Tuesday Poster Session
Category: IBD
P5406 - Prevalence and Risk Factors for Vitamin C Deficiency in Patients With Inflammatory Bowel Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- WB
William Breaux, MD
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
William Breaux, MD, Nicole Ruiz, MD, Kathryn Thompson, MD, Hayalneh Gessessew, MD
Emory University School of Medicine, Atlanta, GA
Introduction: Vitamin C plays a vital role in immune function, collagen production, iron absorption and antioxidant defense. Patients with inflammatory bowel disease (IBD) are at increased risk for micronutrient deficiencies due to chronic inflammation, malabsorption, and dietary restrictions. There is limited data on the prevalence and risk factors of vitamin C deficiency and its impact in patients with IBD. The aim of this study is to evaluate the prevalence of vitamin C deficiency in patients with IBD along with associated risk factors and correlation with IBD disease severity.
Methods: A retrospective chart review was completed on adult patients (ages 18-85) with IBD treated at Emory University Hospital clinic sites who had serum vitamin C levels drawn between December 2019 to September 2024. Vitamin C was considered deficient if the serum level was below 23 umol/L. IBD disease severity was classified based on provider assessment using tools such as the Harvey-Bradshaw Index and the Partial Mayo Score. Body mass index (BMI) was categorized as underweight (< 20), normal weight (20-25) and overweight ( >25). Comparisons of categorical variables were performed using Chi-squared test. Statistical analyses included chi-square testing and logistic regression, with p< 0.05 considered significant.
Results: Out of 433 screened patients, 230 met inclusion criteria. Table 1 highlights the baseline characteristics between the two population groups (those with vitamin C deficiency and those without). Seventy-four (32.2%) were found to have vitamin C deficiency, with a mean serum level of 13.6 in the vitamin C deficient group. No significant correlation was found between vitamin C deficiency and IBD disease severity. Subjects who were overweight were significantly more likely to have vitamin C deficiency compared to normal or underweight patients (OR 2.27, 95% CI 1.19, 4.31, p=0.01). Active smokers were also more likely to be vitamin C deficient (OR 4.74, 95% CI 1.81, 12.40, p=0.002).
Discussion: Vitamin C deficiency was prevalent in almost one third of the study population. Modifiable lifestyle factors, such as smoking and elevated BMI, were identified as significant risk factors. There was notably no correlation found between Vitamin C deficiency and disease severity. These findings highlight the importance of routine assessment of Vitamin C in patients with IBD, especially those with modifiable risk factors, to help improve health outcomes.
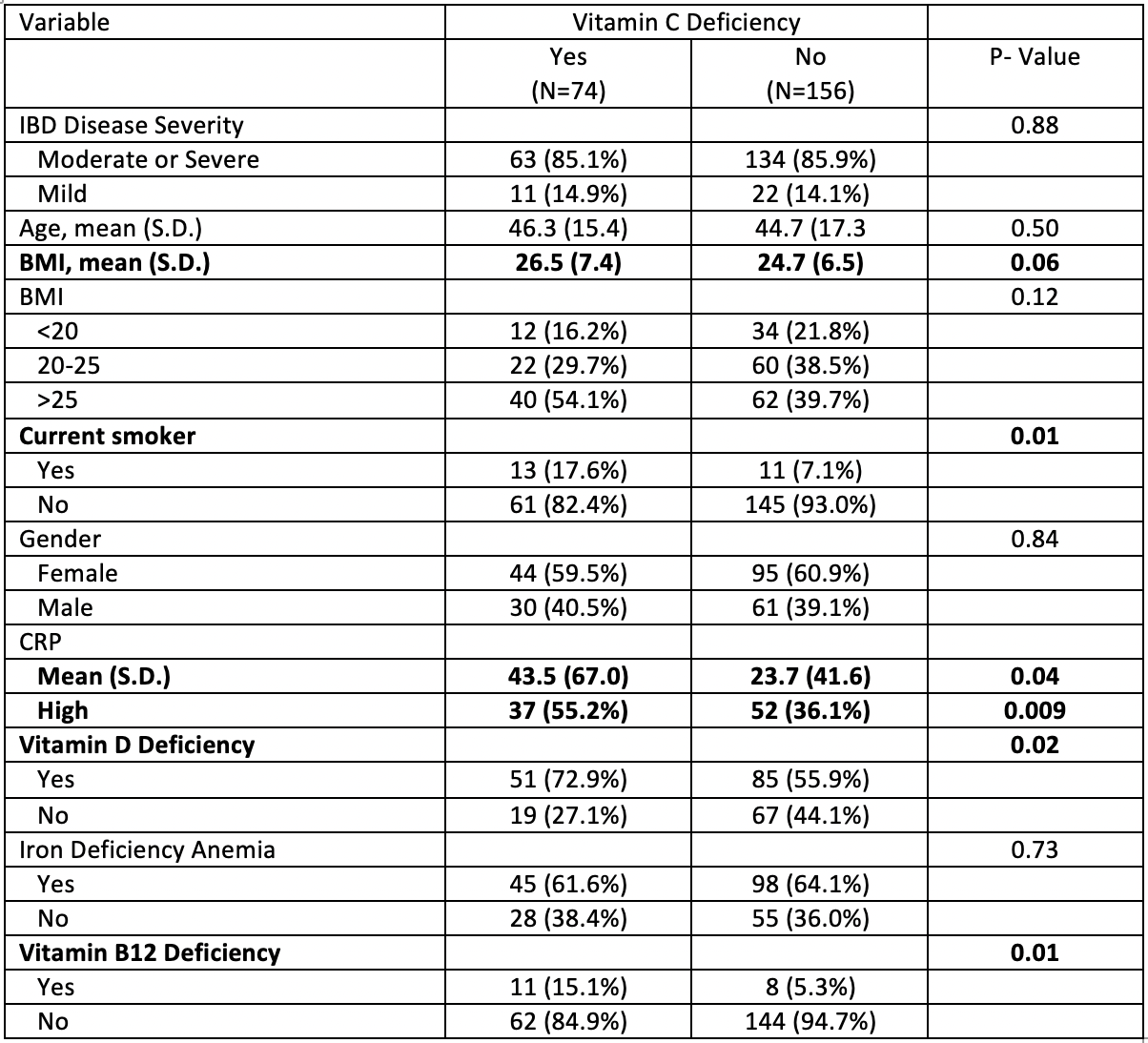
Figure: Descriptive comparison between patients with and without vitamin C deficiency.
