Tuesday Poster Session
Category: IBD
P5385 - Malnutrition in Acute Severe Ulcerative Colitis: Prevalence, Nutritional Interventions, and Clinical Outcomes - A Single-Center Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SS
Shreyak Sharma, MD
Yale University School of Medicine
New Haven, CT
Presenting Author(s)
Shreyak Sharma, MD1, Eleazar E.. Montalvan-Sanchez, MD1, Dalton A. Norwood, MD2, Alexander N.. Levy, MD1
1Yale University School of Medicine, New Haven, CT; 2University of Alabama at Birmingham, Birmingham, AL
Introduction: Ulcerative colitis patients are frequently malnourished. It predisposes them to poorer clinical outcomes. We aim to study the prevalence of malnutrition in hospitalized patients with acute severe ulcerative colitis (ASUC), clinical outcomes, and nutrition specific interventions during their hospital stay.
Methods: We conducted a retrospective study of patients hospitalized with acute severe ulcerative colitis (ASUC) at a single center between 1/1/15-8/30/23. Malnutrition was defined as >5% total body weight loss in 6 months. Outcomes included prolonged hospitalization (≥10 days), use of TPN, infliximab (IFX) rescue, and colectomy. Associations between malnutrition and outcomes were assessed using logistic regression adjusted for age, sex, and race. Summary statistics and group comparisons were conducted using appropriate parametric and nonparametric tests. All analyses were performed using Stata18.
Results: Among 216 patients hospitalized with ASUC, 30.1% (n=65) met criteria for malnutrition. Patients with malnutrition had a lower mean BMI (24.7 vs. 27.0, p=0.022), higher rates of underweight status (BMI < 18.5: 15.6% vs. 6.9%, p=0.048), and lower median albumin (3.3 vs. 3.6 g/dL, p=0.008) compared to non-malnourished patients. Baseline fecal calprotectin levels were also significantly higher in malnourished patients (3895 vs. 2492 µg/g, p=0.008). Nutrition consults were more frequently placed among malnourished patients (63.1% vs. 34.5%, p< 0.001), though only 6.2% received TPN. In adjusted logistic regression, malnutrition was independently associated with increased odds of IFX rescue (OR 2.15, 95% CI 1.16–4.02, p=0.016), but not with prolonged hospitalization (≥10 days), TPN use, or colectomy. An interaction model revealed that low albumin was associated with increased odds of prolonged hospitalization (OR 3.51, 95% CI 1.38–8.91, p=0.008), but malnutrition alone was not significant. The interaction between malnutrition and albumin was not statistically significant (OR 1.86, p=0.512), suggesting independent rather than synergistic effects on length of stay.
Discussion: Approximately 30% patients in a cohort of patients with ASUC were malnourished, which in turn led to greater odds of requiring salvage therapy with infliximab. Longitudinal optimization of nutritional status may lead to improved treatment success in UC.
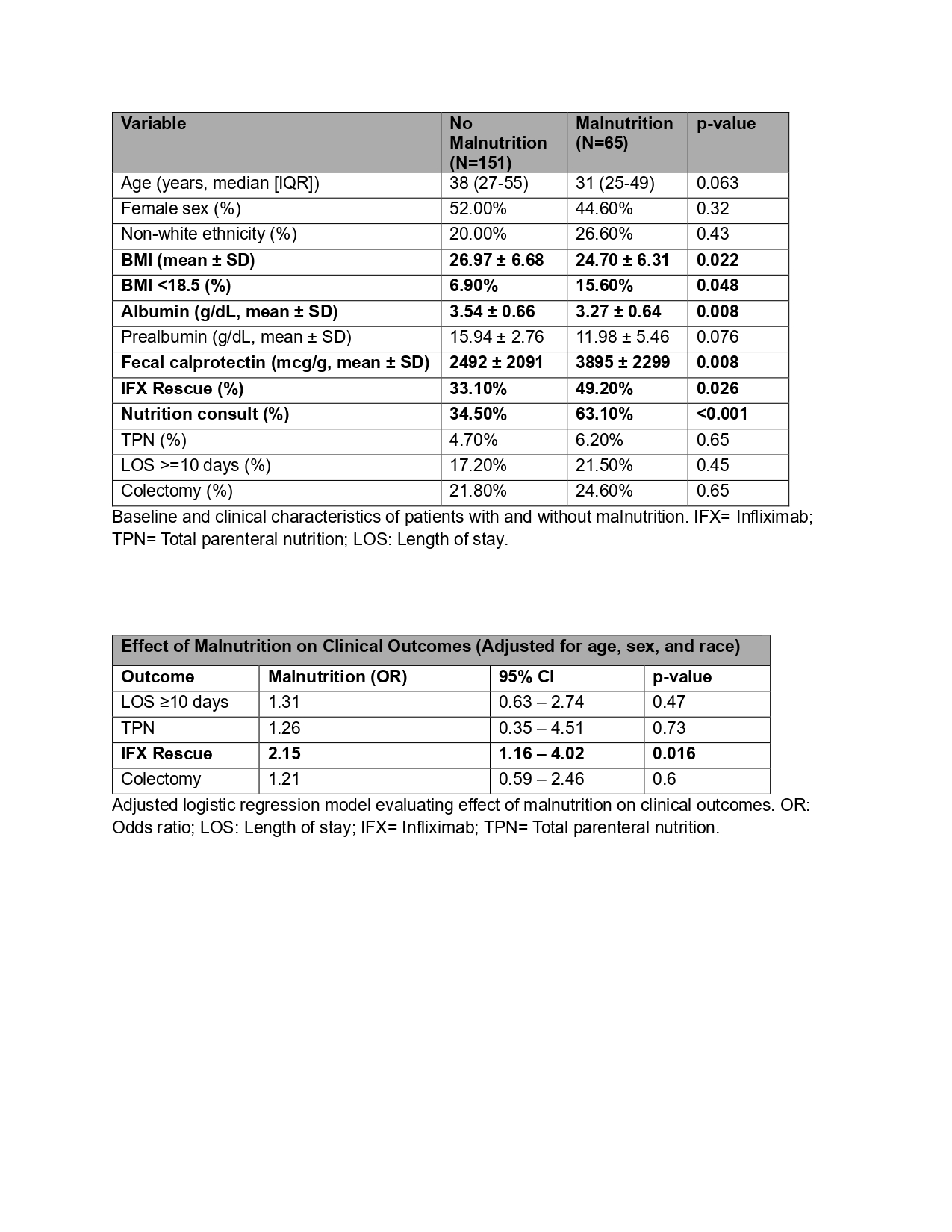
