Tuesday Poster Session
Category: IBD
P5437 - Effect of Dual GLP-1/GIP and GLP-1 Agonists on Inflammatory Bowel Disease Activity Among Patients With Obesity
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JL
Jake Levine, MD
University of Florida Health Shands Hospital
Gainesville, FL
Presenting Author(s)
Jake Levine, MD1, Yao An Lee, BS2, Angela Pham, MD1, Amy Sheer, MD1, Matthew Giansiracusa, DO1, Serena Jingchuan O. Guo, MD, PhD2, Hao Dai, PhD3, Rotana Radwan, PhD2, Jiang Bian, PhD4, Aleksey Novikov, MD5
1University of Florida Health Shands Hospital, Gainesville, FL; 2Department of Pharmaceutical Outcomes and Policy, College of Pharmacy, University of Florida, Gainesville, FL, USA, Gainesville, FL; 3Department of Biostatistics & Health Data Science, Indiana University School of Medicine, Indianapolis, IN, USA, Indianapolis, IN; 4Regenstrief Institute, Indianapolis, IN, USA Department of Biostatistics & Health Data Science, Indiana University School of Medicine, Indianapolis, IN, USA Melvin and Bren Simon Comprehensive Cancer Center, Indiana University, Indianapolis, IN, USA, Gainesville, FL; 5University of Florida College of Medicine, Gainesville, FL
Introduction: Inflammatory bowel disease (IBD), either Crohn’s disease (CD) or ulcerative colitis (UC), is an autoimmune condition characterized by inflammation of GI tract. Obesity is a risk factor for IBD activity. Mounting evidence shows injectable incretins such as Glucagon-like peptide 1 (GLP-1) agonists cause weight loss and may improve IBD disease activity. Newer GLP-1 based agents like tirzepatide, which is a dual agonist of both GLP-1 and Glucose-dependent Insulinotropic Polypeptide (GIP), may have superior weight loss, but their effect on IBD is not known. In this study, we aimed to assess outcomes in patients with IBD and obesity with various GLP-1 medication use versus non-use.
Methods: A retrospective, propensity-matched analysis using data from The OneFlorida+ network from 2012-2023 was done. We evaluated patients with IBD and obesity prescribed GLP-1 based therapy (liraglutide, semaglutide, or tirzepatide) versus those without. 562 patients prescribed GLP-1 based therapies were matched 1:1 to controls based on age, sex, race, BMI, and comorbidities (n=1,124). The control group was time-matched based on GLP-1 users’ index prescription date and all patients were assessed at 12 months. The Cox proportional hazard model was used for analysis.
Results: No differences in GLP-1 users versus non-users with respect to all-cause hospitalization (HR 1.04, CI 0.85-1.28), IBD-hospitalization (HR 1.30, CI 0.90–1.88), IBD-related surgery (HR 0.49, CI 0.21–1.17), or pancreatitis (HR 0.74, CI 0.37-1.47) were seen. In the subgroup analysis, black GLP-1 users had an increased risk of all-cause hospitalizations (HR 1.59, CI 1.11–2.29) but not IBD-related hospitalization (HR 1.41, CI 0.78–2.56) or IBD-related surgery (HR 0.67, CI 0.14-3.13). Use of semaglutide reduced the risk of IBD-related surgery (HR 0.33, CI 0.13-0.83). Among 89 tirzepatide users, none required IBD related surgery versus 2 among matched controls, but this was not statistically significant. Rates of steroid use were low between groups (Table 1).
Discussion: Semaglutide use appeared to lower the risk of IBD-related surgery. Black patients using GLP-1 therapy had an increased risk of all-cause hospitalization, but not IBD-related hospitalization or surgery. Tirzepatide was not associated with net harms or benefits in the studied end points however there were few patients on this medicine. Overall, GLP-1 based therapies were well tolerated in this patient population. Further investigation with larger studies is warranted.
