Tuesday Poster Session
Category: IBD
Increased Risk of <i>De Novo</i> Inflammatory Bowel Disease Following Cholecystectomy: A Population-Based Cohort Study
P5400 - Increased Risk of De Novo Inflammatory Bowel Disease Following Cholecystectomy: A Population-Based Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Saqr Alsakarneh, MD, MS (he/him/his)
Mayo Clinic
Rochester, MN
Presenting Author(s)
Saqr Alsakarneh, MD, MS1, Razan Aburumman, MD2, June Tome, MD3, Abdulla Massad, MD4, Michael Camilleri, MD, DSc3, Francis A.. Farraye, MD, MSc, MACG5, Jana G. Hashash, MD, MSc, FACG5
1Mayo Clinic, Kansas City, MO; 2Henry Ford Health, Detroit, MI; 3Mayo Clinic, Rochester, MN; 4University of Texas Medical Branch, Galveston, TX; 5Mayo Clinic, Jacksonville, FL
Introduction: Cholecystectomy may alter bile acid circulation, leading to changes in intestinal permeability, mucosal inflammation, and gut microbiota composition. While associations with post-cholecystectomy microscopic colitis and bile acid diarrhea are reported, its impact on the incidence of inflammatory bowel disease (IBD) remains unclear. We aimed to assess the risk of de novo IBD following cholecystectomy using a large national database.
Methods: We conducted a retrospective cohort study using the TriNetX electronic health record network from 2010 to 2024. Adult patients (≥18 years) who underwent cholecystectomy were matched 1:1 to controls without cholecystectomy using propensity score matching based on demographics, comorbidities, and medication exposures (Table 1). Patients with a prior history of IBD were excluded from the analysis. The primary outcome was the risk of developing De Novo IBD from index event. Secondary outcomes included risk of ulcerative colitis (UC) and Crohn’s disease (CD), and subgroup analyses based on predictors including age, sex, and comorbidities and medications exposure. With censoring applied, Kaplan-Meier analysis with hazard ratios (HRs) and 95% CIs were used to compare time-to-event rates at daily time intervals.
Results: A total of 570,317 patients with cholecystectomy were matched to 570,317 controls (Table 1). Cholecystectomy was associated with a higher risk of de novo IBD (aHR: 1.29, 95% CI: 1.22–1.35; p< 0.001), driven predominantly by the increased risk of CD (aHR: 1.83, 95% CI: 1.69–1.99; p< 0.001) [Table 2]. Stratified analyses showed elevated IBD risk in both males (aHR: 1.26) and females (aHR: 1.21), with CD risk higher in males (aHR: 1.99) than females (aHR: 1.73). The greatest risk was observed in patients aged 18–60 years (aHR: 1.33, 95% CI: 1.24–1.42).
Among clinical factors, tobacco use conferred the highest IBD risk (aHR: 1.43, 95% CI: 1.19–1.76; p< 0.001) and was the only factor significantly associated with UC (aHR: 1.29, 95% CI: 1.03–1.62; p=0.03). Diabetes, obesity, aspirin, and NSAID use were also associated with increased CD risk, while UC remained nonsignificant in these subgroups.
Discussion: Cholecystectomy is independently associated with an increased risk of de novo IBD, primarily driven by Crohn’s disease. Tobacco use emerged as the only modifiable factor significantly linked to UC. These findings highlight the need for increased clinical awareness and surveillance for IBD following cholecystectomy.
