Tuesday Poster Session
Category: IBD
P5439 - Impact of Percutaneous Endoscopic Gastrostomy Tube Placement on Hospitalization Outcomes in Patients With Inflammatory Bowel Disease: A National Inpatient Sample Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpeg.jpg)
Ki Jung Lee, MD
Tufts Medical Center
Boston, MA
Presenting Author(s)
Ki Jung Lee, MD, Gregory Fan, BS, Mohammad Almeqdadi, MD, Saurav Kini, MBBS, Naira Blenheim, MD, James Carey, MD, Lina Zhang, BS
Tufts Medical Center, Boston, MA
Introduction: Patients with inflammatory bowel disease (IBD) often require enteral feeding as part of nutritional management. However, percutaneous endoscopic gastrostomy (PEG) tube placement carries procedural risks and may impact hospitalization outcomes. This study evaluates the association between PEG placement and clinical outcomes in hospitalized IBD patients.
Methods: 306311 (weighted 1531556) patients with IBD were identified from the 2016-2020 National Inpatient Sample Database. The effect of PEG tube placement on hospital-related and procedurally-related endpoints including mortality, length of stay, sepsis, urinary tract infection, pneumonia, respiratory failure, and malnutrition were determined through multivariate analyses that controlled for demographic factors, hypertension, primary biliary cholangitis, primary sclerosing cholangitis and smoking. A matched cohort using 1:1 propensity-score matching to those with PEG tube placements on the basis of age, gender, and race was created and analyzed using the same methods as for the unmatched cohort.
Results: After propensity matching, a total of 14682 patients were included with 7341 in each group. In the unmatched analysis, IBD patients with PEG were younger than those without PEG. Furthermore in the matched analysis, those with PEG were less likely to have metabolic diseases including obesity, hyperlipidemia, and diabetes. IBD patients with PEG placement had statistically prolonged LOS (aIRR 1.71, 95% CI 1.66-1.76, p< 0.001). They were also at higher risk for infectious and other complications, including sepsis (aOR 2.16, 95%CI 1.75-2.68, p< 0.001), UTI (aOR 2.63, 95%CI 2.09-3.32, p< 0.001), pneumonia (aOR 1.99, 95% CI 1.58-2.50, p< 0.001), respiratory failure (aOR 2.08, 95%CI 1.71-2.53, p< 0.001), and malnutrition (aOR 4.43, 95%CI 3.62-5.42, p< 0.001). Although there was no statistical significance, IBD patients who underwent GT experienced higher in-hospital mortality (aOR 1.633, 95% CI 0.96-2.77, p=0.07) and increased hospitalization costs (insert data).
Discussion: PEG tube placement in hospitalized IBD patients is associated with worse clinical outcomes, including longer LOS and higher rates of infectious complications. Limitations include inability to stratify by disease severity or subgroups (e.g., IBD phenotype or BMI) due to sample constraints. Despite these, the findings underscore the need for careful risk-benefit consideration and attention to socioeconomic factors when pursuing PEG in this population.
