Tuesday Poster Session
Category: IBD
P5399 - Postoperative Complications After Appendectomy in Ulcerative Colitis: A National Inpatient Cohort Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Isaac Giovannie, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Giovannie Isaac-Coss, MD1, Meghana Kakarla, MD2, Patricia Ziegler, MD1, Joseph Frasca, MD1, Maham Lodhi, MD1, Veena Nannegari, MD3, Atsushi Sakuraba, MD, PhD1
1Rush University Medical Center, Chicago, IL; 2Infirmary Health, Mobile, AL; 3Rush University Medical Center, Chicagoii, IL
Introduction: While appendectomy typically has low risk of complications, patients with ulcerative colitis (UC) may have increased odds of adverse postoperative outcomes due to chronic inflammation, immunosuppressive therapy, and malnutrition. Despite these concerns, no large-scale U.S. study has assessed whether UC independently contributes to greater odds of complications or mortality following appendectomy. We evaluated appendectomy outcomes in UC patients using national inpatient data.
Methods: We conducted a retrospective cohort study using the 2018–2021 National Inpatient Sample. Adults (≥18 years) undergoing appendectomy were identified with ICD-10 codes (0DTJ0ZZ, 0DTJ4ZZ, 0DTJ8ZZ); UC was identified via K51.x codes. Primary and secondary outcomes were postoperative complications and in-hospital mortality. Complications were categorized by system (Table 1). Multivariable logistic regression adjusted for age, sex, race/ethnicity, and income. Due to unavailable present-on-admission flags, all complications were assumed postoperative. National estimates were generated using NIS sampling weights.
Results: Among 140,836 appendectomy hospitalizations, 433 (0.3%) involved UC. UC was independently associated with higher odds of any complication (aOR 1.33, 95% CI 1.07–1.65, p=0.01), compared to non-UC patients. A non-significant increase in odds of in-hospital mortality was observed (aOR 2.23, 95% CI 0.91–5.43, p=0.078). UC patients had significantly higher odds of sepsis (aOR 1.88, p=0.004), postop delirium (aOR 3.67, p=0.002), and malnutrition or weight loss (aOR 3.53, p< 0.001). Non-significant trends were noted for