Tuesday Poster Session
Category: IBD
P5365 - Cardiovascular Outcomes and Intervention Rates in Hospitalized Patients With Inflammatory Bowel Disease: A Nationwide Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Sneh Sonaiya, MD, MPH, MBA
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Sneh Sonaiya, MD, MPH, MBA1, Raj H. Patel, MD2, Charmy Parikh, MD3, Magnus Chun, MD1, Pranav Patel, MD4, Ahmad Gill, MD5, Kyaw Min Tun, DO6
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2St. Mary Medical Center, Langhorne, PA; 3Mercy Catholic Medical Center, Darby, PA; 4Geisinger Health System, Danville, PA; 5University of California Davis Health Graduate Medical Education, Sacramento, CA; 6Creighton University School of Medicine, Omaha, NE
Introduction: Inflammatory bowel disease (IBD) has been associated with systemic inflammation, which may contribute to an increased risk of cardiovascular (CV) disease. However, the relationship between IBD and CV outcomes remains unclear. This study aims to compare the CV outcomes in hospitalized patients with and without IBD using a large national database.
Methods: This study utilized the National Inpatient Sample (NIS) database from 2016 to 2020 to identify adult hospitalizations (age >18 years) stratified into two cohorts based on the presence or absence of IBD to evaluate cardiovascular outcomes. Statistical analyses were conducted using SAS 9.4. Multivariate logistic regression was performed to evaluate the association between IBD and cardiovascular outcomes, adjusting for demographics (age, gender), comorbidities, and hospital characteristics.
Results: A total of 173 million hospitalizations without IBD and 1,652,070 hospitalizations with IBD from 2016 to 2020 were analyzed. IBD cohort, compared to non-IBD cohort was associated with significantly lower rates of ST-elevation myocardial infarction (STEMI) (0.31% vs. 0.61%, p< 0.0001), and non-ST-elevation myocardial infarction (NSTEMI) (1.2% vs. 2.07%, p < 0.0001), HFrEF (2.63% vs. 4.26%, p< 0.0001), HFpEF (4.29% vs. 5.78%, p< 0.0001). Similarly, the IBD cohort, compared to the non-IBD cohort also had a significantly lower inpatient burden of atrial fibrillation (10.57% vs. 12.83%, p< 0.0001) and ventricular fibrillation (0.14% vs. 0.22%, p< 0.0001). In contrast, thrombotic