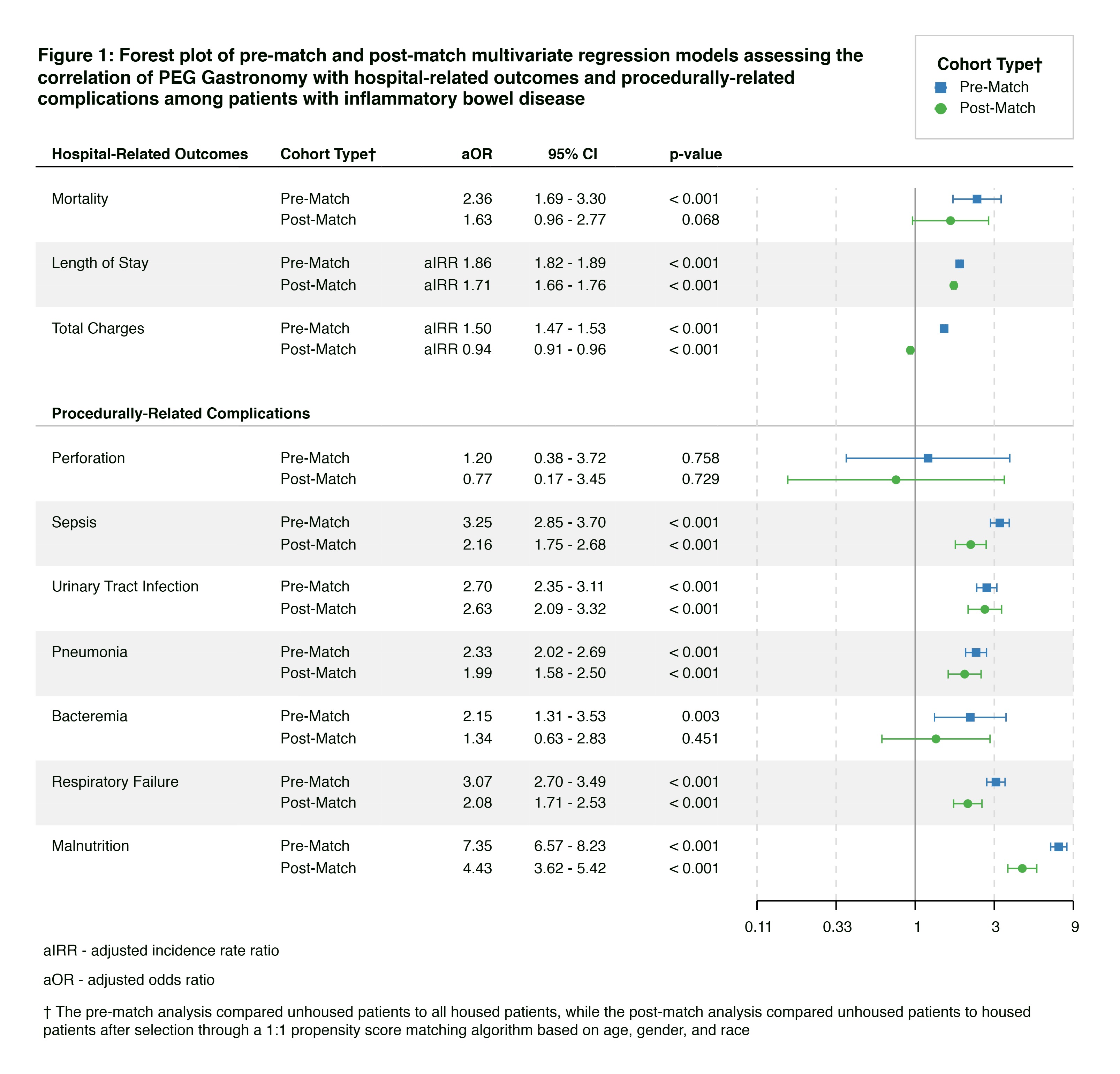
Figure: Figure 1: Forest plot of pre-match and post-match multivariate regression models assessing the correlation of PEG Tube with hospital-related outcomes and procedurally-related complications among patients with inflammatory bowel disease
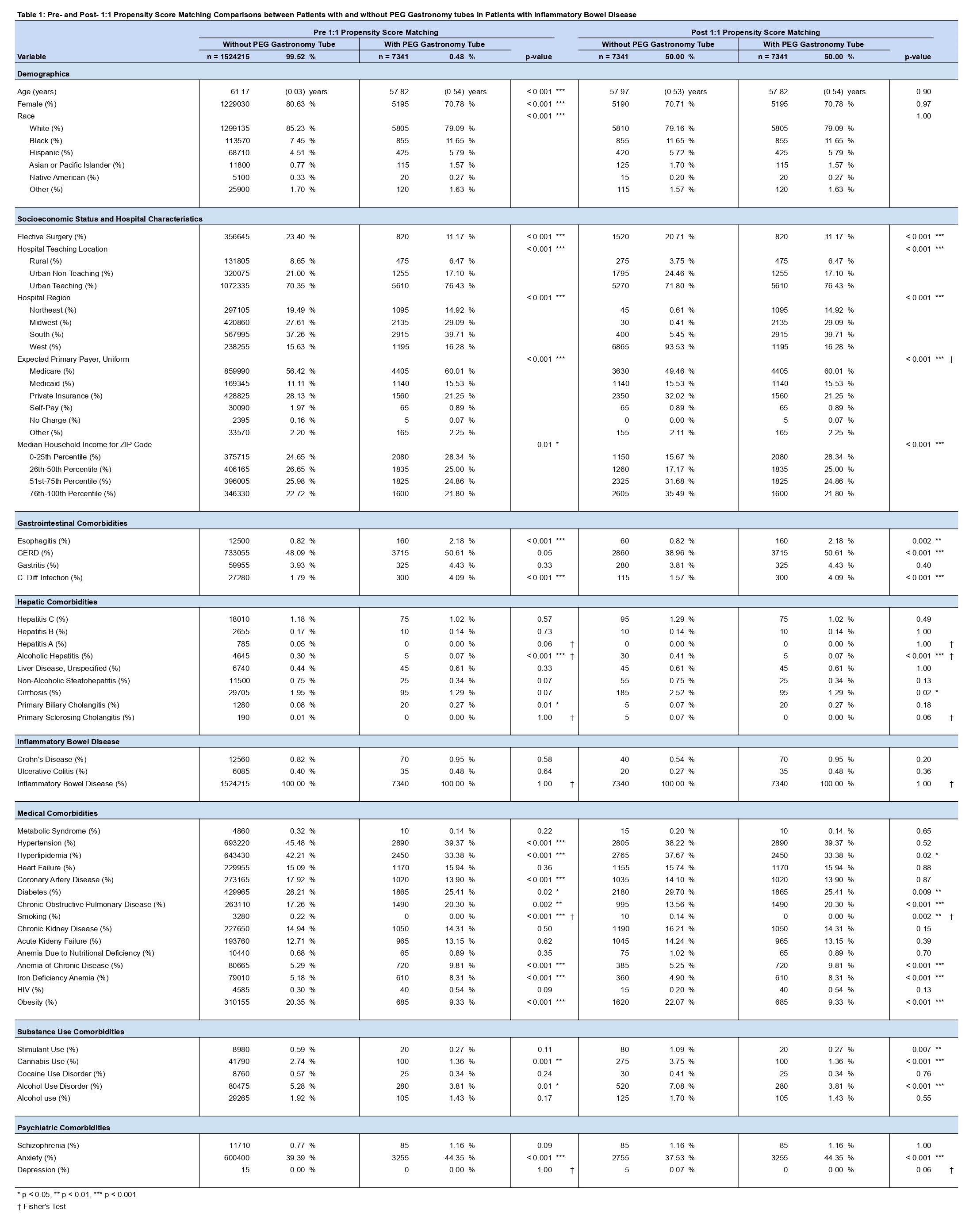
Figure: Table 1: Pre- and Post- 1:1 Propensity Score Matching Comparisons between Patients with and without PEG tubes in Patients with Inflammatory Bowel Disease
Disclosures:
Ki Jung Lee indicated no relevant financial relationships.
Gregory Fan indicated no relevant financial relationships.
Mohammad Almeqdadi indicated no relevant financial relationships.
Saurav Kini indicated no relevant financial relationships.
Naira Blenheim indicated no relevant financial relationships.
James Carey indicated no relevant financial relationships.
Lina Zhang indicated no relevant financial relationships.