pneumonia, ileus, AKI and abscess. Female sex was associated with lower odds of complications and mortality compared to males (aORs 0.73 and 0.75, respectively, p< 0.001). Each year of age increased odds of complications by 3% and mortality by 5% (p< 0.001). Higher income quartile was associated with lower odds of both outcomes. African American patients had higher odds of complications (aOR 1.49) and mortality (aOR 1.77, p< 0.001) compared to non-AA.
Discussion: UC is associated with significantly greater odds of postop complications following appendectomy, particularly for sepsis, delirium, and malnutrition. These findings suggest the importance of tailored perioperative strategies in UC, including nutritional support and multidisciplinary planning. Despite limitations of administrative data, this study underscores the importance of individualized surgical planning in UC populations.
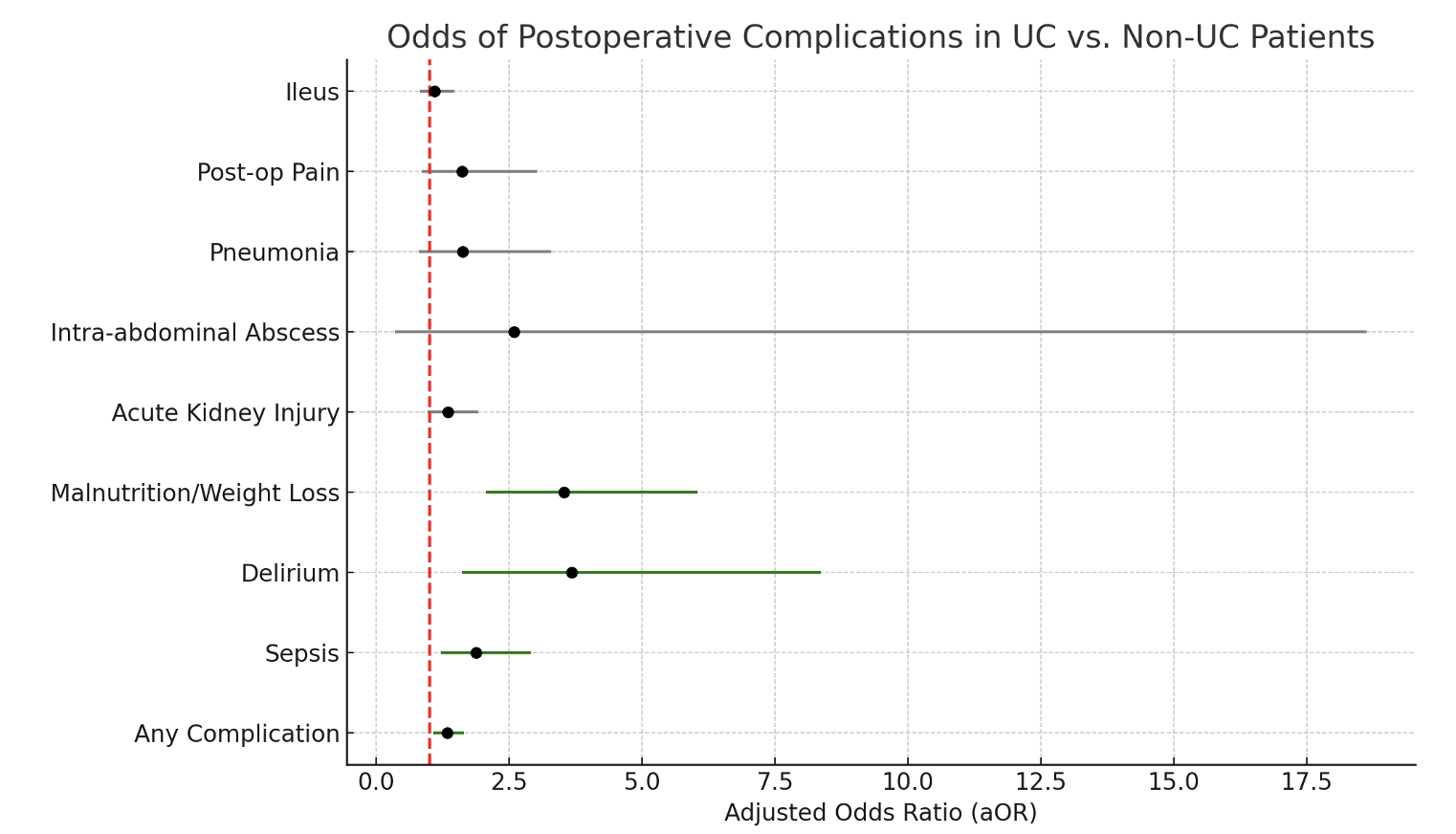
Figure: Adjusted odds ratios (aOR) and 95% confidence intervals for postoperative complications in patients with ulcerative colitis (UC) compared to non-UC patients undergoing appendectomy, based on a national inpatient sample (2018–2021). Green markers indicate statistically significant associations (p < 0.05); gray markers represent non-significant trends. Red dashed line denotes null value (aOR = 1).
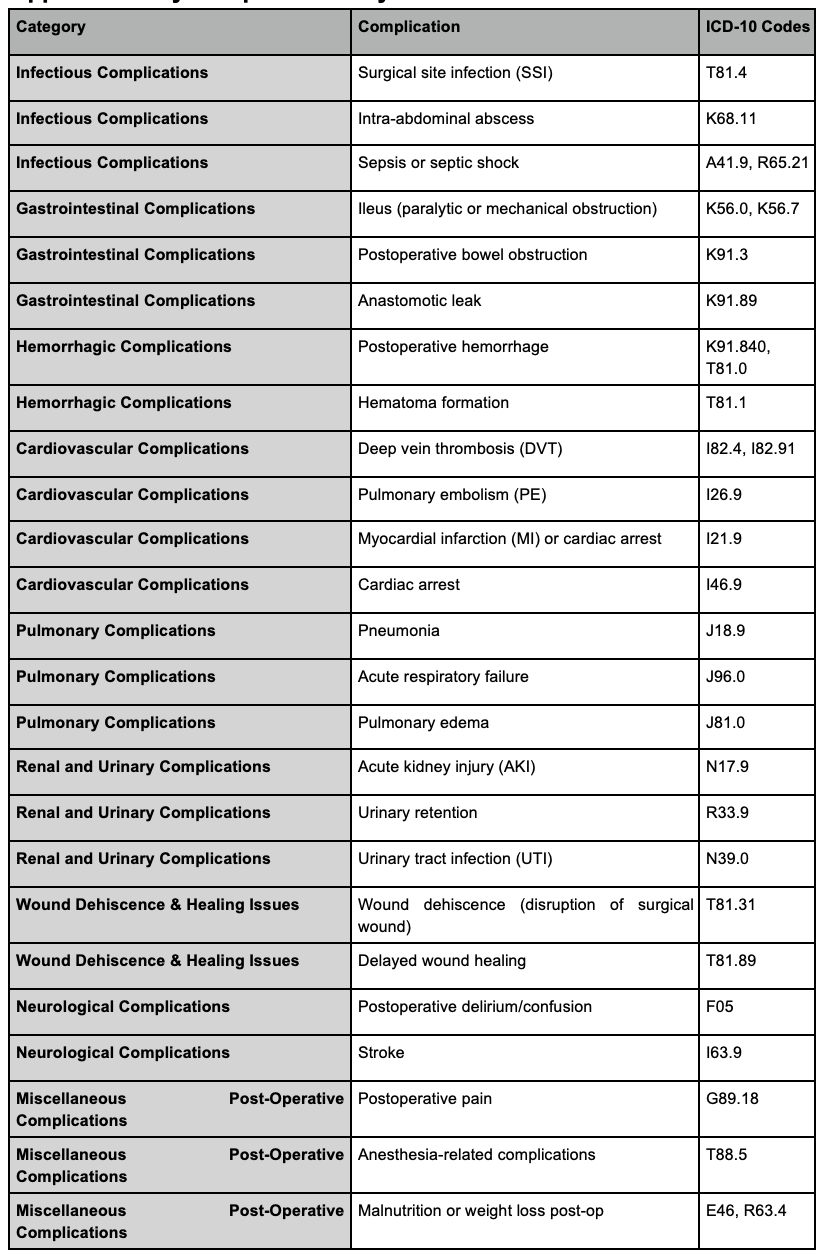
Figure: Table 1: Appendectomy complications by UC status ICD-10 codes
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Meghana Kakarla indicated no relevant financial relationships.
Patricia Ziegler indicated no relevant financial relationships.
Joseph Frasca indicated no relevant financial relationships.
Maham Lodhi indicated no relevant financial relationships.
Veena Nannegari indicated no relevant financial relationships.
Atsushi Sakuraba indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Meghana Kakarla, MD2, Patricia Ziegler, MD1, Joseph Frasca, MD1, Maham Lodhi, MD1, Veena Nannegari, MD3, Atsushi Sakuraba, MD, PhD1. P5399 - Postoperative Complications After Appendectomy in Ulcerative Colitis: A National Inpatient Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rush University Medical Center, Chicago, IL; 2Infirmary Health, Mobile, AL; 3Rush University Medical Center, Chicagoii, IL