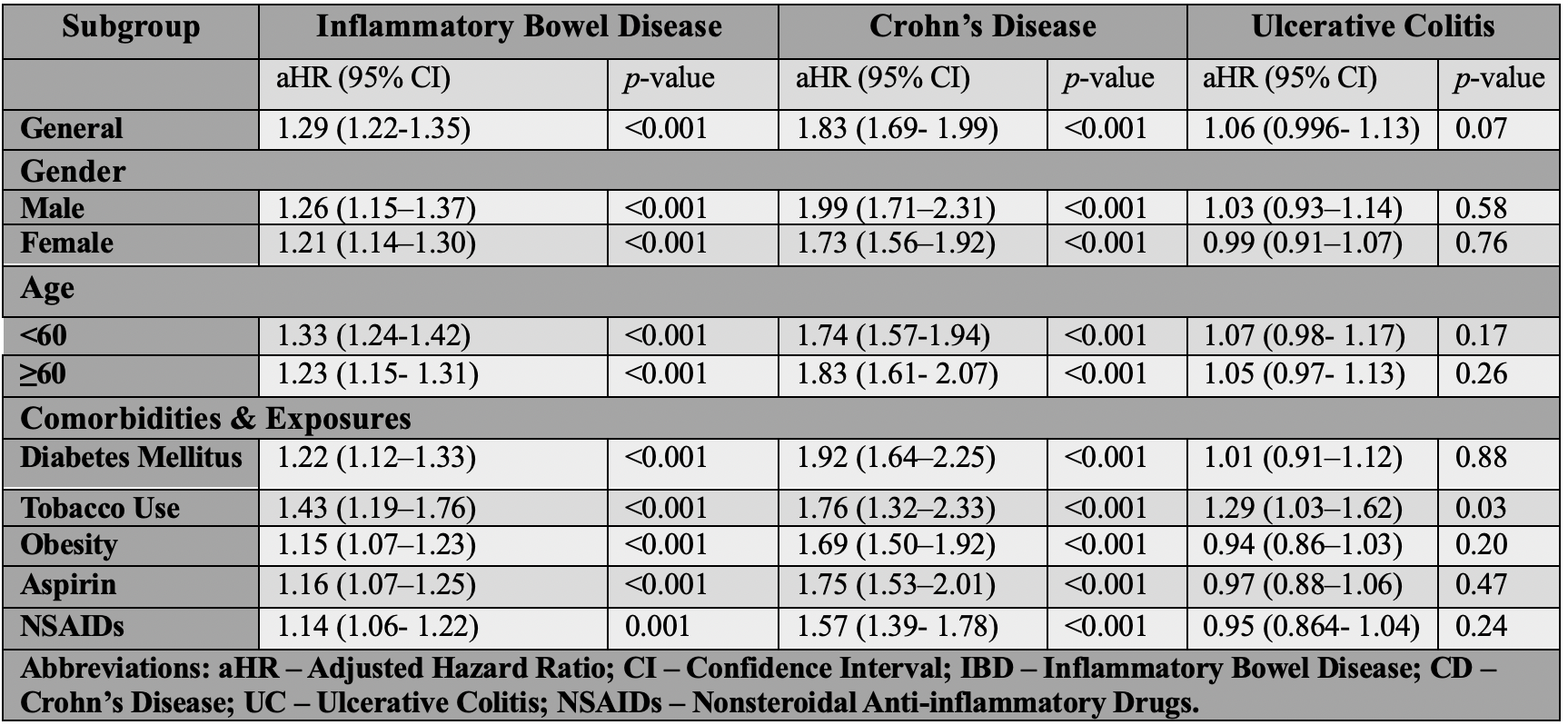
Figure: Table 1: Baseline Characteristics Before and After Propensity Score Matching Between Patients with and Without Cholecystectomy
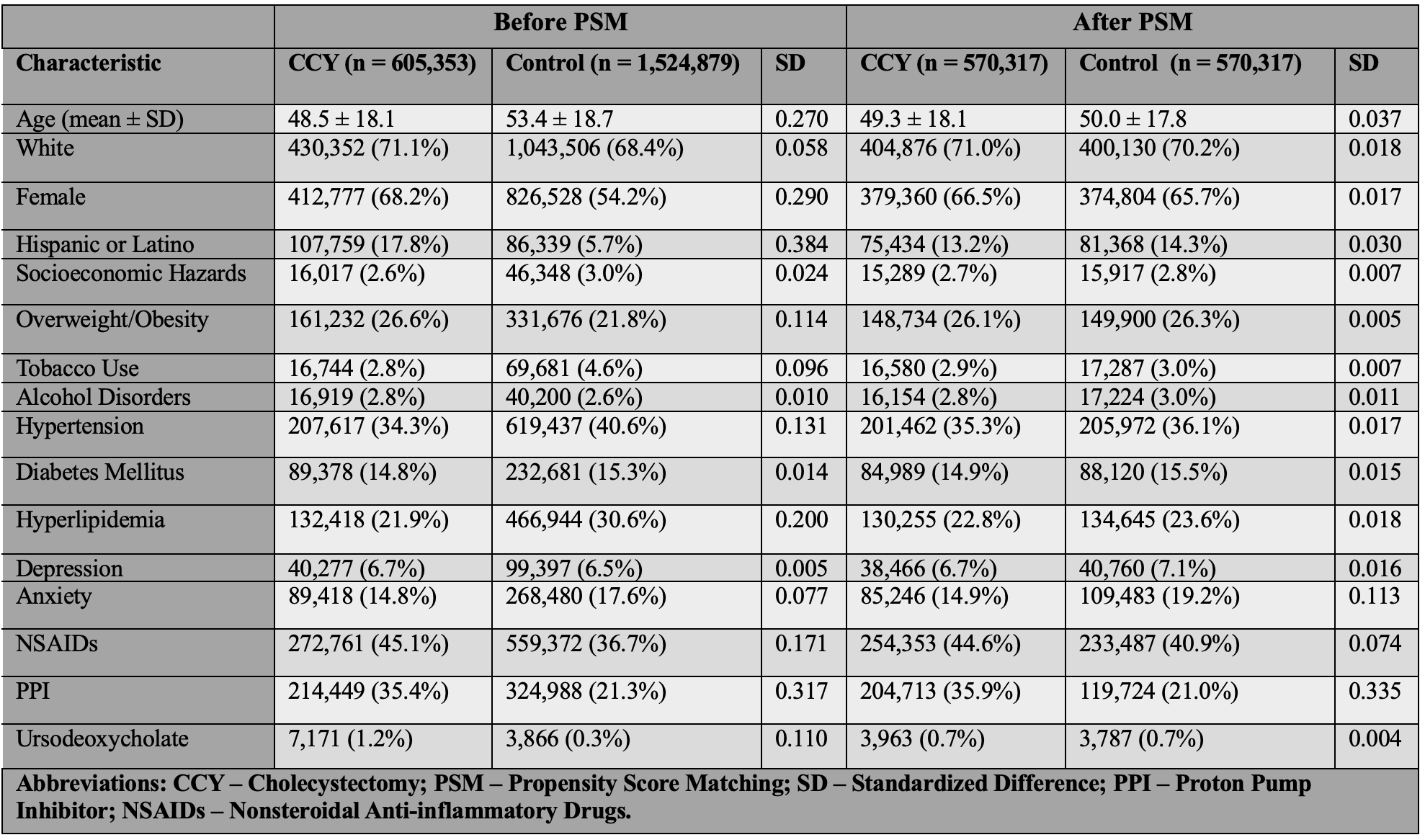
Figure: Table 2: Adjusted Hazard Ratios for Inflammatory Bowel Disease, Crohn’s Disease, and Ulcerative Colitis Following Cholecystectomy: Subgroup Analysis by Demographics and Clinical Factors
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
June Tome indicated no relevant financial relationships.
Abdulla Massad indicated no relevant financial relationships.
Michael Camilleri: Alfasigma – Consultant. Amylyx – Consultant. Biocodex – Grant/Research Support. BioKier – Consultant. Brightseed Bio – Consultant, Grant/Research Support. Coloplast – Consultant. Dignify Therapeutics – Stock Options. Intercept – Consultant. Invea – Consultant. Kallyope – Consultant. McDermott Will & Emery – Consultant. Medpace – Consultant. Monteresearch – Consultant. Neurogastrx – Consultant. NGM Biopharmaceuticals – Grant/Research Support. Pfizer – Grant/Research Support. Phenomix – Stock Options. Renexxion – Consultant. SKYE Bioscience – Consultant. Sumitomo – Consultant. Synlogic – Consultant. Vanda – Grant/Research Support.
Francis Farraye: Astellas – Advisory Committee/Board Member. Avalo – Advisory Committee/Board Member. Bausch – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member, Stock Options. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Jana Hashash: BMS – Ad Board.
