Tuesday Poster Session
Category: IBD
P5375 - National Burden of Anxiety/Depression Symptoms and Counseling/Therapy Utilization Among Adults With Inflammatory Bowel Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ruby Greywoode, MD, MS
Assistant Professor of Medicine
Montefiore Medical Center, Albert Einstein College of Medicine
New York, NY
Presenting Author(s)
Ruby Greywoode, MD, MS1, David W. Lounsbury, PhD2, Thomas Ullman, MD3, Laurie Keefer, PhD, FACG4
1Montefiore Medical Center, Albert Einstein College of Medicine, New York, NY; 2Albert Einstein College of Medicine, New York, NY; 3Icahn School of Medicine at Mount Sinai, Scarsdale, NY; 4Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Given bidirectionality between anxiety/depression and inflammatory bowel disease (IBD) activity, screening for symptoms of anxiety and depression is a recommended part of IBD management. Estimates for the burden of anxiety/depression vary, and there is little data on mental healthcare utilization patterns. We sought to examine the national prevalence of adults with IBD who screen positive for anxiety/depression as well as their patterns of mental health care utilization.
Methods: Adults ≥18 years in the cross-sectional 2023 National Health Interview Survey (NHIS) were screened via the Patient Health Questionnaire depression scale (PHQ2) and Generalized Anxiety Disorder scale (GAD2) with a positive screen cutoff of 3 for both. We analyzed the weighted prevalence of symptoms of anxiety, depression, and mental healthcare utilization for individuals with and without IBD using descriptive statistics. We compared prevalence and utilization estimates using logistic regression, adjusted for age, sex, race, ethnicity, and health insurance status.
Results: Of adults sampled in the 2023 NHIS (n = 29522), 572 reported a history of IBD (UC:n = 390; CD:n = 135; UC/CD:n=44), corresponding to approximately 4.2 million adults with IBD in the United States. (Table 1) There was a significantly higher prevalence of positive screening for anxiety/depression in those with IBD compared to those without IBD (14.3% v. 9.5% and 10.9% v. 6.9%, respectively;P < .001). The odds of screening positive for anxiety and depression was twice that for those with compared to those without IBD (anxiety: OR 2.0,95%CI 1.5-2.8; depression: OR 2.0, 95%CI 1.5-2.7). Approximately a quarter of individuals with IBD received counseling/therapy over the preceding 12 months, twice the odds of those without IBD (OR 2.0,95%CI 1.6-2.6). Among those with IBD who screened positive for anxiety/depression, 40-53% received counseling/therapy from a mental health professional, while 20-29% either did not receive or delayed counseling/therapy due to cost. (Figure 1)
Discussion: Among a nationally representative population of adults with IBD, approximately 1 in 7 screen positive for anxiety and 1 in 10 screen positive for depression, which is twice the odds of adults without IBD. Among those with IBD who screen positive for anxiety/depression up to a quarter forgo or delay counseling/therapy due to cost. Innovations to address cost related barriers to counseling and therapy for patients with IBD and symptoms of anxiety or depression are needed.