Figure: Table 1. Baseline and clinical characteristics of patients with and without malnutrition.
Table 2. Adjusted logistic regression model evaluating effect of malnutrition on clinical outcomes
Disclosures:
Shreyak Sharma indicated no relevant financial relationships.
Eleazar Montalvan-Sanchez indicated no relevant financial relationships.
Dalton Norwood indicated no relevant financial relationships.
Alexander Levy: BMS – Consultant. Johnson & Johnson – Consultant.
Shreyak Sharma, MD1, Eleazar E.. Montalvan-Sanchez, MD1, Dalton A. Norwood, MD2, Alexander N.. Levy, MD1. P5385 - Malnutrition in Acute Severe Ulcerative Colitis: Prevalence, Nutritional Interventions, and Clinical Outcomes - A Single-Center Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Yale University School of Medicine, New Haven, CT; 2University of Alabama at Birmingham, Birmingham, AL
Introduction: Ulcerative colitis patients are frequently malnourished. It predisposes them to poorer clinical outcomes. We aim to study the prevalence of malnutrition in hospitalized patients with acute severe ulcerative colitis (ASUC), clinical outcomes, and nutrition specific interventions during their hospital stay.
Methods: We conducted a retrospective study of patients hospitalized with acute severe ulcerative colitis (ASUC) at a single center between 1/1/15-8/30/23. Malnutrition was defined as >5% total body weight loss in 6 months. Outcomes included prolonged hospitalization (≥10 days), use of TPN, infliximab (IFX) rescue, and colectomy. Associations between malnutrition and outcomes were assessed using logistic regression adjusted for age, sex, and race. Summary statistics and group comparisons were conducted using appropriate parametric and nonparametric tests. All analyses were performed using Stata18.
Results: Among 216 patients hospitalized with ASUC, 30.1% (n=65) met criteria for malnutrition. Patients with malnutrition had a lower mean BMI (24.7 vs. 27.0, p=0.022), higher rates of underweight status (BMI < 18.5: 15.6% vs. 6.9%, p=0.048), and lower median albumin (3.3 vs. 3.6 g/dL, p=0.008) compared to non-malnourished patients. Baseline fecal calprotectin levels were also significantly higher in malnourished patients (3895 vs. 2492 µg/g, p=0.008). Nutrition consults were more frequently placed among malnourished patients (63.1% vs. 34.5%, p< 0.001), though only 6.2% received TPN. In adjusted logistic regression, malnutrition was independently associated with increased odds of IFX rescue (OR 2.15, 95% CI 1.16–4.02, p=0.016), but not with prolonged hospitalization (≥10 days), TPN use, or colectomy. An interaction model revealed that low albumin was associated with increased odds of prolonged hospitalization (OR 3.51, 95% CI 1.38–8.91, p=0.008), but malnutrition alone was not significant. The interaction between malnutrition and albumin was not statistically significant (OR 1.86, p=0.512), suggesting independent rather than synergistic effects on length of stay.
