Tuesday Poster Session
Category: IBD
P5470 - Impact of Brief COVID-19 Pandemic-Associated Endoscopy Delays on Patients With Inflammatory Bowel Disease: A Retrospective Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DR
Daniyal Raza, MD (he/him/his)
LSU Health Sciences Center - SHREVEPORT, LA
Shreveport, LA
Presenting Author(s)
Daniyal Raza, MD1, Khadija Khan, MD2, Farhan Mohiuddin, MD3, Mohammad Alfrad Nobel Bhuiyan, MD4, Sudha Pandit, MD4
1LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA; 2LSU Health Shreveport, Shreveport, LA; 3Louisiana State University School of Medicine, New Orleans, LA; 4Louisiana State University, Shreveport, LA
Introduction: The COVID-19 pandemic led to widespread delays in non-urgent endoscopic procedures, raising concerns about potential adverse outcomes in patients with inflammatory bowel disease (IBD). However, emerging evidence suggests that such delays may not uniformly result in worse clinical outcomes. For instance, a study by Patel et al. found no significant difference in adverse events between patients with delayed and on-time endoscopies, and even observed higher rates of hospitalizations and surgeries in the on-time group, possibly reflecting more severe disease or increased healthcare engagement.
Methods: We conducted a retrospective cohort study on patients with Crohn's disease or ulcerative colitis who underwent endoscopy at a tertiary care center in the U.S. between March 1, 2020, and August 31, 2020. Patients were divided into two groups based on whether their procedures were delayed. We evaluated adverse outcomes including emergency visits, hospitalizations, surgeries, and medication escalation. Covariates were assessed using logistic regression models (Table 1, Table 2). Procedural volume trends during the pandemic and post-pandemic periods were also analyzed (Figure 2). A comparison of adverse outcomes between groups is shown in Figure 1.
Results: No statistically significant association was observed between endoscopy delay and adverse IBD-related outcomes (OR 2.24, 95% CI 0.69–7.85; P=0.18). Similarly, age, sex, disease subtype, and RUCA classification were not significantly associated with adverse outcomes (Table 1) or with the likelihood of procedural delay (Table 2). Endoscopic procedure volume was markedly reduced during the pandemic (n=73) compared to the post-pandemic period (n=625), reflecting operational disruption (Figure 2). Unadjusted frequencies showed a numerically higher proportion of adverse events in patients with delayed procedures (Figure 1), but this difference did not reach statistical significance.
Discussion: In this single-center retrospective analysis, delays in endoscopy during the COVID-19 pandemic were not significantly associated with adverse clinical outcomes in patients with IBD. These findings align with recent literature suggesting that, in certain contexts, endoscopy delays did not lead to worse outcomes. However, the observed trends underscore the need for continued evaluation of procedural triaging during system-wide disruptions and support efforts to maintain timely access to endoscopic care.