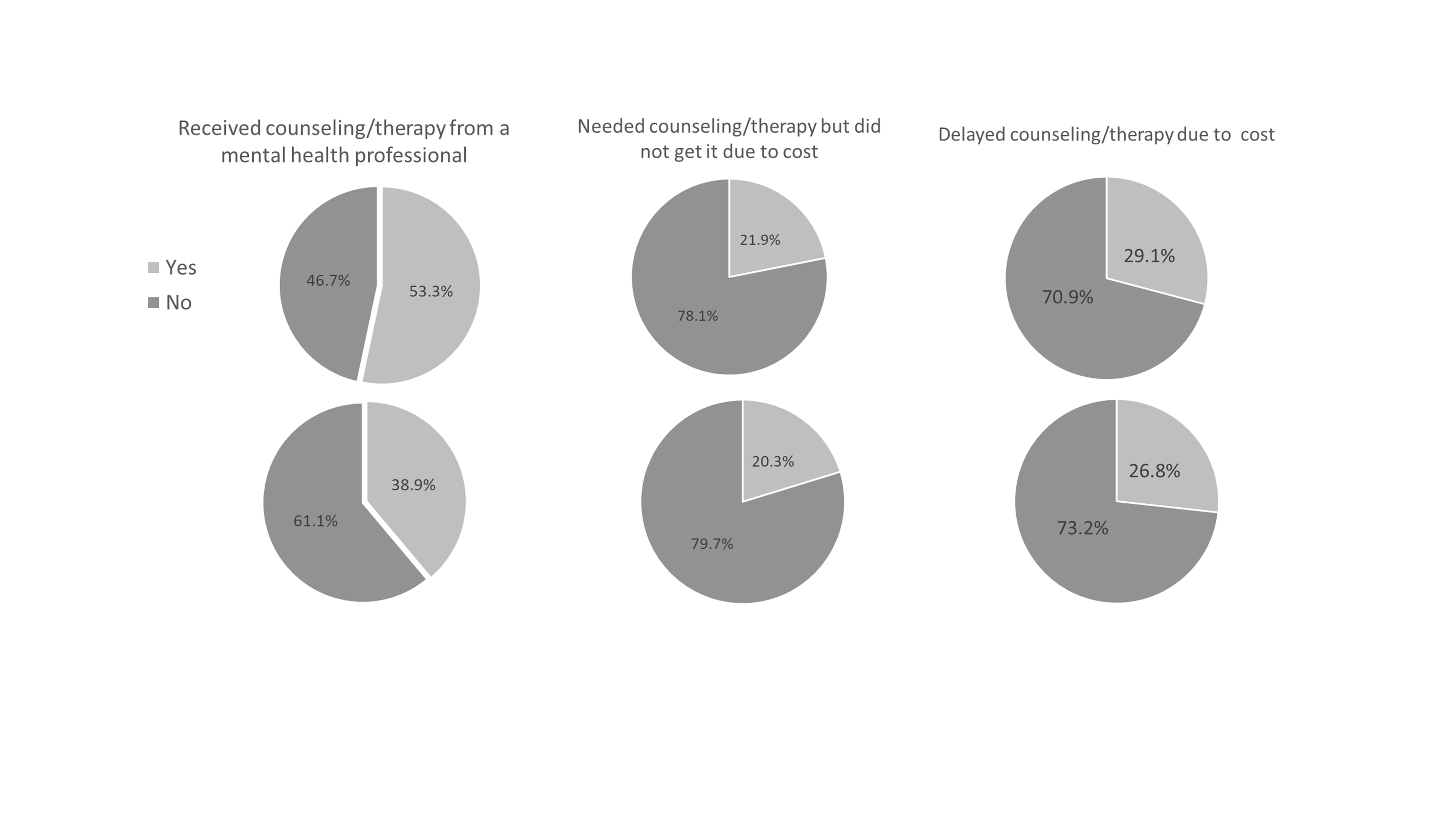
Figure: Figure 1. Counseling and therapy use and affordability among adults with IBD who screen positive for anxiety or depression. In a nationally representative population of US adults with IBD who screen positive for anxiety (top panel) or depression (bottom panel), approximately 40-53% received counseling/therapy over the preceding 12 months, while 20-29% either did not receive or delayed counseling/therapy due to cost.
