Tuesday Poster Session
Category: IBD
P5401 - Impact of Proton Pump Inhibitors and NSAIDs on the Risk of Pouchitis Following Ileal Pouch-Anal Anastomosis in Ulcerative Colitis: A Propensity-Matched Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Saqr Alsakarneh, MD, MS (he/him/his)
Mayo Clinic
Rochester, MN
Presenting Author(s)
Saqr Alsakarneh, MD, MS1, Razan Aburumman, MD2, Abdulla Massad, MD3, Edward L. Barnes, MD, MPH4, Francis A.. Farraye, MD, MSc, MACG5, Maia Kayal, MD6, Jana G. Hashash, MD, MSc, FACG5
1Mayo Clinic, Kansas City, MO; 2Henry Ford Health, Detroit, MI; 3University of Texas Medical Branch, Galveston, TX; 4Multidisciplinary Inflammatory Bowel Diseases Center, Division of Gastroenterology and Hepatology, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, Chapel Hill, NC; 5Mayo Clinic, Jacksonville, FL; 6Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Up to 30% of patients with ulcerative colitis (UC) eventually require colectomy with ileal pouch-anal anastomosis (IPAA). Acute pouchitis is a common complication, affecting up to 70% of these patients. Medications such as proton pump inhibitors (PPIs) and nonsteroidal anti-inflammatory drugs (NSAIDs) have been implicated in gut microbiome alterations, potentially influencing pouchitis development. We aimed to evaluate the association between PPI versus NSAID use and the risk of pouchitis in UC patients undergoing IPAA.
Methods: We conducted a retrospective cohort study using the TriNetX database, which includes de-identified electronic health records from over 125 million patients across 71 healthcare organizations in the United States. Adult UC patients who underwent IPAA were identified using ICD-10 codes. We included patients with documented use of PPIs or NSAIDs within three months post-IPAA. Propensity score matching (1:1) was applied to balance baseline characteristics between cohorts. The primary outcome was the incidence of first-time pouchitis within two years of surgery.
Results: After matching, 1,714 patients in the PPI cohort were compared with 1,714 patients in the NSAID cohort. At 2-year follow-up, 945 patients (55.1%) in the PPI group and 990 patients (57.8%) in the NSAID group developed pouchitis. There was no statistically significant difference in the risk of pouchitis between the groups (adjusted hazard ratio [aHR]: 0.97; 95% CI: 0.84–1.00; p = 0.05) (Figure 1). Findings were consistent across 6-month, 9-month, and 1-year follow-up intervals. However, when compared with patients who were not on PPI or NSAID, patient on PPI (aHR = 1.50; 95% CI: 1.28–1.76; p < 0.001) as well as NSAID (aHR = 1.73; 95% CI: 1.48–2.02; p < 0.001) were at higher risk of developing pouchitis.
Discussion: In this large, real-world cohort of UC patients who underwent IPAA, PPI and NSAID were associated with a significantly increased risk of developing pouchitis compared to patients who did not have exposure to any of them. These findings suggest that PPI or NSAID exposure shortly after IPAA may independently impact pouchitis risk. Further prospective studies are needed to explore the underlying mechanisms and to validate these results.
