Tuesday Poster Session
Category: IBD
P5392 - Natural History of Crohn’s Disease and Ulcerative Colitis in Newly Diagnosed Hispanic Adults in the United States: A Population-Based Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SS
Siddharth Singh, MD, MS
University of California San Diego
San Diego, CA
Presenting Author(s)
Dhruv Ahuja, MBBS1, Yuchen Qi, MS2, Sagar Patel, BS2, Vipul Jairath, MBChB, DPhil, MRCP3, Ronghui Xu, PhD2, James Lewis, MD, MSCE4, Michael D. Kappelman, MD5, Shane Goodwin, PhD6, Siddharth Singh, MD, MS2
1University of California San Diego, Delhi, Delhi, India; 2University of California San Diego, San Diego, CA; 3Department of Medicine and Department of Epidemiology and Biostatistics, Western University, London, ON, Canada; 4University of Penn, Philadelphia, PA; 5University of North Carolina, Chapel Hill, NC; 6Western University, London, ON, Canada
Introduction: We conducted a retrospective cohort study examining the natural history of inflammatory bowel diseases (IBD) in Hispanics, compared with Whites in the United States.
Methods: Using an administrative claims database (OptumLabs® Data Warehouse), we created an inception cohort of adults newly diagnosed with IBD diagnosed with IBD (91% positive predictive value) between 2007-23. We examined and compared cumulative risk of hospitalization, IBD-related surgery and treatment patterns in patients with Crohn’s disease (CD) and ulcerative colitis (UC) between Hispanics and Whites, and examined the interaction between race/ethnicity and education and income as surrogate measures of social risk.
Results: We included 520 Hispanic adults with incident IBD (211 with CD, 309 with UC) compared with 5484 Whites with incident IBD (2447 with CD, 3037 with UC). Among patients with CD, the cumulative 5-y risk of all-cause hospitalization and surgery was 17.7% and 11.5%, respectively, and was similar to the risk observed in Whites (Table 1). While there were no differences in risk of corticosteroid use (Hispanics vs. Whites, 5y risk: 70.0% vs. 69.4%, p=0.59), utilization of immunomodulators (24.2% vs. 33.1%, p=0.047) and advanced therapies (35.8% vs. 48.1%, p=0.001) was lower in Hispanic patients.
Among patients with UC, the cumulative 5-y risk of all-cause hospitalization was lower in Hispanics (10.5% vs. 17.6%, p=0.034), without differences in risk of surgery (3.8% vs. 6.3%, p=0.22) (Table 2). While the risk of corticosteroid use was lower in Hispanics vs. Whites (5y risk: 60.6% vs. 72.7%, p=0.002), no differences were observed in the use of immunomodulator (15.4% vs. 19.8%, p=0.057) or advanced therapies (29.2% vs. 29.2%, p=0.63).
Higher education level, but not income, was associated with lower risk of corticosteroid use and higher risk of advanced therapy use. There was no significant interaction between race, education or income and IBD outcomes.
Discussion: In an inception cohort of newly diagnosed patients with IBD, the natural history of CD was similar between Hispanics vs. Whites, though utilization of advanced therapies and immunomodulators was lower. In contrast, Hispanic adults with UC had lower risk of hospitalization and need for corticosteroids compared with Whites, but without significant differences in utilization of advanced therapies. Education and income level did not explain differences observed between Hispanics vs. Whites.