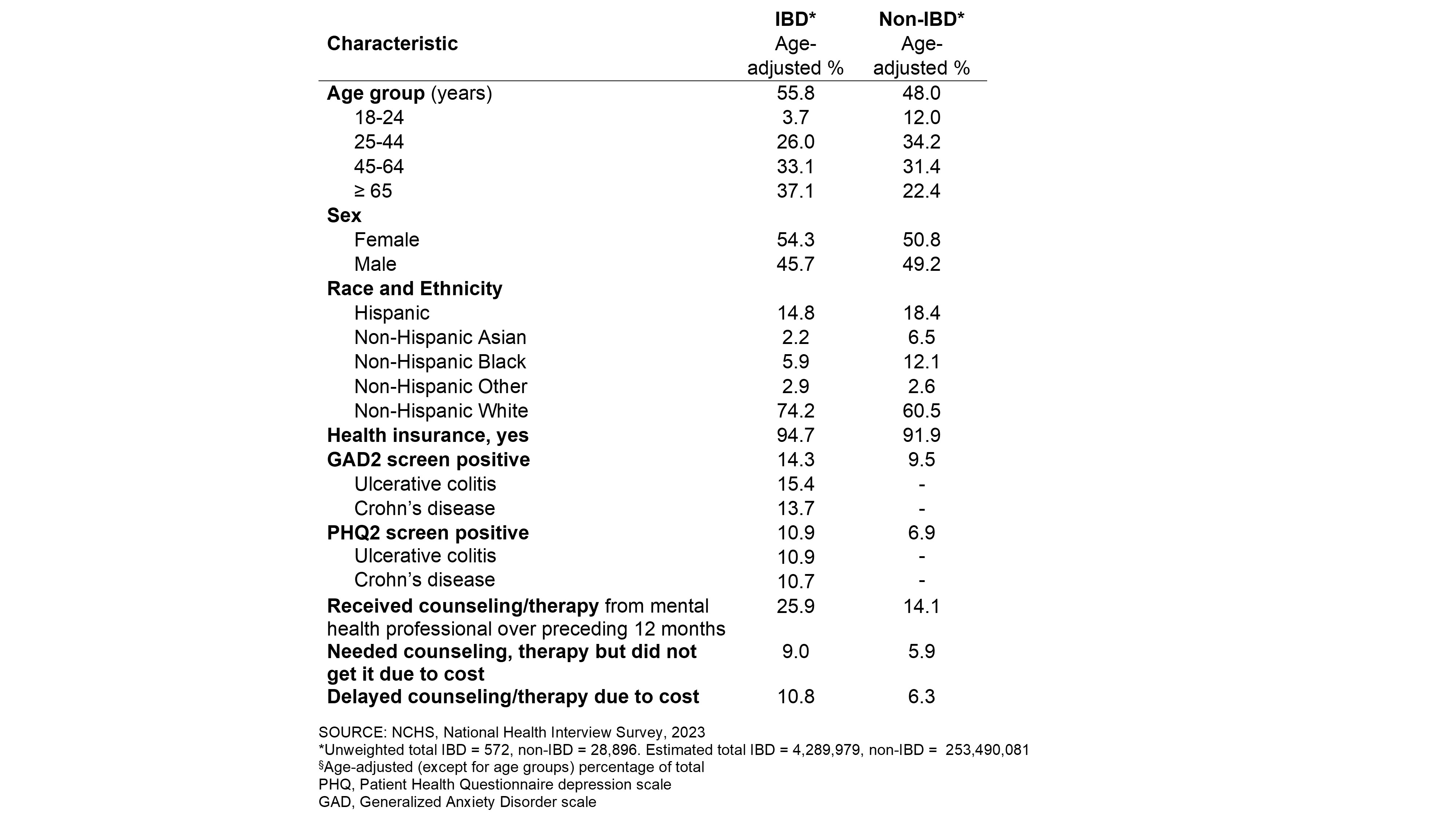
Figure: Table 1. Characteristics of US Adults by Inflammatory Bowel Disease (IBD) Diagnosis
Disclosures:
Ruby Greywoode: Janssen Scientific Affairs – Grant/Research Support. Sanofi – Consultant.
David Lounsbury indicated no relevant financial relationships.
Thomas Ullman: Bristol Myers Squibb – Consultant. J&J – Consultant. Pfizer – Consultant.
Laurie Keefer: AbbVie – Consultant. Ardelyx – Consultant. Eli Lilly – Consultant. Janssen – Consultant. Pfizer – Consultant. Reckitt Health – Consultant. Trellus Health – Owner/Ownership Interest, Stock-publicly held company(excluding mutual/index funds).