events were more frequent in IBD patients, with pulmonary embolism (PE) occurring in 1.3% vs. 1.11% (p< 0.0001) and venous thromboembolism (VTE) in 2.6% vs. 1.71% (p < 0.0001). The rate of advanced cardiovascular interventions was lower in the IBD cohort, with percutaneous coronary intervention performed in 0.5% vs. 0.93% (p< 0.0001), coronary artery bypass grafting in 0.28% vs. 0.55% (p< 0.0001), and cardiac resynchronization therapy in 0.23% vs. 0.43% (p< 0.0001).
Discussion: Hospitalized patients with IBD had lower rates of several CV outcomes compared to non-IBD cohort. However, VTE/PE was more frequent in the IBD cohort, supporting the need for VTE prophylaxis in IBD patients during hospitalization in this population. These findings highlight the complex association of systemic inflammation secondary to underlying IBD and cardiovascular outcomes. Further research is warranted to understand the underlying mechanisms and inform tailored prevention and management strategies.
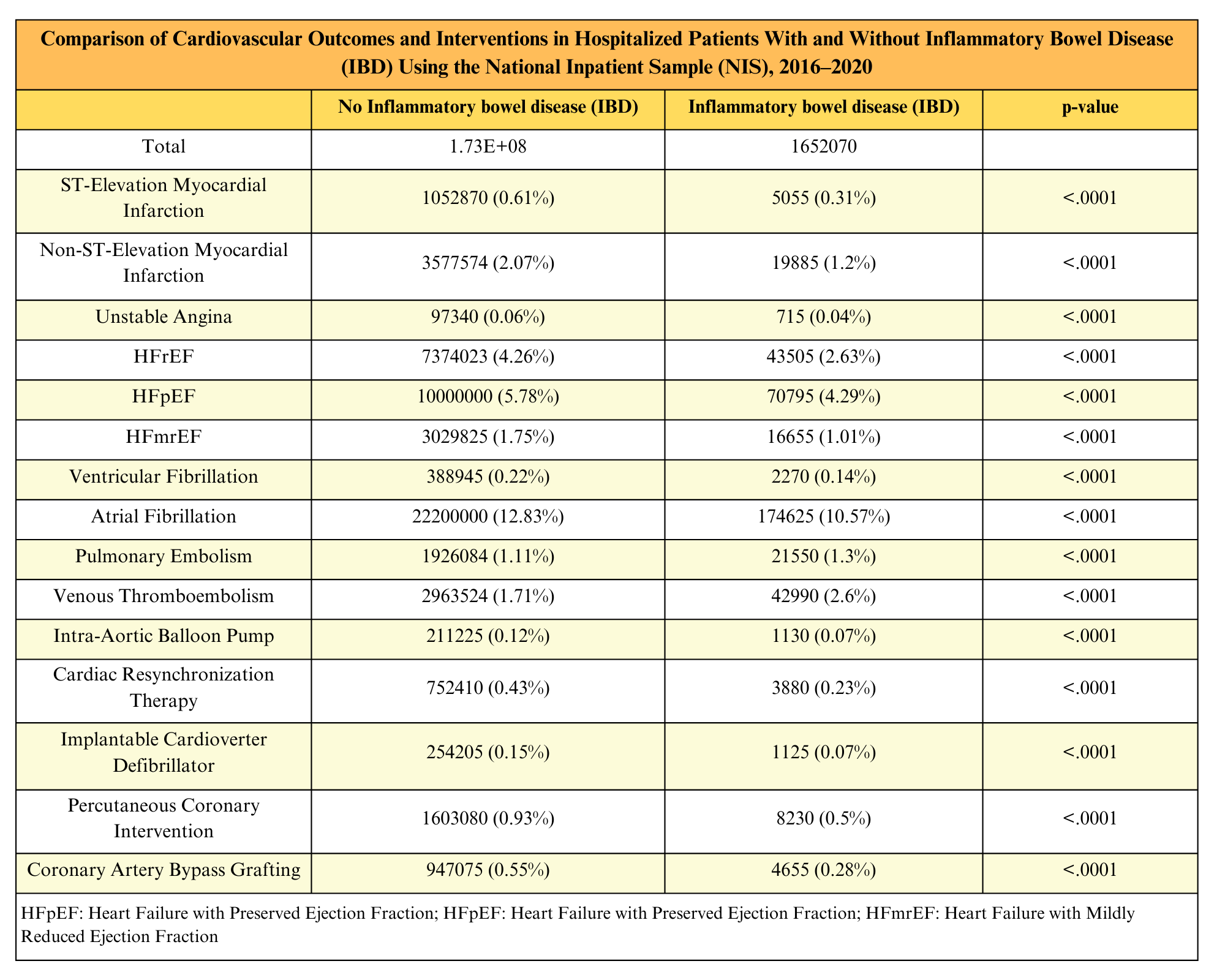
Figure: Table 1: Comparison of Cardiovascular Outcomes and Interventions in Hospitalized Patients With and Without Inflammatory Bowel Disease
(IBD) Using the National Inpatient Sample (NIS), 2016-2020
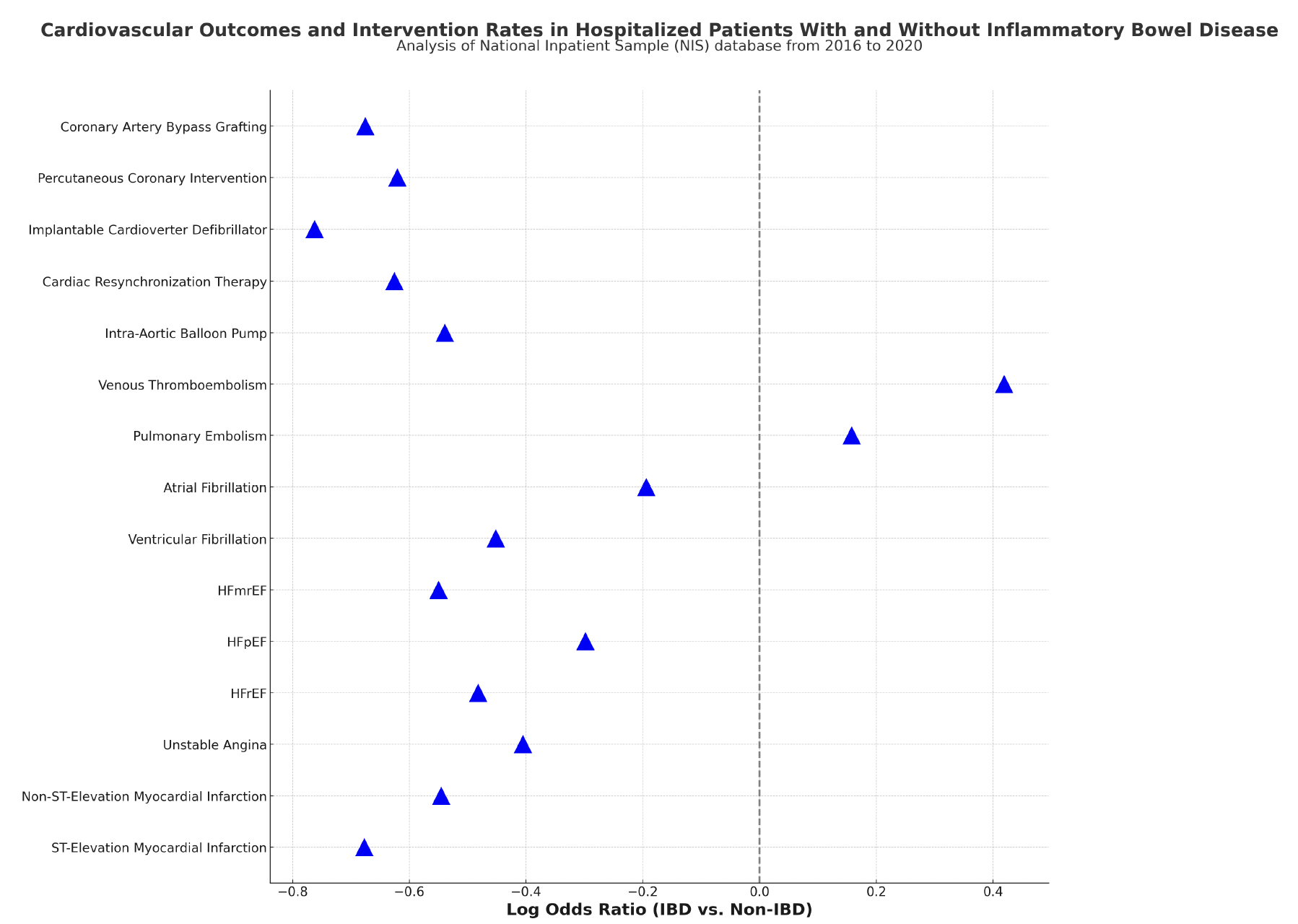
Figure: Figure 2: Log Odds Ratios of Cardiovascular Outcomes and Interventions in Hospitalized Patients With vs. Without Inflammatory Bowel Disease (IBD)
This figure presents the log odds ratios comparing the likelihood of various cardiovascular outcomes and interventions among hospitalized patients with IBD versus those without IBD, using data from the National Inpatient Sample (NIS) database from 2016 to 2020. Negative values indicate lower odds in patients with IBD, while positive values indicate higher odds.
Disclosures:
Sneh Sonaiya indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Magnus Chun indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Ahmad Gill indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Sneh Sonaiya, MD, MPH, MBA1, Raj H. Patel, MD2, Charmy Parikh, MD3, Magnus Chun, MD1, Pranav Patel, MD4, Ahmad Gill, MD5, Kyaw Min Tun, DO6. P5365 - Cardiovascular Outcomes and Intervention Rates in Hospitalized Patients With Inflammatory Bowel Disease: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2St. Mary Medical Center, Langhorne, PA; 3Mercy Catholic Medical Center, Darby, PA; 4Geisinger Health System, Danville, PA; 5University of California Davis Health Graduate Medical Education, Sacramento, CA; 6Creighton University School of Medicine, Omaha, NE