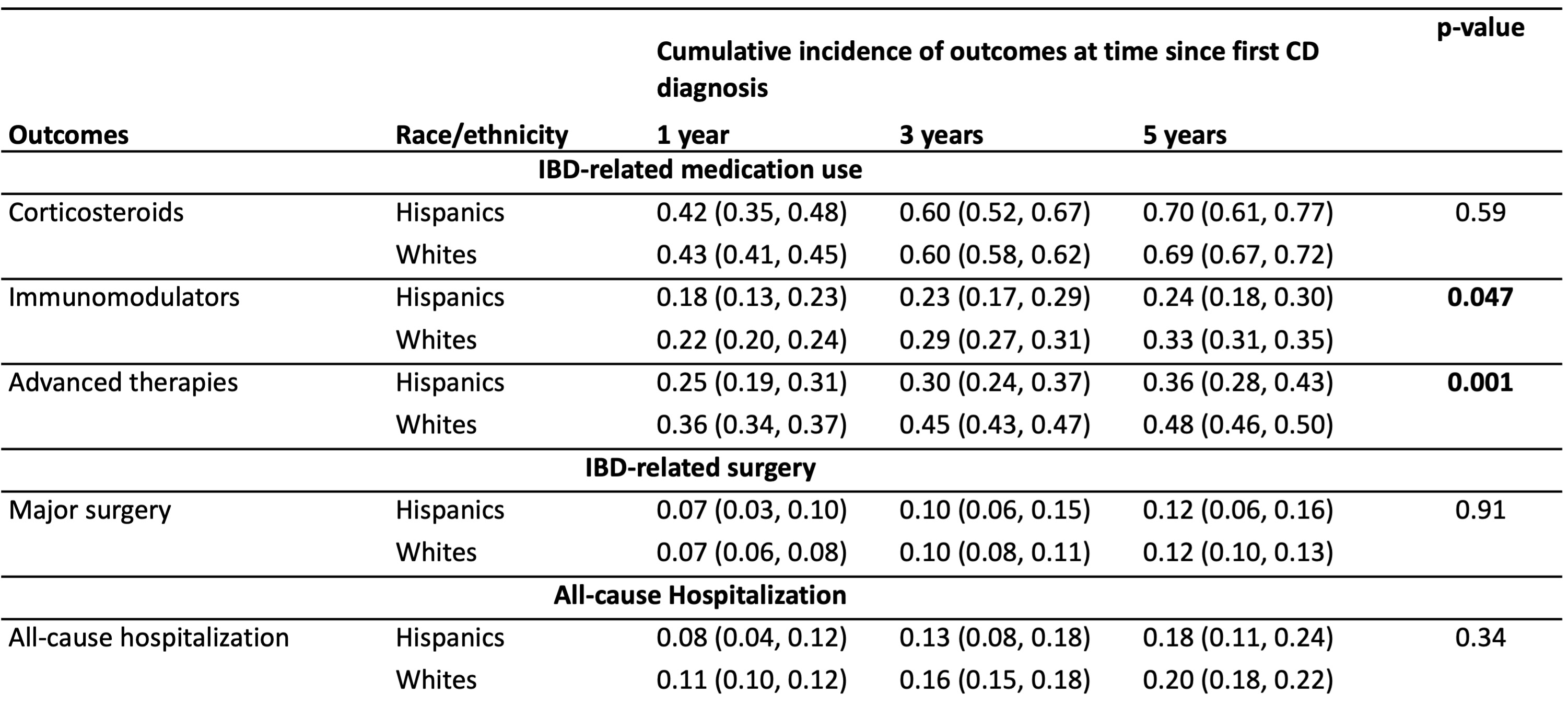
Figure: Cumulative incidence for outcomes calculated 1, 3 and 5 years after first diagnosis of Crohn’s disease in Hispanics vs. Whites
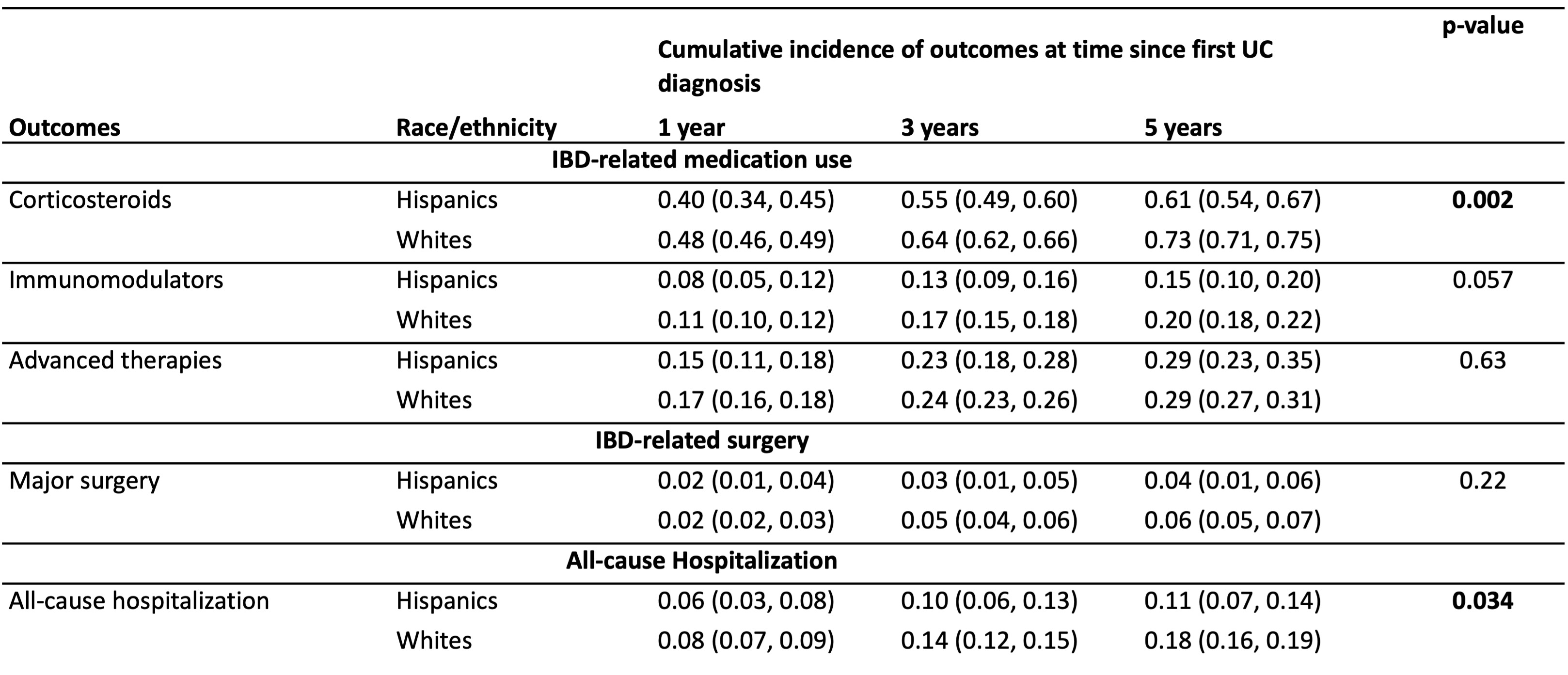
Figure: Cumulative incidence for outcomes calculated 1, 3 and 5 years after first diagnosis of ulcerative colitis in Hispanics vs. Whites
Disclosures:
Dhruv Ahuja indicated no relevant financial relationships.
Yuchen Qi indicated no relevant financial relationships.
Sagar Patel indicated no relevant financial relationships.
Vipul Jairath: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. Alimentiv – Consultant, Grant/Research Support. Arena Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Asahi Kasei Pharma – Consultant, Grant/Research Support, Speakers Bureau. Asieris Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. AstraZeneca – Consultant, Grant/Research Support, Speakers Bureau. Avoro Capital – Consultant. Bristol Myers Squibb – Consultant, Grant/Research Support, Speakers Bureau. Celltrion – Consultant, Grant/Research Support, Speakers Bureau. Eli Lilly and Company – Consultant, Grant/Research Support, Speakers Bureau. Endpoint Health – Consultant. Enthera – Consultant. Ferring Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Flagship Pioneering – Consultant, Grant/Research Support, Speakers Bureau. Fresenius Kabi – Consultant, Grant/Research Support, Speakers Bureau. Galapagos NV – Consultant, Grant/Research Support, Speakers Bureau. Genentech – Consultant, Grant/Research Support, Speakers Bureau. Gilde Healthcare – Consultant. Gilead Sciences – Consultant, Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Consultant, Grant/Research Support, Speakers Bureau. Innomar – Consultant. JAMP – Consultant. Johnson & Johnson – Advisor or Review Panel Member, Speakers Bureau. Merck – Consultant, Grant/Research Support, Speakers Bureau. Metacrine – Consultant, Grant/Research Support, Speakers Bureau. Mylan – Consultant, Grant/Research Support, Speakers Bureau. Pandion Therapeutics – Consultant, Grant/Research Support, Speakers Bureau. Pendopharm – Consultant, Grant/Research Support, Speakers Bureau. Pfizer – Consultant, Grant/Research Support, Speakers Bureau. Prometheus Therapeutics and Diagnostics – Consultant, Grant/Research Support, Speakers Bureau. Protagonist Therapeutics – Consultant, Grant/Research Support, Speakers Bureau. Reistone Biopharma – Consultant, Grant/Research Support, Speakers Bureau. Roche – Consultant, Grant/Research Support, Speakers Bureau. Roivant – Consultant. Sandoz – Consultant, Grant/Research Support, Speakers Bureau. Second Genome – Consultant, Grant/Research Support, Speakers Bureau. Shire – Speakers Bureau. Sorriso Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Syndegen – Consultant. Takeda – Consultant, Intellectual Property/Patents, Speakers Bureau. TD Securities – Consultant. Teva – Consultant, Grant/Research Support, Speakers Bureau. Topivert – Consultant, Grant/Research Support, Speakers Bureau. Ventyx Biosciences – Consultant, Grant/Research Support, Speakers Bureau. Vividion Therapeutics – Consultant, Grant/Research Support, Speakers Bureau.