Introduction: While appendectomy typically has low risk of complications, patients with ulcerative colitis (UC) may have increased odds of adverse postoperative outcomes due to chronic inflammation, immunosuppressive therapy, and malnutrition. Despite these concerns, no large-scale U.S. study has assessed whether UC independently contributes to greater odds of complications or mortality following appendectomy. We evaluated appendectomy outcomes in UC patients using national inpatient data.
Methods: We conducted a retrospective cohort study using the 2018–2021 National Inpatient Sample. Adults (≥18 years) undergoing appendectomy were identified with ICD-10 codes (0DTJ0ZZ, 0DTJ4ZZ, 0DTJ8ZZ); UC was identified via K51.x codes. Primary and secondary outcomes were postoperative complications and in-hospital mortality. Complications were categorized by system (Table 1). Multivariable logistic regression adjusted for age, sex, race/ethnicity, and income. Due to unavailable present-on-admission flags, all complications were assumed postoperative. National estimates were generated using NIS sampling weights.
Results: Among 140,836 appendectomy hospitalizations, 433 (0.3%) involved UC. UC was independently associated with higher odds of any complication (aOR 1.33, 95% CI 1.07–1.65, p=0.01), compared to non-UC patients. A non-significant increase in odds of in-hospital mortality was observed (aOR 2.23, 95% CI 0.91–5.43, p=0.078). UC patients had significantly higher odds of sepsis (aOR 1.88, p=0.004), postop delirium (aOR 3.67, p=0.002), and malnutrition or weight loss (aOR 3.53, p< 0.001). Non-significant trends were noted for pneumonia, ileus, AKI and abscess. Female sex was associated with lower odds of complications and mortality compared to males (aORs 0.73 and 0.75, respectively, p< 0.001). Each year of age increased odds of complications by 3% and mortality by 5% (p< 0.001). Higher income quartile was associated with lower odds of both outcomes. African American patients had higher odds of complications (aOR 1.49) and mortality (aOR 1.77, p< 0.001) compared to non-AA.