Discussion: Approximately 30% patients in a cohort of patients with ASUC were malnourished, which in turn led to greater odds of requiring salvage therapy with infliximab. Longitudinal optimization of nutritional status may lead to improved treatment success in UC.
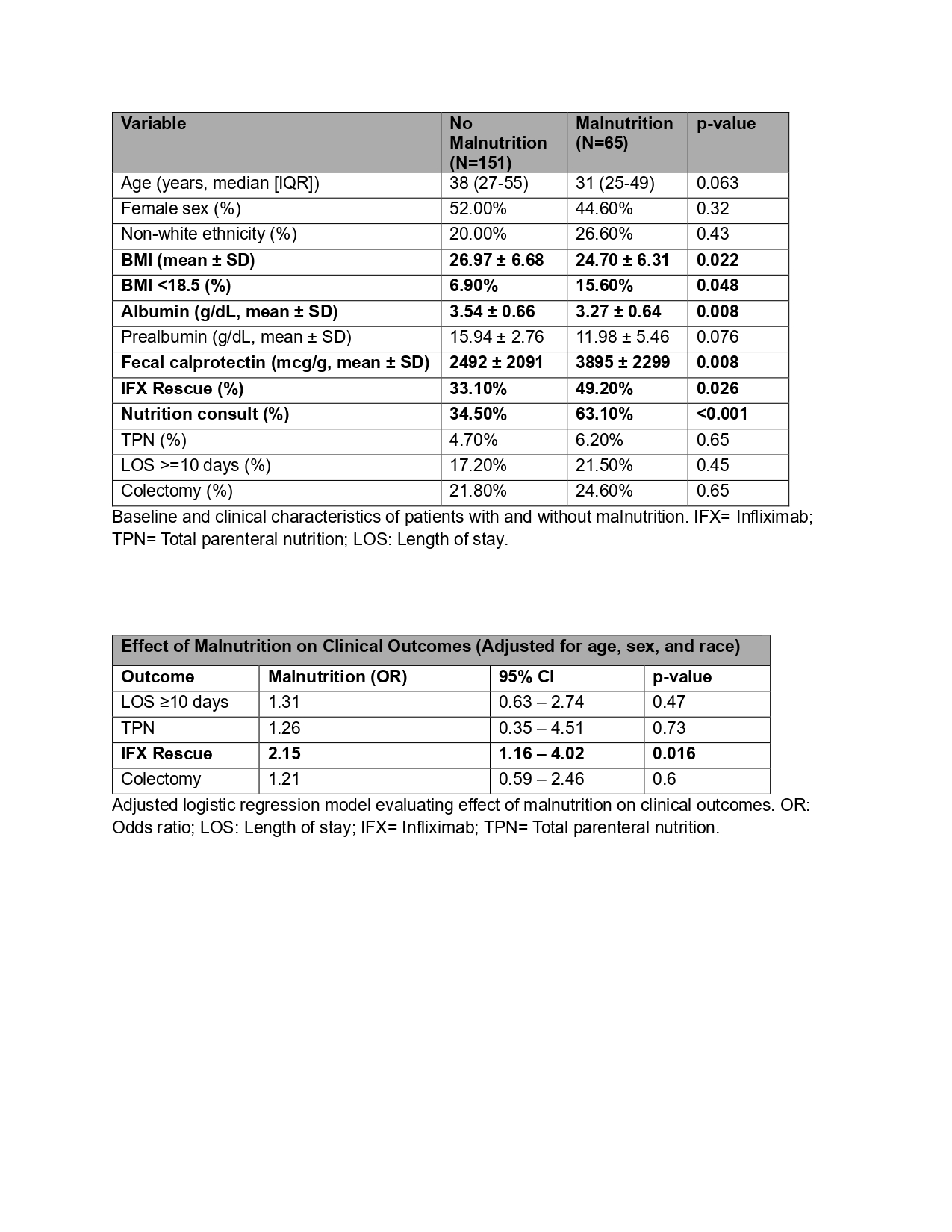
Figure: Table 1. Baseline and clinical characteristics of patients with and without malnutrition.
Table 2. Adjusted logistic regression model evaluating effect of malnutrition on clinical outcomes
Disclosures:
Shreyak Sharma indicated no relevant financial relationships.
Eleazar Montalvan-Sanchez indicated no relevant financial relationships.
Dalton Norwood indicated no relevant financial relationships.
Alexander Levy: BMS – Consultant. Johnson & Johnson – Consultant.
Shreyak Sharma, MD1, Eleazar E.. Montalvan-Sanchez, MD1, Dalton A. Norwood, MD2, Alexander N.. Levy, MD1. P5385 - Malnutrition in Acute Severe Ulcerative Colitis: Prevalence, Nutritional Interventions, and Clinical Outcomes - A Single-Center Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