Disclosures:
William Breaux indicated no relevant financial relationships.
Nicole Ruiz indicated no relevant financial relationships.
Kathryn Thompson indicated no relevant financial relationships.
Hayalneh Gessessew indicated no relevant financial relationships.
William Breaux, MD, Nicole Ruiz, MD, Kathryn Thompson, MD, Hayalneh Gessessew, MD. P5406 - Prevalence and Risk Factors for Vitamin C Deficiency in Patients With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Emory University School of Medicine, Atlanta, GA
Introduction: Vitamin C plays a vital role in immune function, collagen production, iron absorption and antioxidant defense. Patients with inflammatory bowel disease (IBD) are at increased risk for micronutrient deficiencies due to chronic inflammation, malabsorption, and dietary restrictions. There is limited data on the prevalence and risk factors of vitamin C deficiency and its impact in patients with IBD. The aim of this study is to evaluate the prevalence of vitamin C deficiency in patients with IBD along with associated risk factors and correlation with IBD disease severity.
Methods: A retrospective chart review was completed on adult patients (ages 18-85) with IBD treated at Emory University Hospital clinic sites who had serum vitamin C levels drawn between December 2019 to September 2024. Vitamin C was considered deficient if the serum level was below 23 umol/L. IBD disease severity was classified based on provider assessment using tools such as the Harvey-Bradshaw Index and the Partial Mayo Score. Body mass index (BMI) was categorized as underweight (< 20), normal weight (20-25) and overweight ( >25). Comparisons of categorical variables were performed using Chi-squared test. Statistical analyses included chi-square testing and logistic regression, with p< 0.05 considered significant.
Results: Out of 433 screened patients, 230 met inclusion criteria. Table 1 highlights the baseline characteristics between the two population groups (those with vitamin C deficiency and those without). Seventy-four (32.2%) were found to have vitamin C deficiency, with a mean serum level of 13.6 in the vitamin C deficient group. No significant correlation was found between vitamin C deficiency and IBD disease severity. Subjects who were overweight were significantly more likely to have vitamin C deficiency compared to normal or underweight patients (OR 2.27, 95% CI 1.19, 4.31, p=0.01). Active smokers were also more likely to be vitamin C deficient (OR 4.74, 95% CI 1.81, 12.40, p=0.002).
Discussion: Vitamin C deficiency was prevalent in almost one third of the study population. Modifiable lifestyle factors, such as smoking and elevated BMI, were identified as significant risk factors. There was notably no correlation found between Vitamin C deficiency and disease severity. These findings highlight the importance of routine assessment of Vitamin C in patients with IBD, especially those with modifiable risk factors, to help improve health outcomes.