Ronghui Xu indicated no relevant financial relationships.
James Lewis: 3M – Expert witness. AbbVie – Grant/Research Support. Amgen – Advisor or Review Panel Member. Dark Canyon Laboratories – Owner/Ownership Interest. Eli Lilly – Consultant, Grant/Research Support. Johnson & Johnson – Advisory Committee/Board Member, Grant/Research Support. Odyssey Therapeutics – Advisor or Review Panel Member. Pfizer – Advisor or Review Panel Member. Sanofi – Advisor or Review Panel Member. Spyre Therapeutics – Advisor or Review Panel Member.
Michael Kappelman: Eli Lilly – Consultant. Takeda – Consultant.
Shane Goodwin indicated no relevant financial relationships.
Siddharth Singh indicated no relevant financial relationships.
Dhruv Ahuja, MBBS1, Yuchen Qi, MS2, Sagar Patel, BS2, Vipul Jairath, MBChB, DPhil, MRCP3, Ronghui Xu, PhD2, James Lewis, MD, MSCE4, Michael D. Kappelman, MD5, Shane Goodwin, PhD6, Siddharth Singh, MD, MS2. P5392 - Natural History of Crohn’s Disease and Ulcerative Colitis in Newly Diagnosed Hispanic Adults in the United States: A Population-Based Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California San Diego, Delhi, Delhi, India; 2University of California San Diego, San Diego, CA; 3Department of Medicine and Department of Epidemiology and Biostatistics, Western University, London, ON, Canada; 4University of Penn, Philadelphia, PA; 5University of North Carolina, Chapel Hill, NC; 6Western University, London, ON, Canada
Introduction: We conducted a retrospective cohort study examining the natural history of inflammatory bowel diseases (IBD) in Hispanics, compared with Whites in the United States.
Methods: Using an administrative claims database (OptumLabs® Data Warehouse), we created an inception cohort of adults newly diagnosed with IBD diagnosed with IBD (91% positive predictive value) between 2007-23. We examined and compared cumulative risk of hospitalization, IBD-related surgery and treatment patterns in patients with Crohn’s disease (CD) and ulcerative colitis (UC) between Hispanics and Whites, and examined the interaction between race/ethnicity and education and income as surrogate measures of social risk.
Results: We included 520 Hispanic adults with incident IBD (211 with CD, 309 with UC) compared with 5484 Whites with incident IBD (2447 with CD, 3037 with UC). Among patients with CD, the cumulative 5-y risk of all-cause hospitalization and surgery was 17.7% and 11.5%, respectively, and was similar to the risk observed in Whites (Table 1). While there were no differences in risk of corticosteroid use (Hispanics vs. Whites, 5y risk: 70.0% vs. 69.4%, p=0.59), utilization of immunomodulators (24.2% vs. 33.1%, p=0.047) and advanced therapies (35.8% vs. 48.1%, p=0.001) was lower in Hispanic patients.
