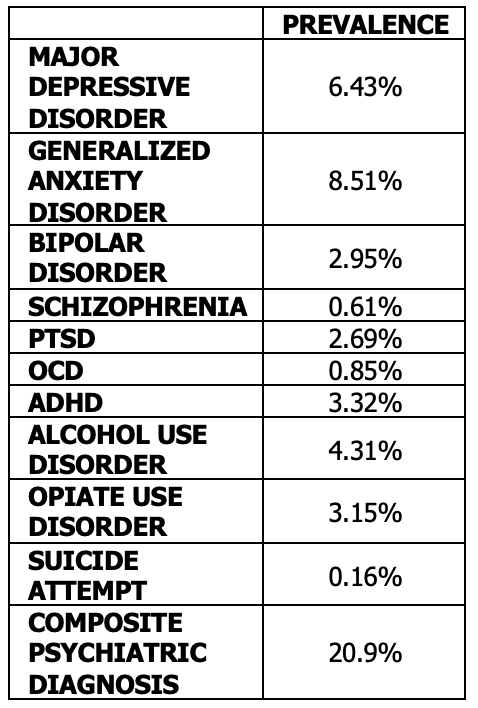
Figure: Table 1: General prevalence of psychiatric conditions in patients with IBD receiving treatment
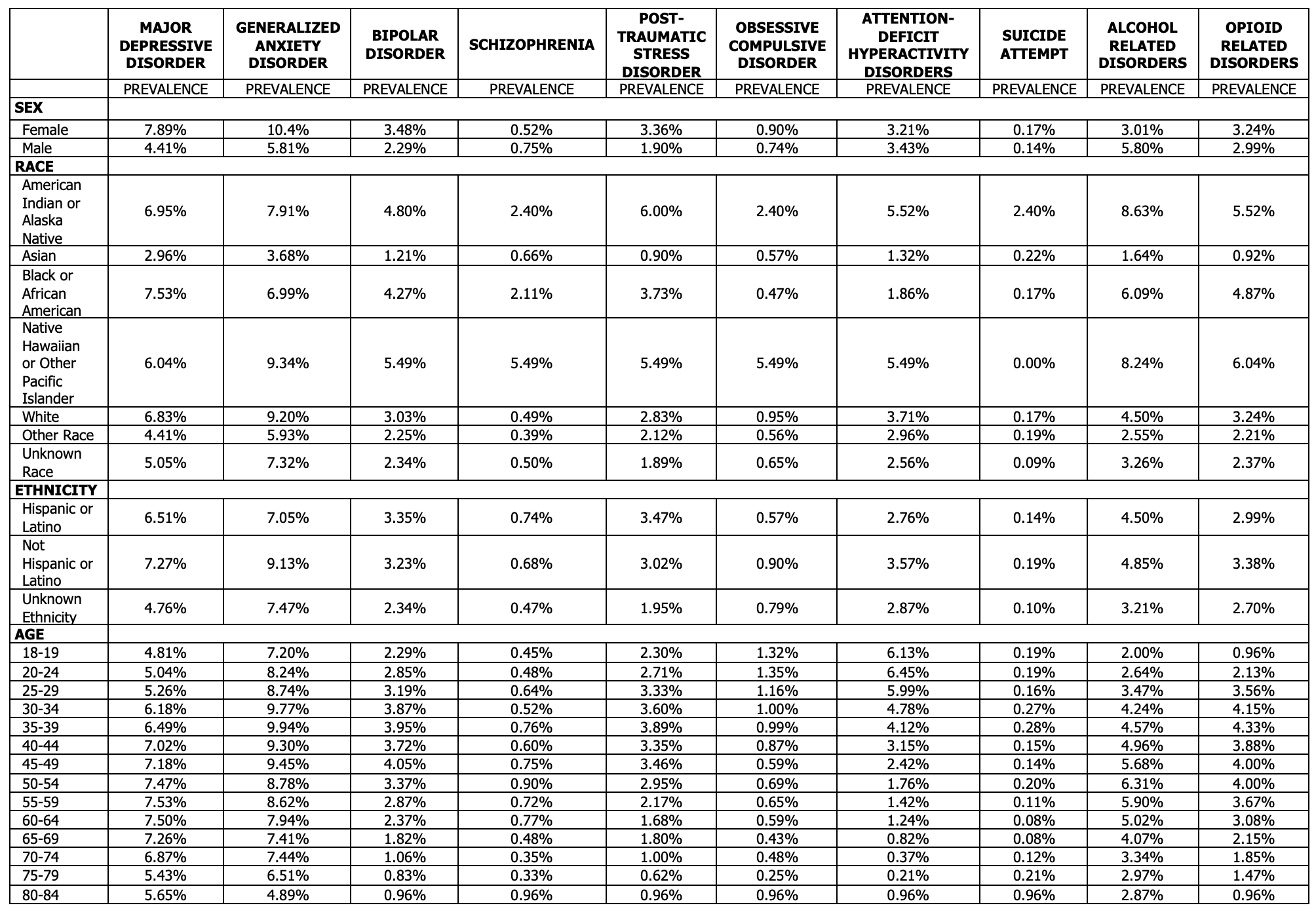
Figure: Table 2: Prevalence of psychiatric conditions in patients with IBD receiving treatment by sex, race, ethnicity, and age
Disclosures:
Sydney Donohue indicated no relevant financial relationships.
Alekhya Mannava indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Vu Nguyen: AbbVie – Consultant, Speakers Bureau. Johnson & Johnson – Consultant, Speakers Bureau.
Preetika Sinh: Bristol Myers Squibb – Advisory Committee/Board Member.
Fabio Cominelli indicated no relevant financial relationships.
Jeffry Katz indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Miguel Regueiro: AbbVie – Advisory Committee/Board Member, Consultant. Amgen – Advisory Committee/Board Member, Consultant. BMS – Advisory Committee/Board Member, Consultant. Boehringer Ingelheim Pharmaceuticals Inc. – Advisory Committee/Board Member, Consultant. Celegene – Advisory Committee/Board Member, Consultant. Eli Lilly and Company – Advisory Committee/Board Member, Consultant. Genentech – Advisory Committee/Board Member, Consultant. Gilead – Advisory Committee/Board Member, Consultant. Janssen – Advisory Committee/Board Member, Consultant. Organon – Advisory Committee/Board Member, Consultant. Pfizer – Advisory Committee/Board Member, Consultant. Prometheus – Advisory Committee/Board Member, Consultant. Salix – Advisory Committee/Board Member, Consultant. Takeda – Advisory Committee/Board Member, Consultant. UCB – Advisory Committee/Board Member, Consultant.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Sydney R. Donohue, MD1, Alekhya Mannava, MD, MBA1, Jaime A. Perez, PhD1, Vu Nguyen, MD1, Preetika Sinh, MD2, Fabio Cominelli, MD, PhD1, Jeffry A.. Katz, MD1, Gregory S. Cooper, MD3, Miguel Regueiro, MD4, Emad Mansoor, MD1. P5481 - The Prevalence of Psychiatric Comorbidities in Inflammatory Bowel Disease: A Stratified Analysis With a National Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