Ruby Greywoode, MD, MS1, David W. Lounsbury, PhD2, Thomas Ullman, MD3, Laurie Keefer, PhD, FACG4. P5375 - National Burden of Anxiety/Depression Symptoms and Counseling/Therapy Utilization Among Adults With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Montefiore Medical Center, Albert Einstein College of Medicine, New York, NY; 2Albert Einstein College of Medicine, New York, NY; 3Icahn School of Medicine at Mount Sinai, Scarsdale, NY; 4Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Given bidirectionality between anxiety/depression and inflammatory bowel disease (IBD) activity, screening for symptoms of anxiety and depression is a recommended part of IBD management. Estimates for the burden of anxiety/depression vary, and there is little data on mental healthcare utilization patterns. We sought to examine the national prevalence of adults with IBD who screen positive for anxiety/depression as well as their patterns of mental health care utilization.
Methods: Adults ≥18 years in the cross-sectional 2023 National Health Interview Survey (NHIS) were screened via the Patient Health Questionnaire depression scale (PHQ2) and Generalized Anxiety Disorder scale (GAD2) with a positive screen cutoff of 3 for both. We analyzed the weighted prevalence of symptoms of anxiety, depression, and mental healthcare utilization for individuals with and without IBD using descriptive statistics. We compared prevalence and utilization estimates using logistic regression, adjusted for age, sex, race, ethnicity, and health insurance status.