Ki Jung Lee, MD, Gregory Fan, BS, Mohammad Almeqdadi, MD, Saurav Kini, MBBS, Naira Blenheim, MD, James Carey, MD, Lina Zhang, BS. P5439 - Impact of Percutaneous Endoscopic Gastrostomy Tube Placement on Hospitalization Outcomes in Patients With Inflammatory Bowel Disease: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Tufts Medical Center, Boston, MA
Introduction: Patients with inflammatory bowel disease (IBD) often require enteral feeding as part of nutritional management. However, percutaneous endoscopic gastrostomy (PEG) tube placement carries procedural risks and may impact hospitalization outcomes. This study evaluates the association between PEG placement and clinical outcomes in hospitalized IBD patients.
Methods: 306311 (weighted 1531556) patients with IBD were identified from the 2016-2020 National Inpatient Sample Database. The effect of PEG tube placement on hospital-related and procedurally-related endpoints including mortality, length of stay, sepsis, urinary tract infection, pneumonia, respiratory failure, and malnutrition were determined through multivariate analyses that controlled for demographic factors, hypertension, primary biliary cholangitis, primary sclerosing cholangitis and smoking. A matched cohort using 1:1 propensity-score matching to those with PEG tube placements on the basis of age, gender, and race was created and analyzed using the same methods as for the unmatched cohort.