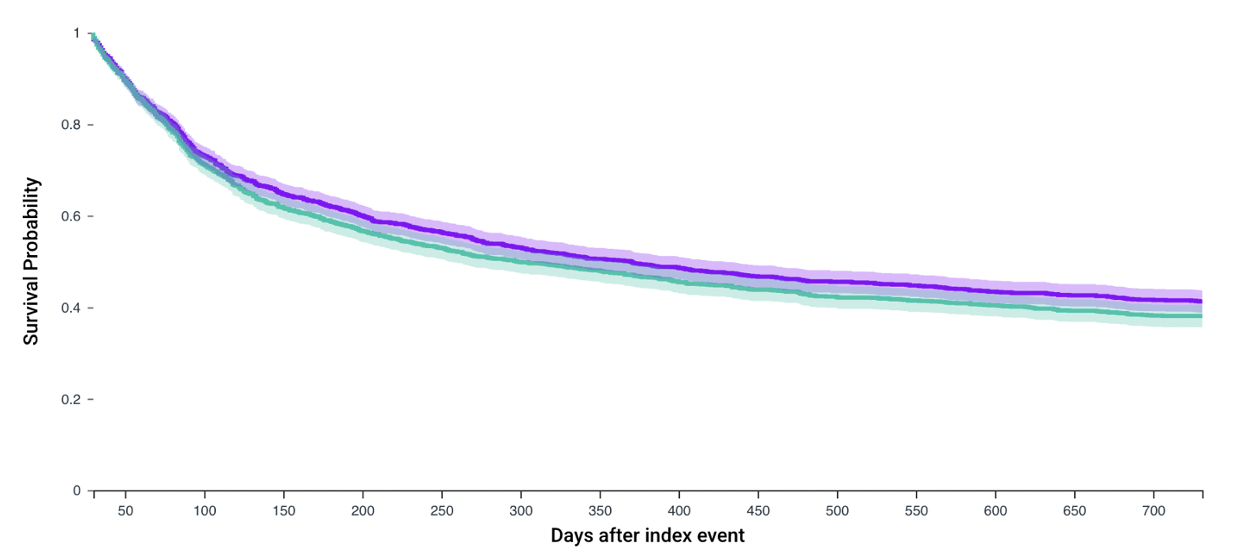
Figure: Figure 1. Kaplan-Meier curve demonstrating the cumulative incidence of pouchitis in the two study groups. There was no statistically significant difference in the risk of pouchitis between the groups.
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Abdulla Massad indicated no relevant financial relationships.
Edward Barnes: AbbVie, Inc. – Consultant. Boomerang – Consultant. Eli Lilly – Consultant. Eli Lilly – Grant/Research Support. Pfizer – Consultant. Sanofi – Consultant. Takeda – Consultant. Target RWE – Consultant.
Francis Farraye: Astellas – Advisory Committee/Board Member. Avalo – Advisory Committee/Board Member. Bausch – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member, Stock Options. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Maia Kayal: Abbvie – Consultant. Johnson&Johnson – Consultant. Pfizer – Consultant. Takeda – Consultant.
Jana Hashash: BMS – Ad Board.
Saqr Alsakarneh, MD, MS1, Razan Aburumman, MD2, Abdulla Massad, MD3, Edward L. Barnes, MD, MPH4, Francis A.. Farraye, MD, MSc, MACG5, Maia Kayal, MD6, Jana G. Hashash, MD, MSc, FACG5. P5401 - Impact of Proton Pump Inhibitors and NSAIDs on the Risk of Pouchitis Following Ileal Pouch-Anal Anastomosis in Ulcerative Colitis: A Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Kansas City, MO; 2Henry Ford Health, Detroit, MI; 3University of Texas Medical Branch, Galveston, TX; 4Multidisciplinary Inflammatory Bowel Diseases Center, Division of Gastroenterology and Hepatology, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, Chapel Hill, NC; 5Mayo Clinic, Jacksonville, FL; 6Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Up to 30% of patients with ulcerative colitis (UC) eventually require colectomy with ileal pouch-anal anastomosis (IPAA). Acute pouchitis is a common complication, affecting up to 70% of these patients. Medications such as proton pump inhibitors (PPIs) and nonsteroidal anti-inflammatory drugs (NSAIDs) have been implicated in gut microbiome alterations, potentially influencing pouchitis development. We aimed to evaluate the association between PPI versus NSAID use and the risk of pouchitis in UC patients undergoing IPAA.
Methods: We conducted a retrospective cohort study using the TriNetX database, which includes de-identified electronic health records from over 125 million patients across 71 healthcare organizations in the United States. Adult UC patients who underwent IPAA were identified using ICD-10 codes. We included patients with documented use of PPIs or NSAIDs within three months post-IPAA. Propensity score matching (1:1) was applied to balance baseline characteristics between cohorts. The primary outcome was the incidence of first-time pouchitis within two years of surgery.
Results: After matching, 1,714 patients in the PPI cohort were compared with 1,714 patients in the NSAID cohort. At 2-year follow-up, 945 patients (55.1%) in the PPI group and 990 patients (57.8%) in the NSAID group developed pouchitis. There was no statistically significant difference in the risk of pouchitis between the groups (adjusted hazard ratio [aHR]: 0.97; 95% CI: 0.84–1.00; p = 0.05) (Figure 1). Findings were consistent across 6-month, 9-month, and 1-year follow-up intervals. However, when compared with patients who were not on PPI or NSAID, patient on PPI (aHR = 1.50; 95% CI: 1.28–1.76; p < 0.001) as well as NSAID (aHR = 1.73; 95% CI: 1.48–2.02; p < 0.001) were at higher risk of developing pouchitis.