Results: Of adults sampled in the 2023 NHIS (n = 29522), 572 reported a history of IBD (UC:n = 390; CD:n = 135; UC/CD:n=44), corresponding to approximately 4.2 million adults with IBD in the United States. (Table 1) There was a significantly higher prevalence of positive screening for anxiety/depression in those with IBD compared to those without IBD (14.3% v. 9.5% and 10.9% v. 6.9%, respectively;P < .001). The odds of screening positive for anxiety and depression was twice that for those with compared to those without IBD (anxiety: OR 2.0,95%CI 1.5-2.8; depression: OR 2.0, 95%CI 1.5-2.7). Approximately a quarter of individuals with IBD received counseling/therapy over the preceding 12 months, twice the odds of those without IBD (OR 2.0,95%CI 1.6-2.6). Among those with IBD who screened positive for anxiety/depression, 40-53% received counseling/therapy from a mental health professional, while 20-29% either did not receive or delayed counseling/therapy due to cost. (Figure 1)
Discussion: Among a nationally representative population of adults with IBD, approximately 1 in 7 screen positive for anxiety and 1 in 10 screen positive for depression, which is twice the odds of adults without IBD. Among those with IBD who screen positive for anxiety/depression up to a quarter forgo or delay counseling/therapy due to cost. Innovations to address cost related barriers to counseling and therapy for patients with IBD and symptoms of anxiety or depression are needed.
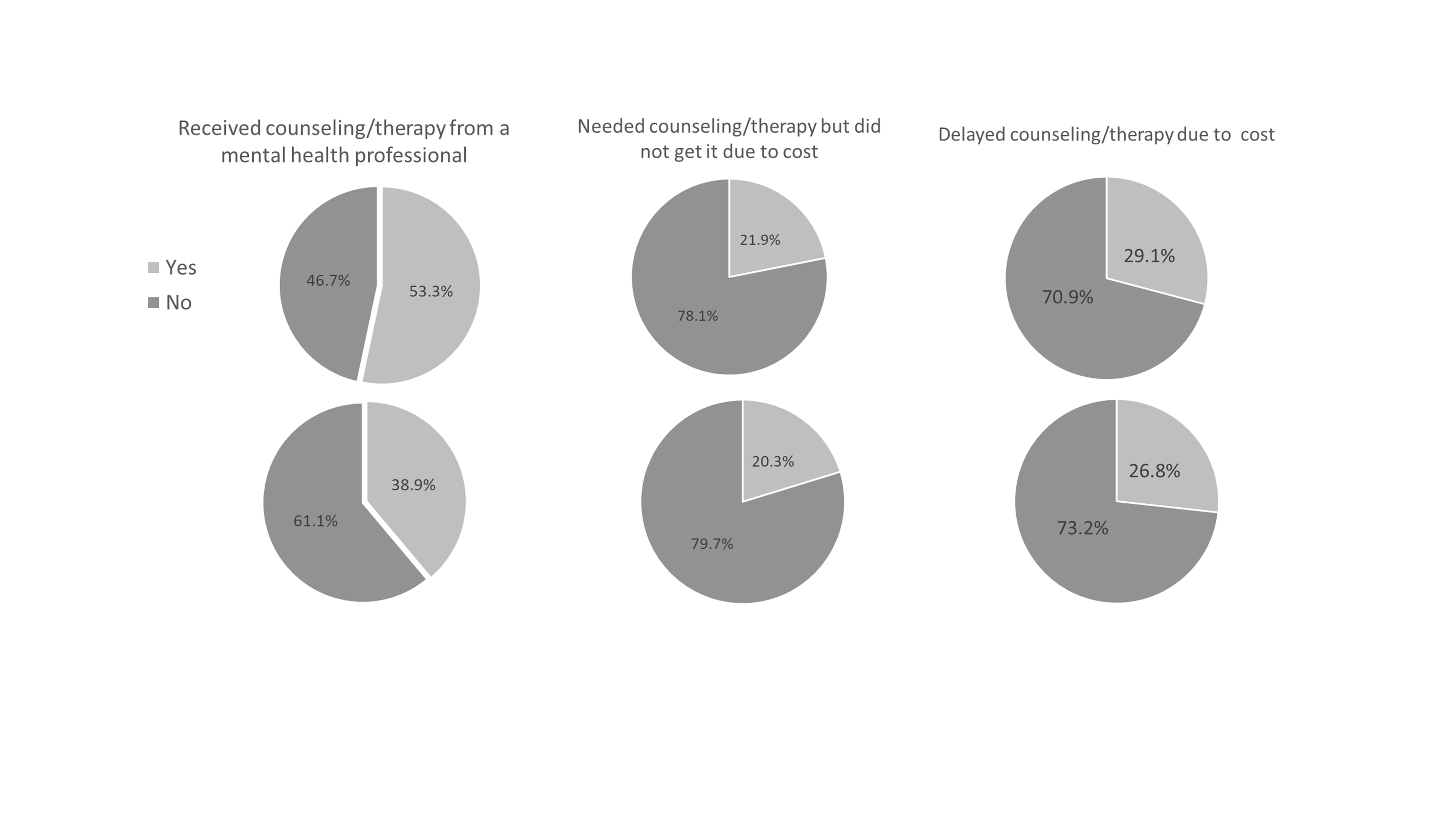
Figure: Figure 1. Counseling and therapy use and affordability among adults with IBD who screen positive for anxiety or depression. In a nationally representative population of US adults with IBD who screen positive for anxiety (top panel) or depression (bottom panel), approximately 40-53% received counseling/therapy over the preceding 12 months, while 20-29% either did not receive or delayed counseling/therapy due to cost.