Among patients with UC, the cumulative 5-y risk of all-cause hospitalization was lower in Hispanics (10.5% vs. 17.6%, p=0.034), without differences in risk of surgery (3.8% vs. 6.3%, p=0.22) (Table 2). While the risk of corticosteroid use was lower in Hispanics vs. Whites (5y risk: 60.6% vs. 72.7%, p=0.002), no differences were observed in the use of immunomodulator (15.4% vs. 19.8%, p=0.057) or advanced therapies (29.2% vs. 29.2%, p=0.63).
Higher education level, but not income, was associated with lower risk of corticosteroid use and higher risk of advanced therapy use. There was no significant interaction between race, education or income and IBD outcomes.
Discussion: In an inception cohort of newly diagnosed patients with IBD, the natural history of CD was similar between Hispanics vs. Whites, though utilization of advanced therapies and immunomodulators was lower. In contrast, Hispanic adults with UC had lower risk of hospitalization and need for corticosteroids compared with Whites, but without significant differences in utilization of advanced therapies. Education and income level did not explain differences observed between Hispanics vs. Whites.
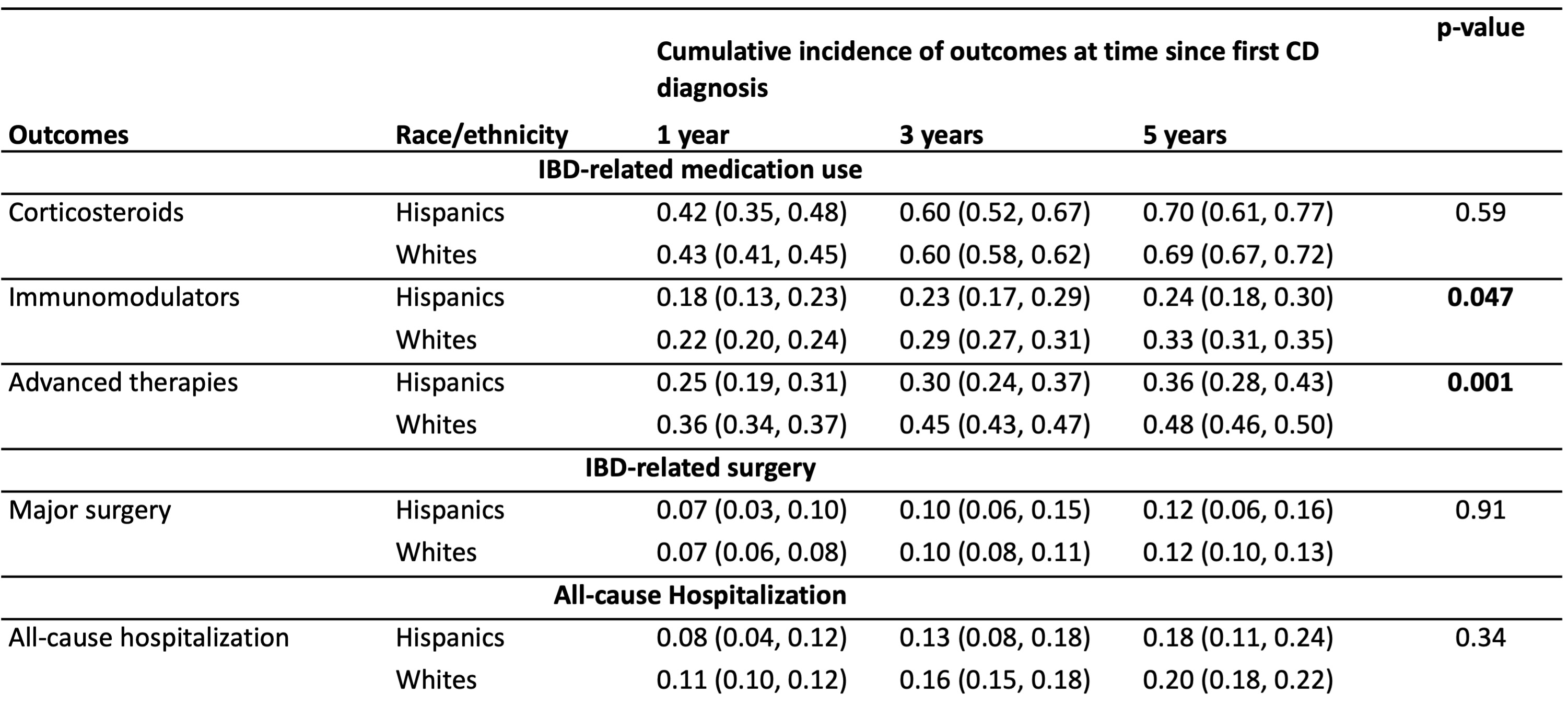
Figure: Cumulative incidence for outcomes calculated 1, 3 and 5 years after first diagnosis of Crohn’s disease in Hispanics vs. Whites
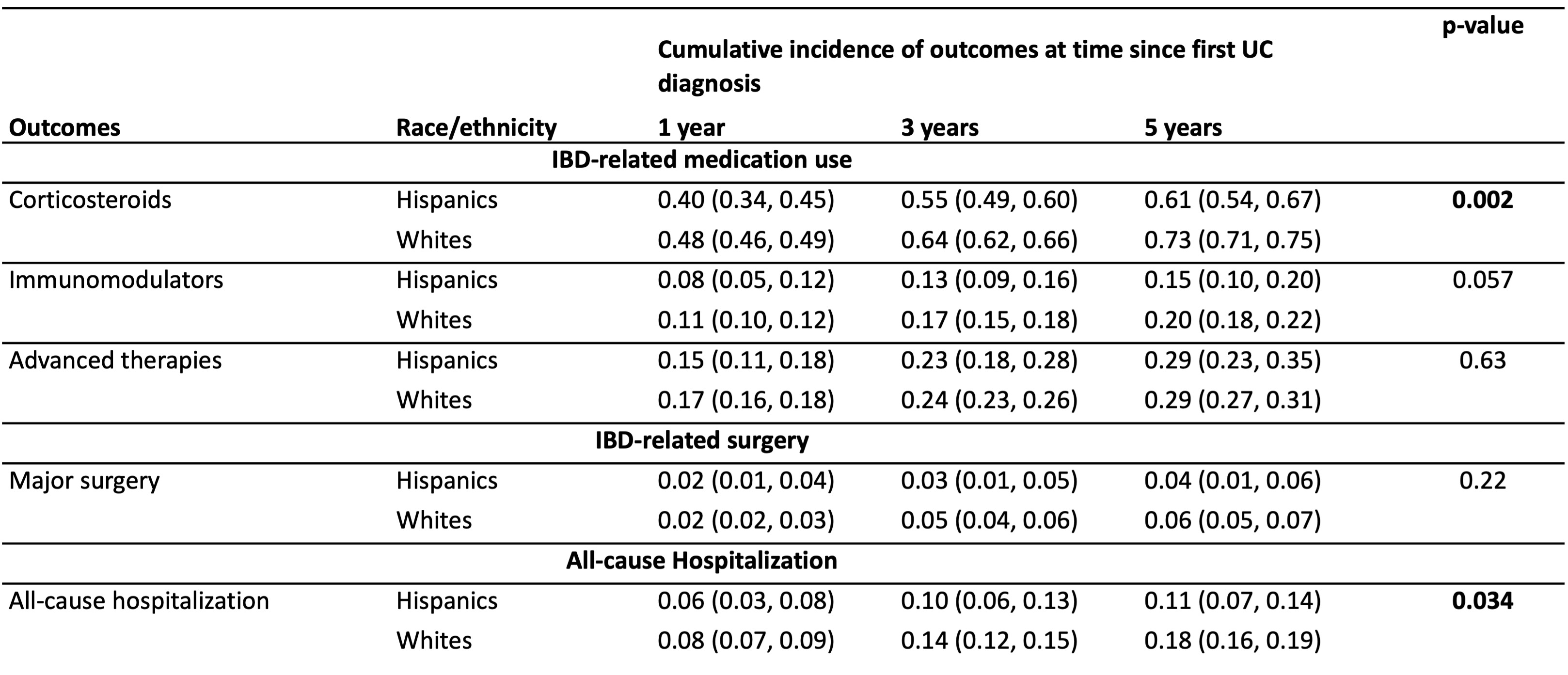
Figure: Cumulative incidence for outcomes calculated 1, 3 and 5 years after first diagnosis of ulcerative colitis in Hispanics vs. Whites
Disclosures:
Dhruv Ahuja indicated no relevant financial relationships.