Introduction: Inflammatory bowel disease (IBD) has been associated with systemic inflammation, which may contribute to an increased risk of cardiovascular (CV) disease. However, the relationship between IBD and CV outcomes remains unclear. This study aims to compare the CV outcomes in hospitalized patients with and without IBD using a large national database.
Methods: This study utilized the National Inpatient Sample (NIS) database from 2016 to 2020 to identify adult hospitalizations (age >18 years) stratified into two cohorts based on the presence or absence of IBD to evaluate cardiovascular outcomes. Statistical analyses were conducted using SAS 9.4. Multivariate logistic regression was performed to evaluate the association between IBD and cardiovascular outcomes, adjusting for demographics (age, gender), comorbidities, and hospital characteristics.
Results: A total of 173 million hospitalizations without IBD and 1,652,070 hospitalizations with IBD from 2016 to 2020 were analyzed. IBD cohort, compared to non-IBD cohort was associated with significantly lower rates of ST-elevation myocardial infarction (STEMI) (0.31% vs. 0.61%, p< 0.0001), and non-ST-elevation myocardial infarction (NSTEMI) (1.2% vs. 2.07%, p < 0.0001), HFrEF (2.63% vs. 4.26%, p< 0.0001), HFpEF (4.29% vs. 5.78%, p< 0.0001). Similarly, the IBD cohort, compared to the non-IBD cohort also had a significantly lower inpatient burden of atrial fibrillation (10.57% vs. 12.83%, p< 0.0001) and ventricular fibrillation (0.14% vs. 0.22%, p< 0.0001). In contrast, thrombotic events were more frequent in IBD patients, with pulmonary embolism (PE) occurring in 1.3% vs. 1.11% (p< 0.0001) and venous thromboembolism (VTE) in 2.6% vs. 1.71% (p < 0.0001). The rate of advanced cardiovascular interventions was lower in the IBD cohort, with percutaneous coronary intervention performed in 0.5% vs. 0.93% (p< 0.0001), coronary artery bypass grafting in 0.28% vs. 0.55% (p< 0.0001), and cardiac resynchronization therapy in 0.23% vs. 0.43% (p< 0.0001).