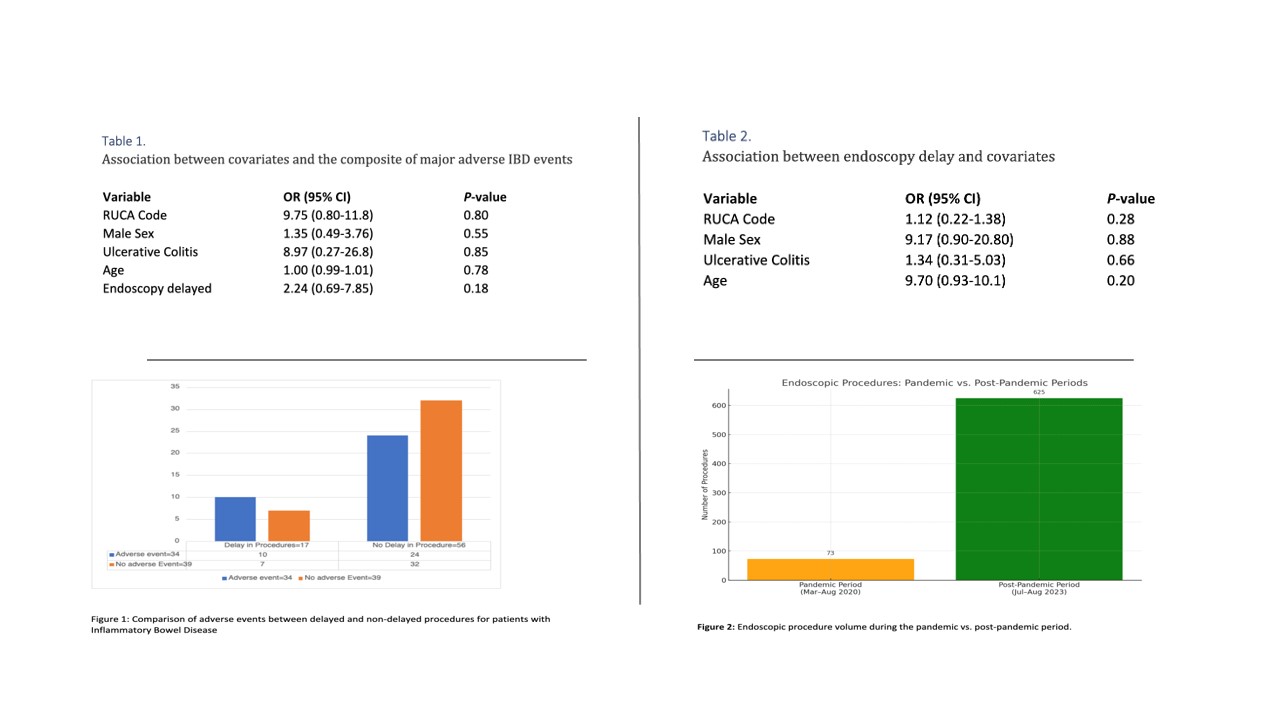
Figure: Impact of COVID-19–Related Endoscopy Delays on Adverse Outcomes in Patients with Inflammatory Bowel Disease
Disclosures:
Daniyal Raza indicated no relevant financial relationships.
Khadija Khan indicated no relevant financial relationships.
Farhan Mohiuddin indicated no relevant financial relationships.
Mohammad Alfrad Nobel Bhuiyan indicated no relevant financial relationships.
Sudha Pandit: Medtronic – Product feedback.
Daniyal Raza, MD1, Khadija Khan, MD2, Farhan Mohiuddin, MD3, Mohammad Alfrad Nobel Bhuiyan, MD4, Sudha Pandit, MD4. P5470 - Impact of Brief COVID-19 Pandemic-Associated Endoscopy Delays on Patients With Inflammatory Bowel Disease: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA; 2LSU Health Shreveport, Shreveport, LA; 3Louisiana State University School of Medicine, New Orleans, LA; 4Louisiana State University, Shreveport, LA
Introduction: The COVID-19 pandemic led to widespread delays in non-urgent endoscopic procedures, raising concerns about potential adverse outcomes in patients with inflammatory bowel disease (IBD). However, emerging evidence suggests that such delays may not uniformly result in worse clinical outcomes. For instance, a study by Patel et al. found no significant difference in adverse events between patients with delayed and on-time endoscopies, and even observed higher rates of hospitalizations and surgeries in the on-time group, possibly reflecting more severe disease or increased healthcare engagement.
Methods: We conducted a retrospective cohort study on patients with Crohn's disease or ulcerative colitis who underwent endoscopy at a tertiary care center in the U.S. between March 1, 2020, and August 31, 2020. Patients were divided into two groups based on whether their procedures were delayed. We evaluated adverse outcomes including emergency visits, hospitalizations, surgeries, and medication escalation. Covariates were assessed using logistic regression models (Table 1, Table 2). Procedural volume trends during the pandemic and post-pandemic periods were also analyzed (Figure 2). A comparison of adverse outcomes between groups is shown in Figure 1.
Results: No statistically significant association was observed between endoscopy delay and adverse IBD-related outcomes (OR 2.24, 95% CI 0.69–7.85; P=0.18). Similarly, age, sex, disease subtype, and RUCA classification were not significantly associated with adverse outcomes (Table 1) or with the likelihood of procedural delay (Table 2). Endoscopic procedure volume was markedly reduced during the pandemic (n=73) compared to the post-pandemic period (n=625), reflecting operational disruption (Figure 2). Unadjusted frequencies showed a numerically higher proportion of adverse events in patients with delayed procedures (Figure 1), but this difference did not reach statistical significance.