Yuchen Qi indicated no relevant financial relationships.
Sagar Patel indicated no relevant financial relationships.
Vipul Jairath: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. Alimentiv – Consultant, Grant/Research Support. Arena Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Asahi Kasei Pharma – Consultant, Grant/Research Support, Speakers Bureau. Asieris Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. AstraZeneca – Consultant, Grant/Research Support, Speakers Bureau. Avoro Capital – Consultant. Bristol Myers Squibb – Consultant, Grant/Research Support, Speakers Bureau. Celltrion – Consultant, Grant/Research Support, Speakers Bureau. Eli Lilly and Company – Consultant, Grant/Research Support, Speakers Bureau. Endpoint Health – Consultant. Enthera – Consultant. Ferring Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Flagship Pioneering – Consultant, Grant/Research Support, Speakers Bureau. Fresenius Kabi – Consultant, Grant/Research Support, Speakers Bureau. Galapagos NV – Consultant, Grant/Research Support, Speakers Bureau. Genentech – Consultant, Grant/Research Support, Speakers Bureau. Gilde Healthcare – Consultant. Gilead Sciences – Consultant, Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Consultant, Grant/Research Support, Speakers Bureau. Innomar – Consultant. JAMP – Consultant. Johnson & Johnson – Advisor or Review Panel Member, Speakers Bureau. Merck – Consultant, Grant/Research Support, Speakers Bureau. Metacrine – Consultant, Grant/Research Support, Speakers Bureau. Mylan – Consultant, Grant/Research Support, Speakers Bureau. Pandion Therapeutics – Consultant, Grant/Research Support, Speakers Bureau. Pendopharm – Consultant, Grant/Research Support, Speakers Bureau. Pfizer – Consultant, Grant/Research Support, Speakers Bureau. Prometheus Therapeutics and Diagnostics – Consultant, Grant/Research Support, Speakers Bureau. Protagonist Therapeutics – Consultant, Grant/Research Support, Speakers Bureau. Reistone Biopharma – Consultant, Grant/Research Support, Speakers Bureau. Roche – Consultant, Grant/Research Support, Speakers Bureau. Roivant – Consultant. Sandoz – Consultant, Grant/Research Support, Speakers Bureau. Second Genome – Consultant, Grant/Research Support, Speakers Bureau. Shire – Speakers Bureau. Sorriso Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Syndegen – Consultant. Takeda – Consultant, Intellectual Property/Patents, Speakers Bureau. TD Securities – Consultant. Teva – Consultant, Grant/Research Support, Speakers Bureau. Topivert – Consultant, Grant/Research Support, Speakers Bureau. Ventyx Biosciences – Consultant, Grant/Research Support, Speakers Bureau. Vividion Therapeutics – Consultant, Grant/Research Support, Speakers Bureau.
Ronghui Xu indicated no relevant financial relationships.
James Lewis: 3M – Expert witness. AbbVie – Grant/Research Support. Amgen – Advisor or Review Panel Member. Dark Canyon Laboratories – Owner/Ownership Interest. Eli Lilly – Consultant, Grant/Research Support. Johnson & Johnson – Advisory Committee/Board Member, Grant/Research Support. Odyssey Therapeutics – Advisor or Review Panel Member. Pfizer – Advisor or Review Panel Member. Sanofi – Advisor or Review Panel Member. Spyre Therapeutics – Advisor or Review Panel Member.
Michael Kappelman: Eli Lilly – Consultant. Takeda – Consultant.
Shane Goodwin indicated no relevant financial relationships.
Siddharth Singh indicated no relevant financial relationships.
Dhruv Ahuja, MBBS1, Yuchen Qi, MS2, Sagar Patel, BS2, Vipul Jairath, MBChB, DPhil, MRCP3, Ronghui Xu, PhD2, James Lewis, MD, MSCE4, Michael D. Kappelman, MD5, Shane Goodwin, PhD6, Siddharth Singh, MD, MS2. P5392 - Natural History of Crohn’s Disease and Ulcerative Colitis in Newly Diagnosed Hispanic Adults in the United States: A Population-Based Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