Discussion: In this large, real-world cohort of UC patients who underwent IPAA, PPI and NSAID were associated with a significantly increased risk of developing pouchitis compared to patients who did not have exposure to any of them. These findings suggest that PPI or NSAID exposure shortly after IPAA may independently impact pouchitis risk. Further prospective studies are needed to explore the underlying mechanisms and to validate these results.
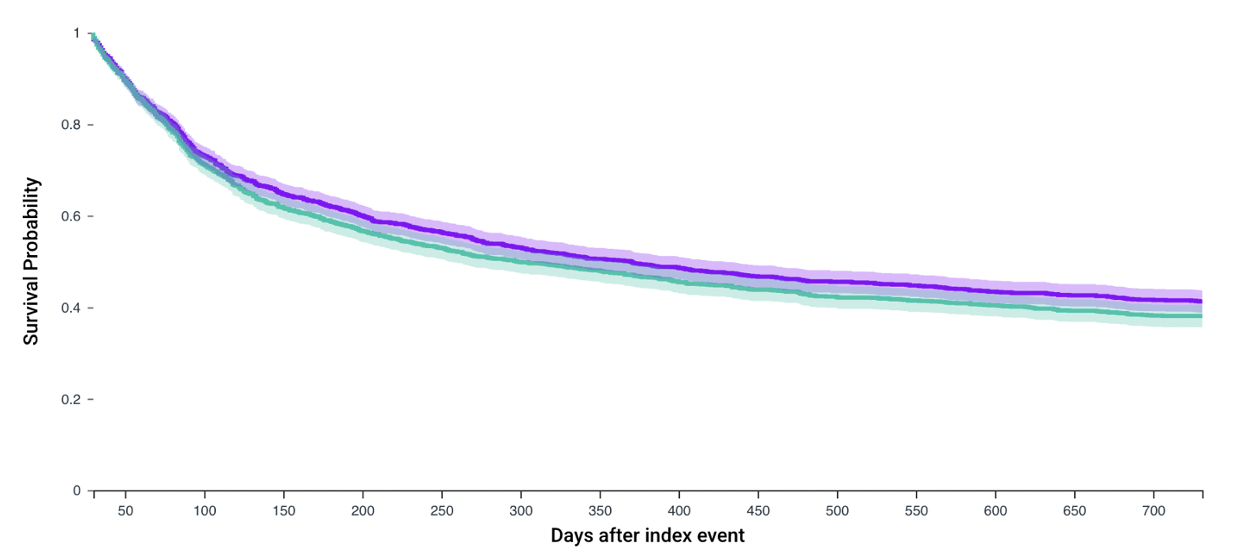
Figure: Figure 1. Kaplan-Meier curve demonstrating the cumulative incidence of pouchitis in the two study groups. There was no statistically significant difference in the risk of pouchitis between the groups.
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Abdulla Massad indicated no relevant financial relationships.
Edward Barnes: AbbVie, Inc. – Consultant. Boomerang – Consultant. Eli Lilly – Consultant. Eli Lilly – Grant/Research Support. Pfizer – Consultant. Sanofi – Consultant. Takeda – Consultant. Target RWE – Consultant.
Francis Farraye: Astellas – Advisory Committee/Board Member. Avalo – Advisory Committee/Board Member. Bausch – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member, Stock Options. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Maia Kayal: Abbvie – Consultant. Johnson&Johnson – Consultant. Pfizer – Consultant. Takeda – Consultant.
Jana Hashash: BMS – Ad Board.
Saqr Alsakarneh, MD, MS1, Razan Aburumman, MD2, Abdulla Massad, MD3, Edward L. Barnes, MD, MPH4, Francis A.. Farraye, MD, MSc, MACG5, Maia Kayal, MD6, Jana G. Hashash, MD, MSc, FACG5. P5401 - Impact of Proton Pump Inhibitors and NSAIDs on the Risk of Pouchitis Following Ileal Pouch-Anal Anastomosis in Ulcerative Colitis: A Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