Results: After propensity matching, a total of 14682 patients were included with 7341 in each group. In the unmatched analysis, IBD patients with PEG were younger than those without PEG. Furthermore in the matched analysis, those with PEG were less likely to have metabolic diseases including obesity, hyperlipidemia, and diabetes. IBD patients with PEG placement had statistically prolonged LOS (aIRR 1.71, 95% CI 1.66-1.76, p< 0.001). They were also at higher risk for infectious and other complications, including sepsis (aOR 2.16, 95%CI 1.75-2.68, p< 0.001), UTI (aOR 2.63, 95%CI 2.09-3.32, p< 0.001), pneumonia (aOR 1.99, 95% CI 1.58-2.50, p< 0.001), respiratory failure (aOR 2.08, 95%CI 1.71-2.53, p< 0.001), and malnutrition (aOR 4.43, 95%CI 3.62-5.42, p< 0.001). Although there was no statistical significance, IBD patients who underwent GT experienced higher in-hospital mortality (aOR 1.633, 95% CI 0.96-2.77, p=0.07) and increased hospitalization costs (insert data).
Discussion: PEG tube placement in hospitalized IBD patients is associated with worse clinical outcomes, including longer LOS and higher rates of infectious complications. Limitations include inability to stratify by disease severity or subgroups (e.g., IBD phenotype or BMI) due to sample constraints. Despite these, the findings underscore the need for careful risk-benefit consideration and attention to socioeconomic factors when pursuing PEG in this population.