Discussion: In this single-center retrospective analysis, delays in endoscopy during the COVID-19 pandemic were not significantly associated with adverse clinical outcomes in patients with IBD. These findings align with recent literature suggesting that, in certain contexts, endoscopy delays did not lead to worse outcomes. However, the observed trends underscore the need for continued evaluation of procedural triaging during system-wide disruptions and support efforts to maintain timely access to endoscopic care.
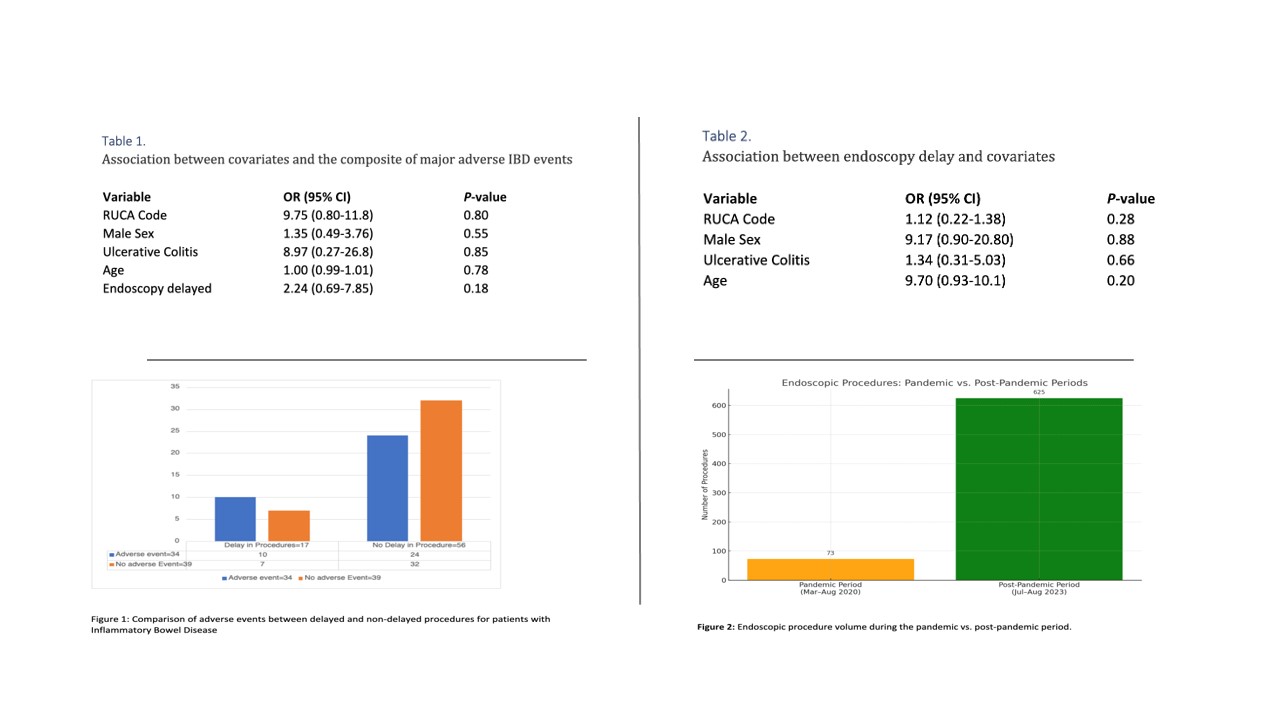
Figure: Impact of COVID-19–Related Endoscopy Delays on Adverse Outcomes in Patients with Inflammatory Bowel Disease
Disclosures:
Daniyal Raza indicated no relevant financial relationships.
Khadija Khan indicated no relevant financial relationships.
Farhan Mohiuddin indicated no relevant financial relationships.
Mohammad Alfrad Nobel Bhuiyan indicated no relevant financial relationships.
Sudha Pandit: Medtronic – Product feedback.
Daniyal Raza, MD1, Khadija Khan, MD2, Farhan Mohiuddin, MD3, Mohammad Alfrad Nobel Bhuiyan, MD4, Sudha Pandit, MD4. P5470 - Impact of Brief COVID-19 Pandemic-Associated Endoscopy Delays on Patients With Inflammatory Bowel Disease: A Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