Discussion: UC is associated with significantly greater odds of postop complications following appendectomy, particularly for sepsis, delirium, and malnutrition. These findings suggest the importance of tailored perioperative strategies in UC, including nutritional support and multidisciplinary planning. Despite limitations of administrative data, this study underscores the importance of individualized surgical planning in UC populations.
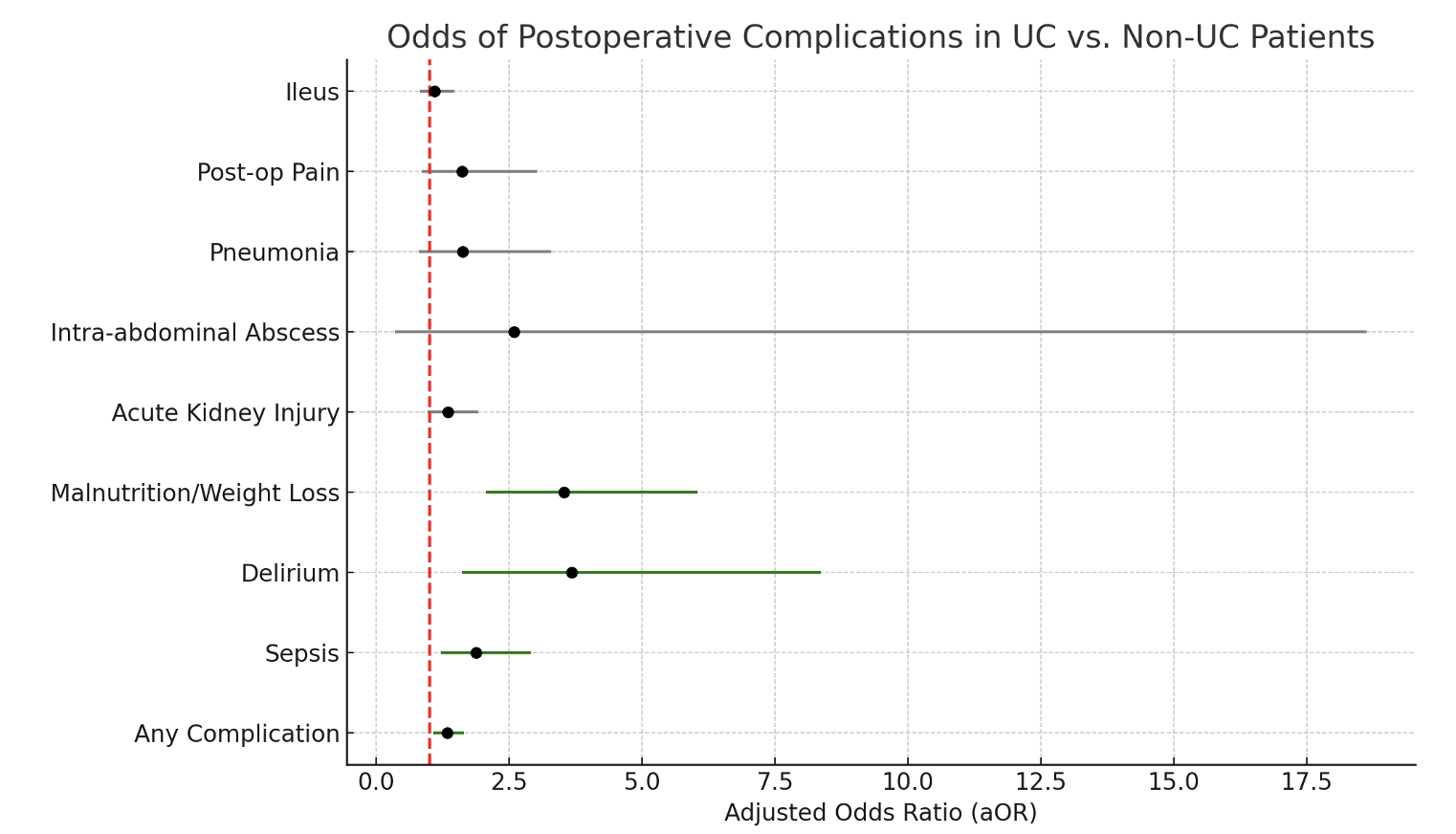
Figure: Adjusted odds ratios (aOR) and 95% confidence intervals for postoperative complications in patients with ulcerative colitis (UC) compared to non-UC patients undergoing appendectomy, based on a national inpatient sample (2018–2021). Green markers indicate statistically significant associations (p < 0.05); gray markers represent non-significant trends. Red dashed line denotes null value (aOR = 1).