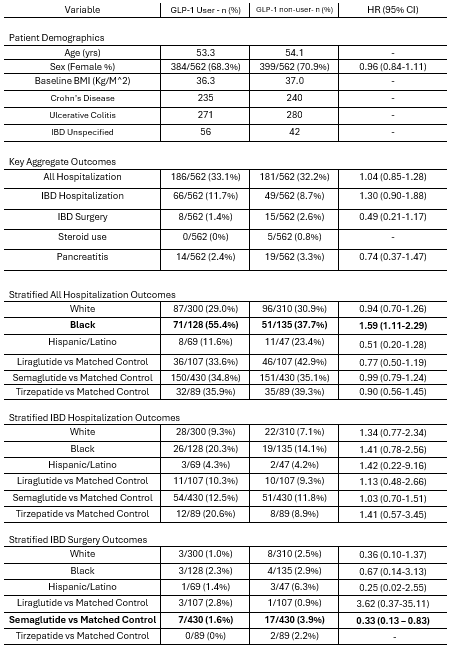
Figure: Table 1: Description of Demographics and Statistical Analysis -
HR= Hazard ratio; CI= Confidence interval; IBD=Inflammatory Bowel Disease; Sum of different GLP-1 agents is greater than 562 as some patients switched agents; Sum of self-identified race is less than 562 as some patients did not self-identify their race.
Disclosures:
Jake Levine indicated no relevant financial relationships.
Yao An Lee indicated no relevant financial relationships.
Angela Pham: Abbvie – Speakers Bureau. Janssen – Advisory Committee/Board Member. Pfizer Inc. – Grant/Research Support.
Amy Sheer: PeerView – Consultant.
Matthew Giansiracusa indicated no relevant financial relationships.
Serena Jingchuan Guo indicated no relevant financial relationships.
Hao Dai indicated no relevant financial relationships.
Rotana Radwan indicated no relevant financial relationships.
Jiang Bian indicated no relevant financial relationships.
Aleksey Novikov indicated no relevant financial relationships.
Jake Levine, MD1, Yao An Lee, BS2, Angela Pham, MD1, Amy Sheer, MD1, Matthew Giansiracusa, DO1, Serena Jingchuan O. Guo, MD, PhD2, Hao Dai, PhD3, Rotana Radwan, PhD2, Jiang Bian, PhD4, Aleksey Novikov, MD5. P5437 - Effect of Dual GLP-1/GIP and GLP-1 Agonists on Inflammatory Bowel Disease Activity Among Patients With Obesity, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Florida Health Shands Hospital, Gainesville, FL; 2Department of Pharmaceutical Outcomes and Policy, College of Pharmacy, University of Florida, Gainesville, FL, USA, Gainesville, FL; 3Department of Biostatistics & Health Data Science, Indiana University School of Medicine, Indianapolis, IN, USA, Indianapolis, IN; 4Regenstrief Institute, Indianapolis, IN, USA Department of Biostatistics & Health Data Science, Indiana University School of Medicine, Indianapolis, IN, USA Melvin and Bren Simon Comprehensive Cancer Center, Indiana University, Indianapolis, IN, USA, Gainesville, FL; 5University of Florida College of Medicine, Gainesville, FL
Introduction: Inflammatory bowel disease (IBD), either Crohn’s disease (CD) or ulcerative colitis (UC), is an autoimmune condition characterized by inflammation of GI tract. Obesity is a risk factor for IBD activity. Mounting evidence shows injectable incretins such as Glucagon-like peptide 1 (GLP-1) agonists cause weight loss and may improve IBD disease activity. Newer GLP-1 based agents like tirzepatide, which is a dual agonist of both GLP-1 and Glucose-dependent Insulinotropic Polypeptide (GIP), may have superior weight loss, but their effect on IBD is not known. In this study, we aimed to assess outcomes in patients with IBD and obesity with various GLP-1 medication use versus non-use.
Methods: A retrospective, propensity-matched analysis using data from The OneFlorida+ network from 2012-2023 was done. We evaluated patients with IBD and obesity prescribed GLP-1 based therapy (liraglutide, semaglutide, or tirzepatide) versus those without. 562 patients prescribed GLP-1 based therapies were matched 1:1 to controls based on age, sex, race, BMI, and comorbidities (n=1,124). The control group was time-matched based on GLP-1 users’ index prescription date and all patients were assessed at 12 months. The Cox proportional hazard model was used for analysis.