Saqr Alsakarneh, MD, MS1, Razan Aburumman, MD2, June Tome, MD3, Abdulla Massad, MD4, Michael Camilleri, MD, DSc3, Francis A.. Farraye, MD, MSc, MACG5, Jana G. Hashash, MD, MSc, FACG5. P5400 - Increased Risk of <i>De Novo</i> Inflammatory Bowel Disease Following Cholecystectomy: A Population-Based Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Kansas City, MO; 2Henry Ford Health, Detroit, MI; 3Mayo Clinic, Rochester, MN; 4University of Texas Medical Branch, Galveston, TX; 5Mayo Clinic, Jacksonville, FL
Introduction: Cholecystectomy may alter bile acid circulation, leading to changes in intestinal permeability, mucosal inflammation, and gut microbiota composition. While associations with post-cholecystectomy microscopic colitis and bile acid diarrhea are reported, its impact on the incidence of inflammatory bowel disease (IBD) remains unclear. We aimed to assess the risk of de novo IBD following cholecystectomy using a large national database.
Methods: We conducted a retrospective cohort study using the TriNetX electronic health record network from 2010 to 2024. Adult patients (≥18 years) who underwent cholecystectomy were matched 1:1 to controls without cholecystectomy using propensity score matching based on demographics, comorbidities, and medication exposures (Table 1). Patients with a prior history of IBD were excluded from the analysis. The primary outcome was the risk of developing De Novo IBD from index event. Secondary outcomes included risk of ulcerative colitis (UC) and Crohn’s disease (CD), and subgroup analyses based on predictors including age, sex, and comorbidities and medications exposure. With censoring applied, Kaplan-Meier analysis with hazard ratios (HRs) and 95% CIs were used to compare time-to-event rates at daily time intervals.
Results: A total of 570,317 patients with cholecystectomy were matched to 570,317 controls (Table 1). Cholecystectomy was associated with a higher risk of de novo IBD (aHR: 1.29, 95% CI: 1.22–1.35; p< 0.001), driven predominantly by the increased risk of CD (aHR: 1.83, 95% CI: 1.69–1.99; p< 0.001) [Table 2]. Stratified analyses showed elevated IBD risk in both males (aHR: 1.26) and females (aHR: 1.21), with CD risk higher in males (aHR: 1.99) than females (aHR: 1.73). The greatest risk was observed in patients aged 18–60 years (aHR: 1.33, 95% CI: 1.24–1.42).
Among clinical factors, tobacco use conferred the highest IBD risk (aHR: 1.43, 95% CI: 1.19–1.76; p< 0.001) and was the only factor significantly associated with UC (aHR: 1.29, 95% CI: 1.03–1.62; p=0.03). Diabetes, obesity, aspirin, and NSAID use were also associated with increased CD risk, while UC remained nonsignificant in these subgroups.
Discussion: Cholecystectomy is independently associated with an increased risk of de novo IBD, primarily driven by Crohn’s disease. Tobacco use emerged as the only modifiable factor significantly linked to UC. These findings highlight the need for increased clinical awareness and surveillance for IBD following cholecystectomy.