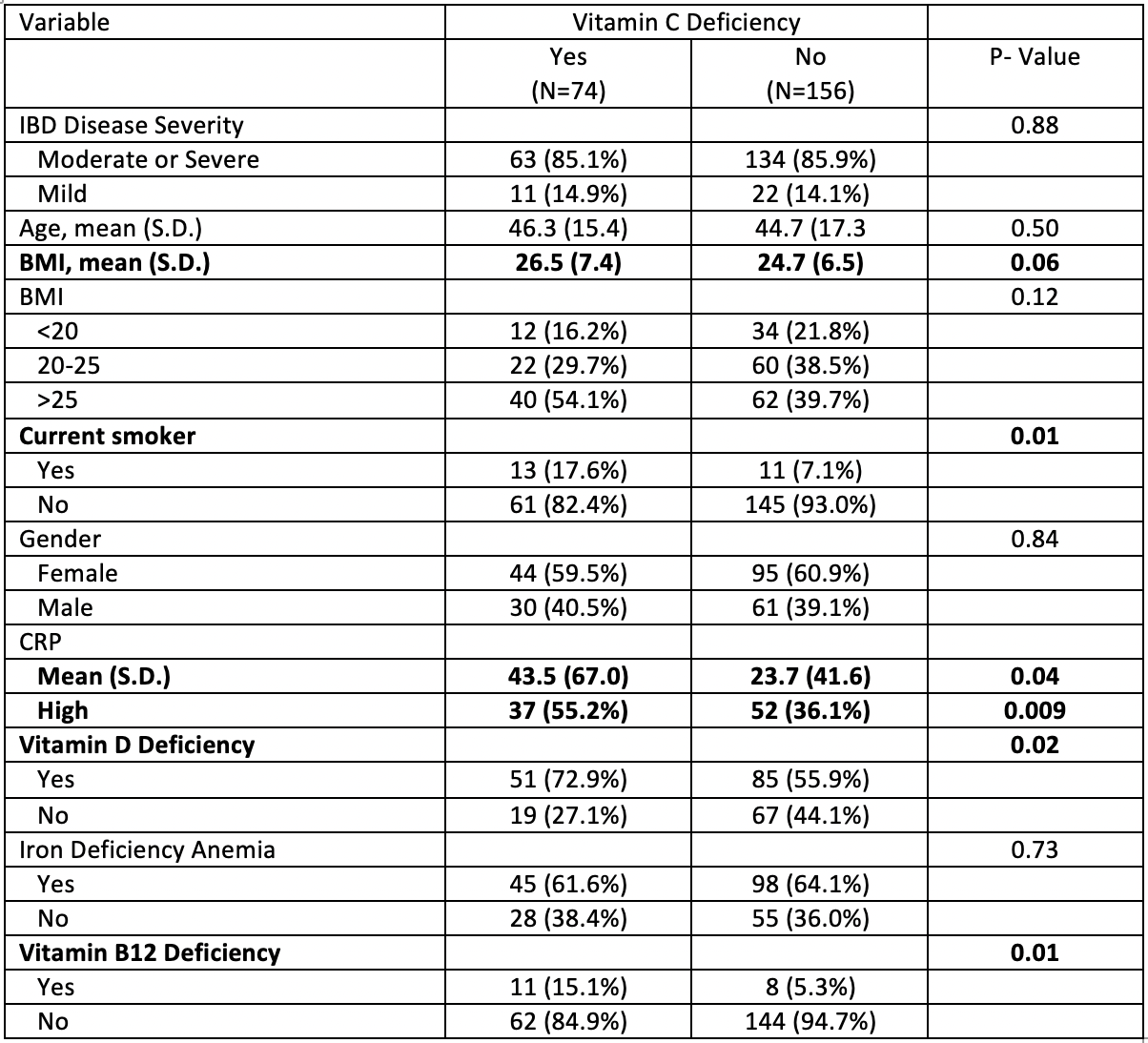
Figure: Descriptive comparison between patients with and without vitamin C deficiency.
Disclosures:
William Breaux indicated no relevant financial relationships.
Nicole Ruiz indicated no relevant financial relationships.
Kathryn Thompson indicated no relevant financial relationships.
Hayalneh Gessessew indicated no relevant financial relationships.
William Breaux, MD, Nicole Ruiz, MD, Kathryn Thompson, MD, Hayalneh Gessessew, MD. P5406 - Prevalence and Risk Factors for Vitamin C Deficiency in Patients With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