Results: No differences in GLP-1 users versus non-users with respect to all-cause hospitalization (HR 1.04, CI 0.85-1.28), IBD-hospitalization (HR 1.30, CI 0.90–1.88), IBD-related surgery (HR 0.49, CI 0.21–1.17), or pancreatitis (HR 0.74, CI 0.37-1.47) were seen. In the subgroup analysis, black GLP-1 users had an increased risk of all-cause hospitalizations (HR 1.59, CI 1.11–2.29) but not IBD-related hospitalization (HR 1.41, CI 0.78–2.56) or IBD-related surgery (HR 0.67, CI 0.14-3.13). Use of semaglutide reduced the risk of IBD-related surgery (HR 0.33, CI 0.13-0.83). Among 89 tirzepatide users, none required IBD related surgery versus 2 among matched controls, but this was not statistically significant. Rates of steroid use were low between groups (Table 1).
Discussion: Semaglutide use appeared to lower the risk of IBD-related surgery. Black patients using GLP-1 therapy had an increased risk of all-cause hospitalization, but not IBD-related hospitalization or surgery. Tirzepatide was not associated with net harms or benefits in the studied end points however there were few patients on this medicine. Overall, GLP-1 based therapies were well tolerated in this patient population. Further investigation with larger studies is warranted.
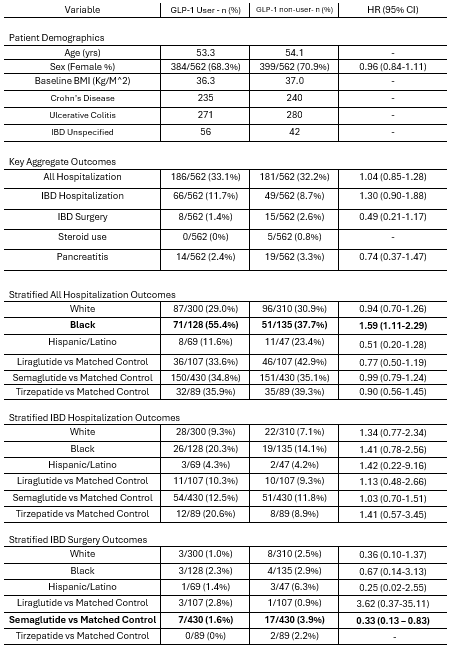
Figure: Table 1: Description of Demographics and Statistical Analysis -
HR= Hazard ratio; CI= Confidence interval; IBD=Inflammatory Bowel Disease; Sum of different GLP-1 agents is greater than 562 as some patients switched agents; Sum of self-identified race is less than 562 as some patients did not self-identify their race.
Disclosures:
Jake Levine indicated no relevant financial relationships.
Yao An Lee indicated no relevant financial relationships.
Angela Pham: Abbvie – Speakers Bureau. Janssen – Advisory Committee/Board Member. Pfizer Inc. – Grant/Research Support.
Amy Sheer: PeerView – Consultant.
Matthew Giansiracusa indicated no relevant financial relationships.
Serena Jingchuan Guo indicated no relevant financial relationships.
Hao Dai indicated no relevant financial relationships.
Rotana Radwan indicated no relevant financial relationships.
Jiang Bian indicated no relevant financial relationships.
Aleksey Novikov indicated no relevant financial relationships.
Jake Levine, MD1, Yao An Lee, BS2, Angela Pham, MD1, Amy Sheer, MD1, Matthew Giansiracusa, DO1, Serena Jingchuan O. Guo, MD, PhD2, Hao Dai, PhD3, Rotana Radwan, PhD2, Jiang Bian, PhD4, Aleksey Novikov, MD5. P5437 - Effect of Dual GLP-1/GIP and GLP-1 Agonists on Inflammatory Bowel Disease Activity Among Patients With Obesity, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

