Tuesday Poster Session
Category: IBD
P5405 - Vaccination Prevalence in Patients With Inflammatory Bowel Disease: A Community Hospital Perspective
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Panisara Fangsaard, MD
Bassett Medical Center
Cooperstown, NY
Presenting Author(s)
Panisara Fangsaard, MD1, Trairat Unteng, MD1, Kannate Chotiphansiri, MD1, Abolfazl Ahmady, MD1, Nikita Srivalsan, MD1, Natchaya Polpichai, MD2, Amber Charoen, MD3, Edward Bischof, MD1, Carmine Catalano, MD1
1Bassett Medical Center, Cooperstown, NY; 2Division of gastroenterology/hepatology, Medical College of Georgia at Augusta University, Chicago, IL; 3Washington State University (WSU), Pullman, WA
Introduction: Patients with inflammatory diseases (IBD) are at higher risk of severe vaccine-preventable diseases, particularly those receiving immunosuppressants. Previous studies have shown suboptimal vaccination rates in this special population. One contributing factor is the lack of clearly defined responsibility among healthcare providers. This study aims to address these knowledge gaps in the setting of a community hospital.
Methods: We conducted a retrospective chart review of patients with IBD who were treated with biologics or immunomodulators during the study period. Patients were seen in either the primary care (PC) or gastroenterology (GI) clinic between 2022 and 2024 across Bassett Healthcare Network. Immunization records for influenza vaccination (IFV) were obtained over 2 seasons (2022-2023 and 2023-2024). Other vaccine records, including COVID-19 vaccination (CVV), pneumococcal pneumonia vaccination (PPV), and zoster vaccination (ZTV), were included without time restriction. Types of prescribers, including PCP, GI, and others, were also analyzed.
Results: Of the total 502 patient records reviewed, 328 (65.3%) met the inclusion criteria. Demographic data are summarized in Table 1. The highest vaccination rates are noted in CVV at 81.4%, followed by PPV at 58.3%, IFV at 54.3%, and ZTV at 29.1%, as demonstrated in Table 2. Across all vaccines, PC was the predominant prescriber, followed by others, then GI. Over 70% of IFV were prescribed by PC in both seasons, with one shot (1.2%) given by GI. For PPV, PC prescribed 71.4% of the dose 1 alone, 82.4% of the first dose, and 90.2% of the second dose among two-dose recipients. For ZTV, a relatively even distribution of prescribers was observed between PC and others, 55% and 45%, respectively. Prescriber data for CVV was not analyzed due to confounding documentation.
Discussion: Although over half of IBD patients received CVV, IFV, and PPV, nearly 50% were unvaccinated. These low rates of immunization are significantly noted in ZTV. These findings suggest the persistent low prevalence of vaccination in IBD patients and emphasize a critical gap in preventive care. While the vaccine prescriber distribution underscores the curtail role of PC, there is an opportunity for GI to contribute more. These findings suggest the need for collaboration between PC and GI to enhance vaccination rates in this high-risk population.
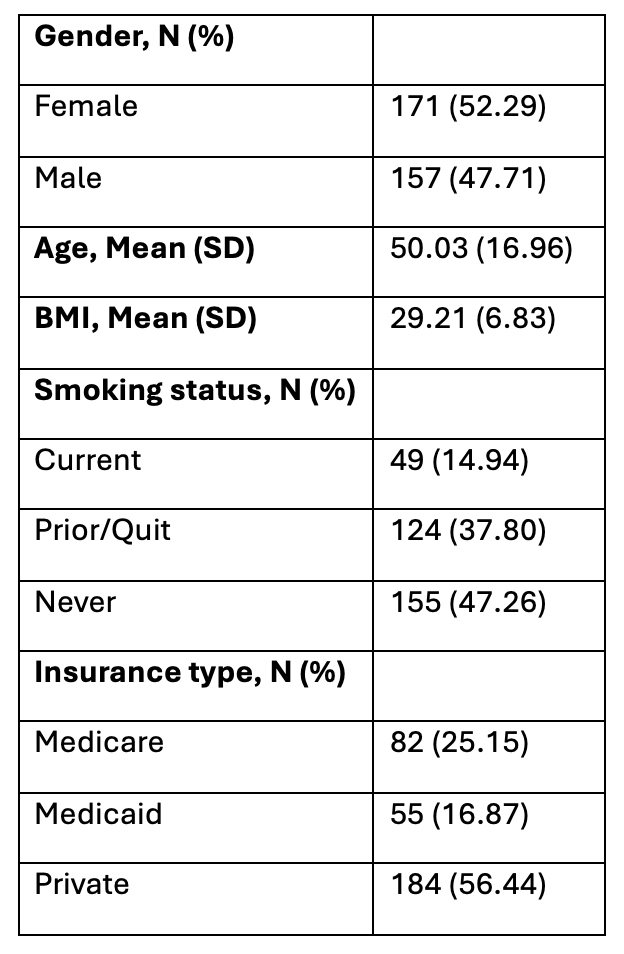
Figure: Table 1. Demographic data

Figure: Table 2. Vaccination rates and provider type distribution
Disclosures:
Panisara Fangsaard indicated no relevant financial relationships.
Trairat Unteng indicated no relevant financial relationships.
Kannate Chotiphansiri indicated no relevant financial relationships.
Abolfazl Ahmady indicated no relevant financial relationships.
Nikita Srivalsan indicated no relevant financial relationships.
Natchaya Polpichai indicated no relevant financial relationships.
Amber Charoen indicated no relevant financial relationships.
Edward Bischof indicated no relevant financial relationships.
Carmine Catalano indicated no relevant financial relationships.