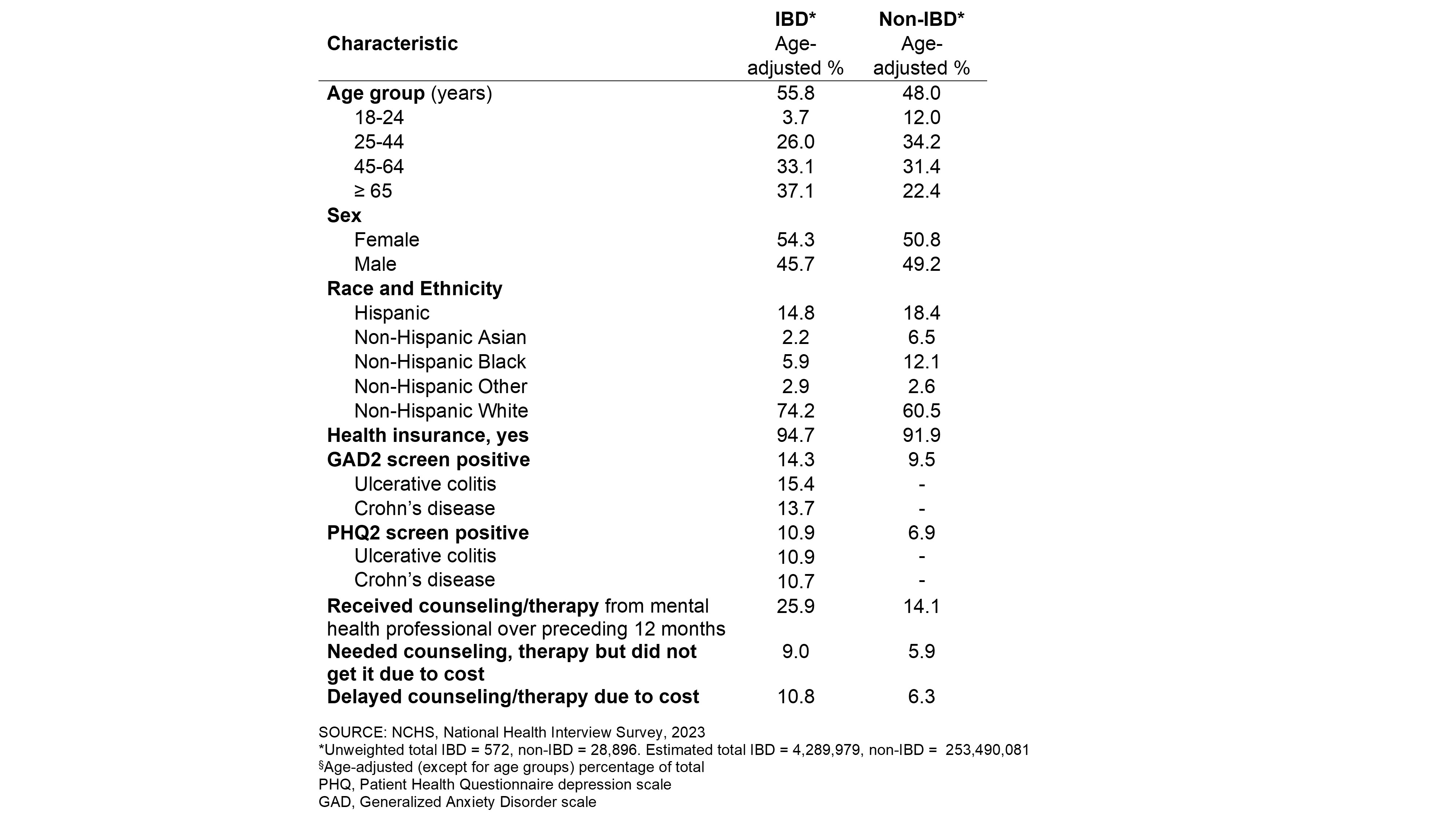
Figure: Table 1. Characteristics of US Adults by Inflammatory Bowel Disease (IBD) Diagnosis
Disclosures:
Ruby Greywoode: Janssen Scientific Affairs – Grant/Research Support. Sanofi – Consultant.
David Lounsbury indicated no relevant financial relationships.
Thomas Ullman: Bristol Myers Squibb – Consultant. J&J – Consultant. Pfizer – Consultant.
Laurie Keefer: AbbVie – Consultant. Ardelyx – Consultant. Eli Lilly – Consultant. Janssen – Consultant. Pfizer – Consultant. Reckitt Health – Consultant. Trellus Health – Owner/Ownership Interest, Stock-publicly held company(excluding mutual/index funds).
Ruby Greywoode, MD, MS1, David W. Lounsbury, PhD2, Thomas Ullman, MD3, Laurie Keefer, PhD, FACG4. P5375 - National Burden of Anxiety/Depression Symptoms and Counseling/Therapy Utilization Among Adults With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