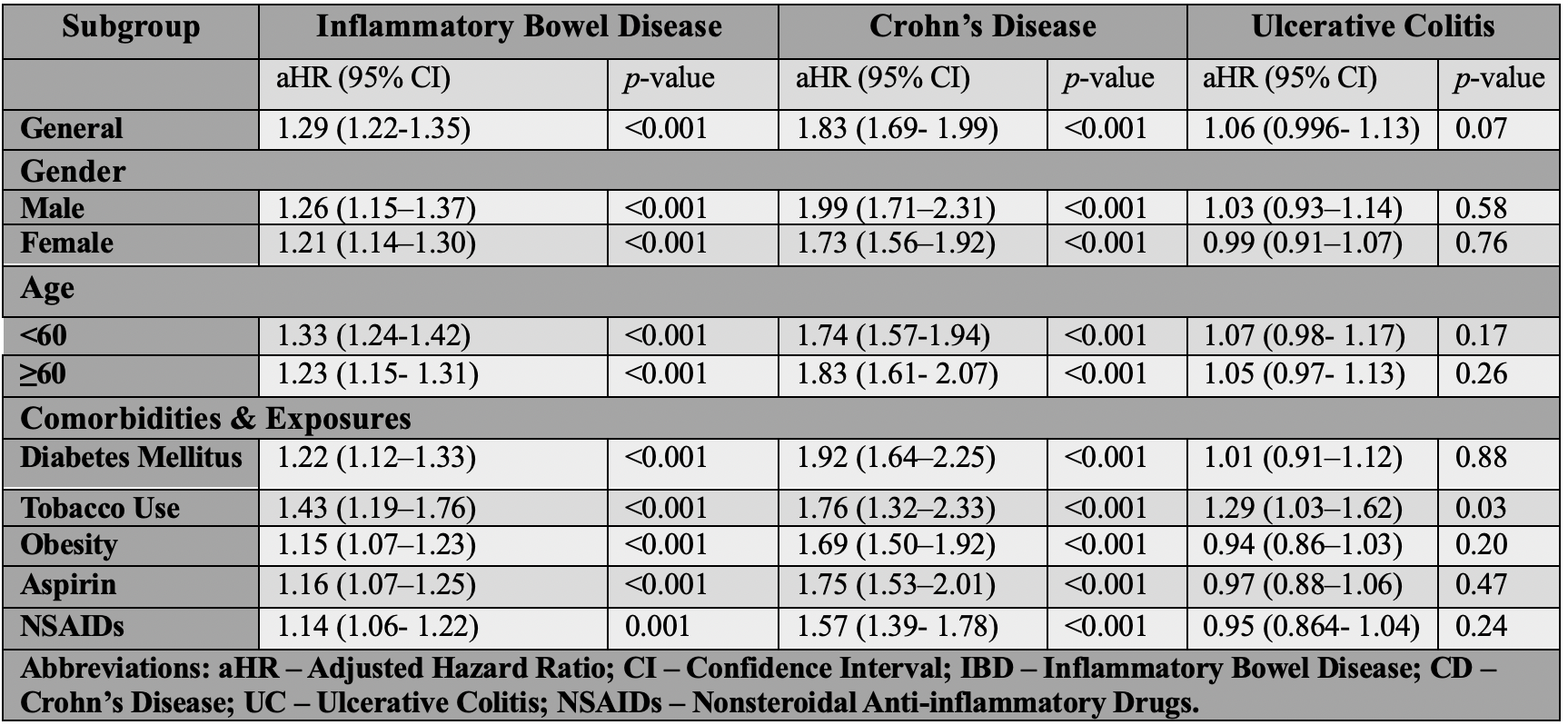
Figure: Table 1: Baseline Characteristics Before and After Propensity Score Matching Between Patients with and Without Cholecystectomy
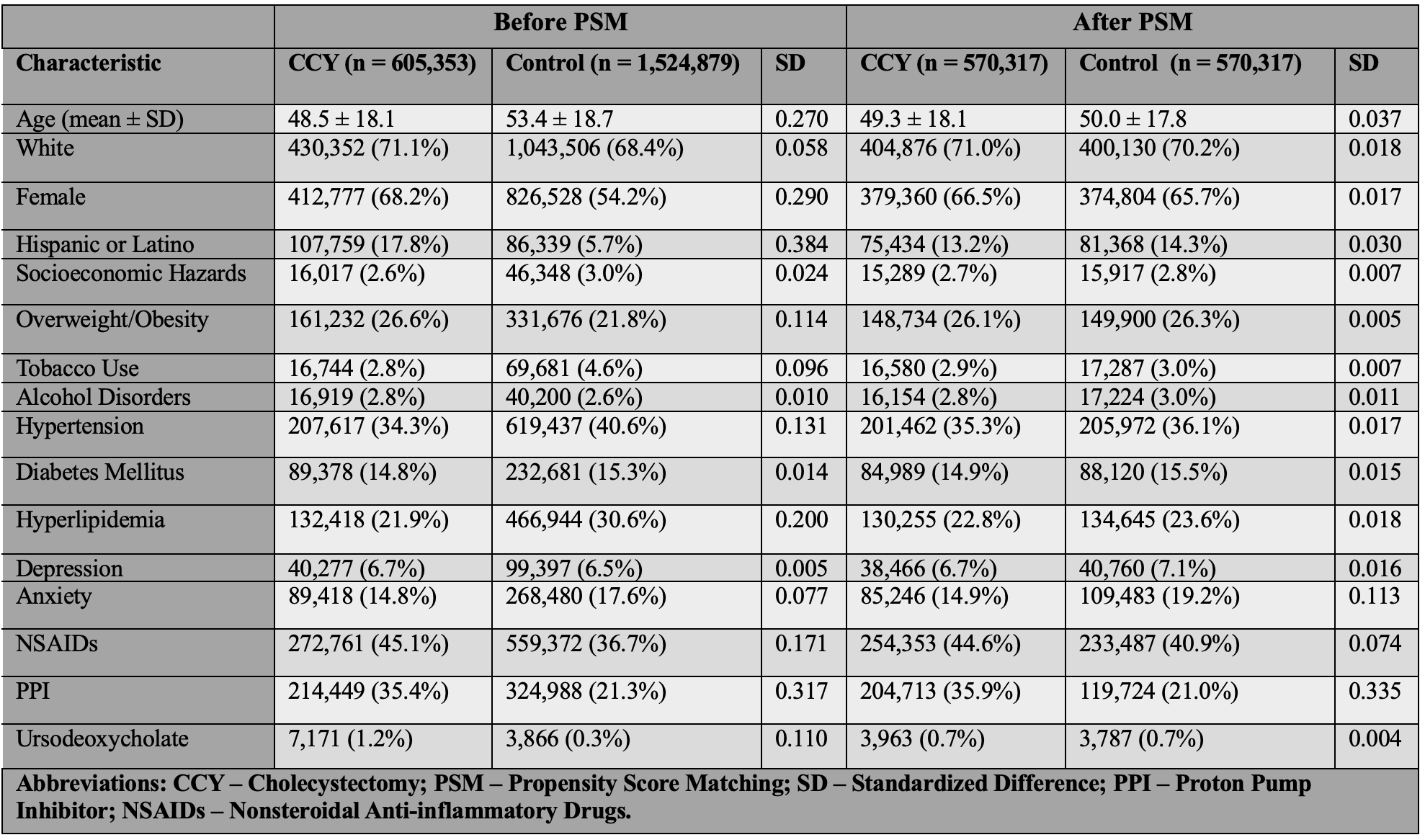
Figure: Table 2: Adjusted Hazard Ratios for Inflammatory Bowel Disease, Crohn’s Disease, and Ulcerative Colitis Following Cholecystectomy: Subgroup Analysis by Demographics and Clinical Factors
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
June Tome indicated no relevant financial relationships.
Abdulla Massad indicated no relevant financial relationships.
Michael Camilleri: Alfasigma – Consultant. Amylyx – Consultant. Biocodex – Grant/Research Support. BioKier – Consultant. Brightseed Bio – Consultant, Grant/Research Support. Coloplast – Consultant. Dignify Therapeutics – Stock Options. Intercept – Consultant. Invea – Consultant. Kallyope – Consultant. McDermott Will & Emery – Consultant. Medpace – Consultant. Monteresearch – Consultant. Neurogastrx – Consultant. NGM Biopharmaceuticals – Grant/Research Support. Pfizer – Grant/Research Support. Phenomix – Stock Options. Renexxion – Consultant. SKYE Bioscience – Consultant. Sumitomo – Consultant. Synlogic – Consultant. Vanda – Grant/Research Support.
Francis Farraye: Astellas – Advisory Committee/Board Member. Avalo – Advisory Committee/Board Member. Bausch – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member, Stock Options. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Jana Hashash: BMS – Ad Board.
Saqr Alsakarneh, MD, MS1, Razan Aburumman, MD2, June Tome, MD3, Abdulla Massad, MD4, Michael Camilleri, MD, DSc3, Francis A.. Farraye, MD, MSc, MACG5, Jana G. Hashash, MD, MSc, FACG5. P5400 - Increased Risk of <i>De Novo</i> Inflammatory Bowel Disease Following Cholecystectomy: A Population-Based Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