Panisara Fangsaard, MD1, Trairat Unteng, MD1, Kannate Chotiphansiri, MD1, Abolfazl Ahmady, MD1, Nikita Srivalsan, MD1, Natchaya Polpichai, MD2, Amber Charoen, MD3, Edward Bischof, MD1, Carmine Catalano, MD1. P5405 - Vaccination Prevalence in Patients With Inflammatory Bowel Disease: A Community Hospital Perspective, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Bassett Medical Center, Cooperstown, NY; 2Division of gastroenterology/hepatology, Medical College of Georgia at Augusta University, Chicago, IL; 3Washington State University (WSU), Pullman, WA
Introduction: Patients with inflammatory diseases (IBD) are at higher risk of severe vaccine-preventable diseases, particularly those receiving immunosuppressants. Previous studies have shown suboptimal vaccination rates in this special population. One contributing factor is the lack of clearly defined responsibility among healthcare providers. This study aims to address these knowledge gaps in the setting of a community hospital.
Methods: We conducted a retrospective chart review of patients with IBD who were treated with biologics or immunomodulators during the study period. Patients were seen in either the primary care (PC) or gastroenterology (GI) clinic between 2022 and 2024 across Bassett Healthcare Network. Immunization records for influenza vaccination (IFV) were obtained over 2 seasons (2022-2023 and 2023-2024). Other vaccine records, including COVID-19 vaccination (CVV), pneumococcal pneumonia vaccination (PPV), and zoster vaccination (ZTV), were included without time restriction. Types of prescribers, including PCP, GI, and others, were also analyzed.
Results: Of the total 502 patient records reviewed, 328 (65.3%) met the inclusion criteria. Demographic data are summarized in Table 1. The highest vaccination rates are noted in CVV at 81.4%, followed by PPV at 58.3%, IFV at 54.3%, and ZTV at 29.1%, as demonstrated in Table 2. Across all vaccines, PC was the predominant prescriber, followed by others, then GI. Over 70% of IFV were prescribed by PC in both seasons, with one shot (1.2%) given by GI. For PPV, PC prescribed 71.4% of the dose 1 alone, 82.4% of the first dose, and 90.2% of the second dose among two-dose recipients. For ZTV, a relatively even distribution of prescribers was observed between PC and others, 55% and 45%, respectively. Prescriber data for CVV was not analyzed due to confounding documentation.
Discussion: Although over half of IBD patients received CVV, IFV, and PPV, nearly 50% were unvaccinated. These low rates of immunization are significantly noted in ZTV. These findings suggest the persistent low prevalence of vaccination in IBD patients and emphasize a critical gap in preventive care. While the vaccine prescriber distribution underscores the curtail role of PC, there is an opportunity for GI to contribute more. These findings suggest the need for collaboration between PC and GI to enhance vaccination rates in this high-risk population.
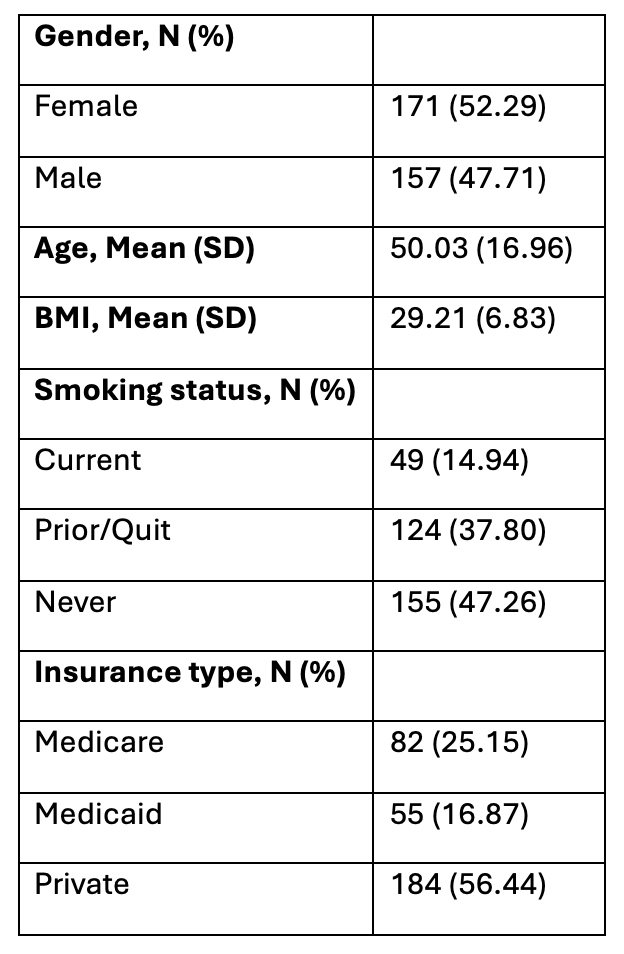
Figure: Table 1. Demographic data

Figure: Table 2. Vaccination rates and provider type distribution
Disclosures:
Panisara Fangsaard indicated no relevant financial relationships.
Trairat Unteng indicated no relevant financial relationships.
Kannate Chotiphansiri indicated no relevant financial relationships.
Abolfazl Ahmady indicated no relevant financial relationships.
Nikita Srivalsan indicated no relevant financial relationships.
Natchaya Polpichai indicated no relevant financial relationships.
Amber Charoen indicated no relevant financial relationships.
Edward Bischof indicated no relevant financial relationships.
Carmine Catalano indicated no relevant financial relationships.
Panisara Fangsaard, MD1, Trairat Unteng, MD1, Kannate Chotiphansiri, MD1, Abolfazl Ahmady, MD1, Nikita Srivalsan, MD1, Natchaya Polpichai, MD2, Amber Charoen, MD3, Edward Bischof, MD1, Carmine Catalano, MD1. P5405 - Vaccination Prevalence in Patients With Inflammatory Bowel Disease: A Community Hospital Perspective, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