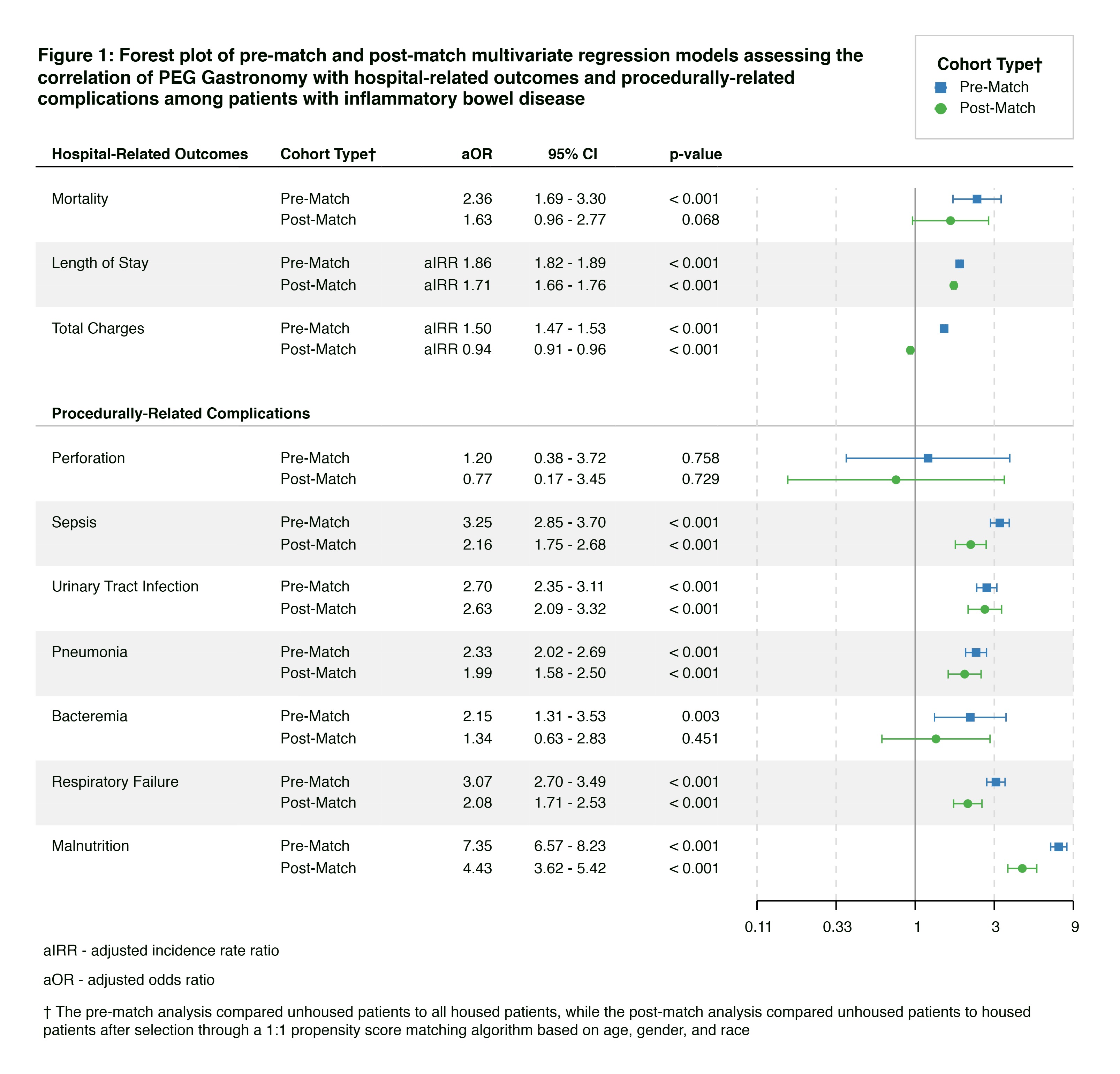
Figure: Figure 1: Forest plot of pre-match and post-match multivariate regression models assessing the correlation of PEG Tube with hospital-related outcomes and procedurally-related complications among patients with inflammatory bowel disease
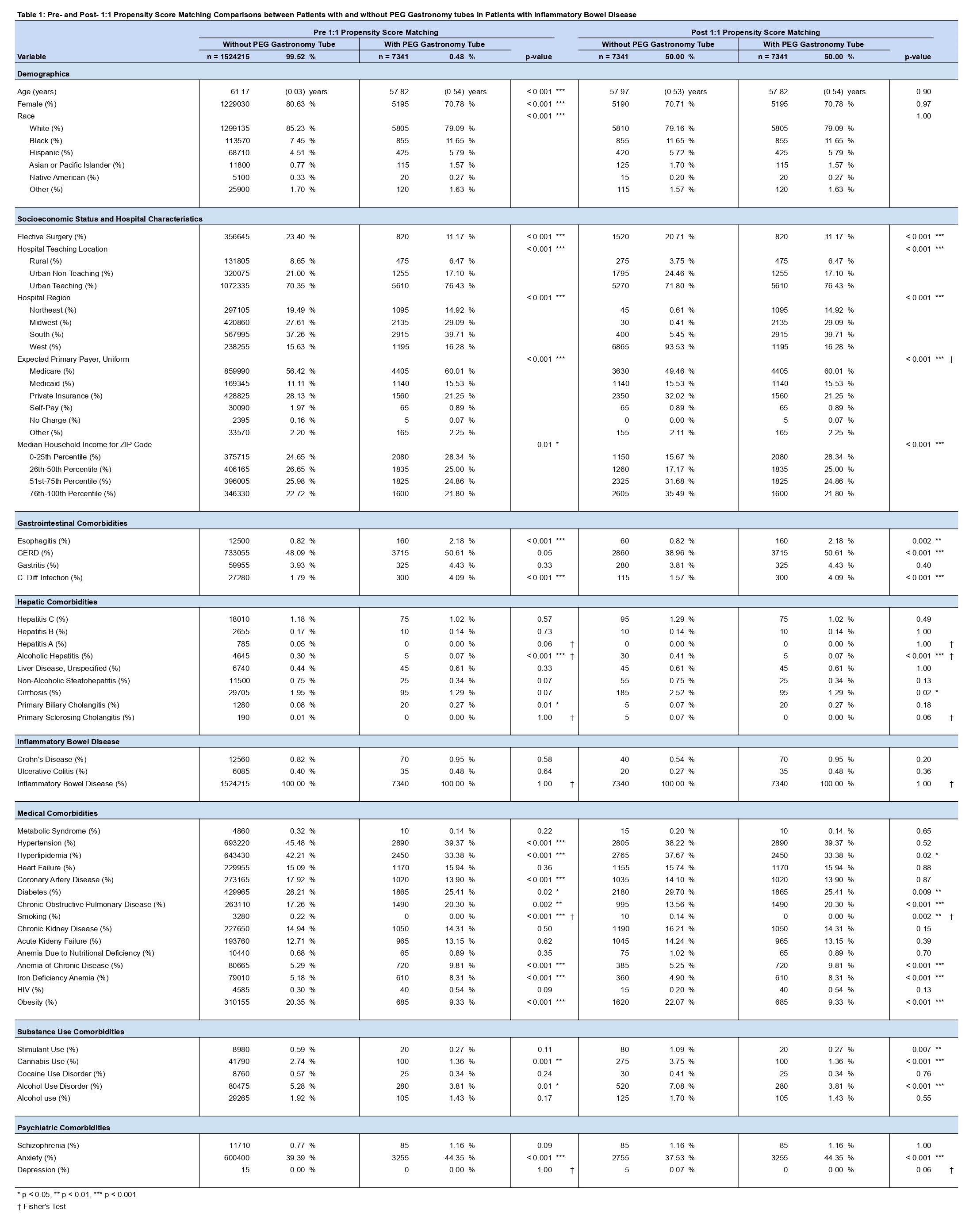
Figure: Table 1: Pre- and Post- 1:1 Propensity Score Matching Comparisons between Patients with and without PEG tubes in Patients with Inflammatory Bowel Disease
Disclosures:
Ki Jung Lee indicated no relevant financial relationships.
Gregory Fan indicated no relevant financial relationships.
Mohammad Almeqdadi indicated no relevant financial relationships.
Saurav Kini indicated no relevant financial relationships.
Naira Blenheim indicated no relevant financial relationships.
James Carey indicated no relevant financial relationships.
Lina Zhang indicated no relevant financial relationships.
Ki Jung Lee, MD, Gregory Fan, BS, Mohammad Almeqdadi, MD, Saurav Kini, MBBS, Naira Blenheim, MD, James Carey, MD, Lina Zhang, BS. P5439 - Impact of Percutaneous Endoscopic Gastrostomy Tube Placement on Hospitalization Outcomes in Patients With Inflammatory Bowel Disease: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