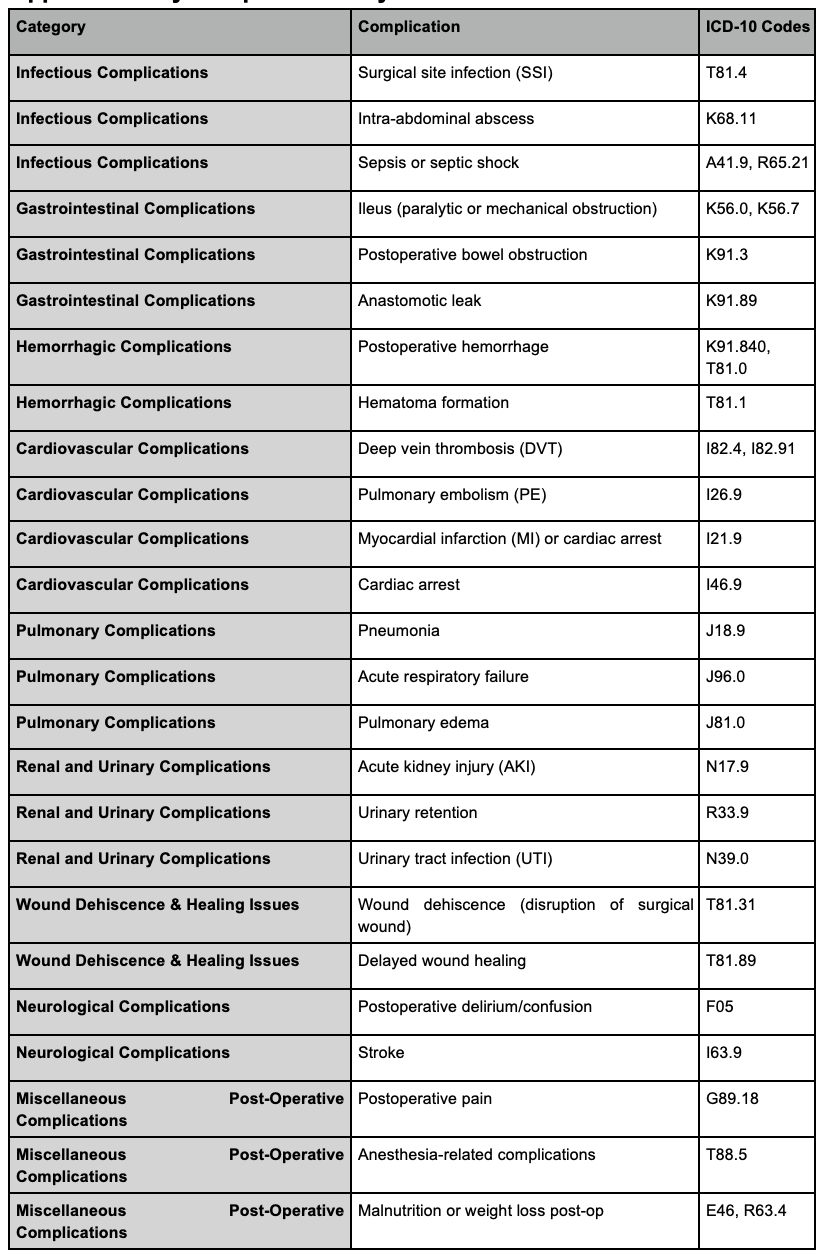
Figure: Table 1: Appendectomy complications by UC status ICD-10 codes
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Meghana Kakarla indicated no relevant financial relationships.
Patricia Ziegler indicated no relevant financial relationships.
Joseph Frasca indicated no relevant financial relationships.
Maham Lodhi indicated no relevant financial relationships.
Veena Nannegari indicated no relevant financial relationships.
Atsushi Sakuraba indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Meghana Kakarla, MD2, Patricia Ziegler, MD1, Joseph Frasca, MD1, Maham Lodhi, MD1, Veena Nannegari, MD3, Atsushi Sakuraba, MD, PhD1. P5399 - Postoperative Complications After Appendectomy in Ulcerative Colitis: A National Inpatient Cohort Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