Discussion: Hospitalized patients with IBD had lower rates of several CV outcomes compared to non-IBD cohort. However, VTE/PE was more frequent in the IBD cohort, supporting the need for VTE prophylaxis in IBD patients during hospitalization in this population. These findings highlight the complex association of systemic inflammation secondary to underlying IBD and cardiovascular outcomes. Further research is warranted to understand the underlying mechanisms and inform tailored prevention and management strategies.
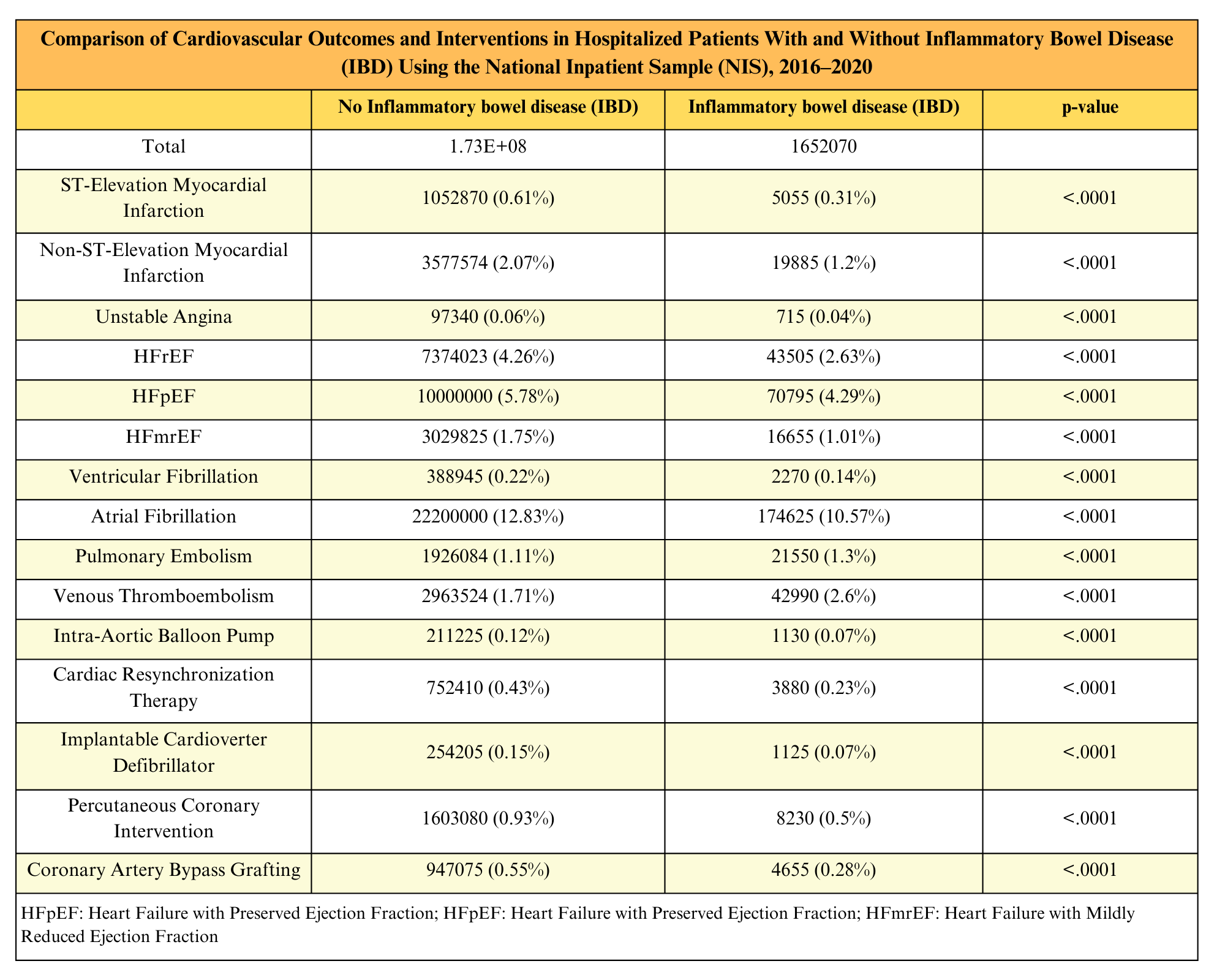
Figure: Table 1: Comparison of Cardiovascular Outcomes and Interventions in Hospitalized Patients With and Without Inflammatory Bowel Disease
(IBD) Using the National Inpatient Sample (NIS), 2016-2020
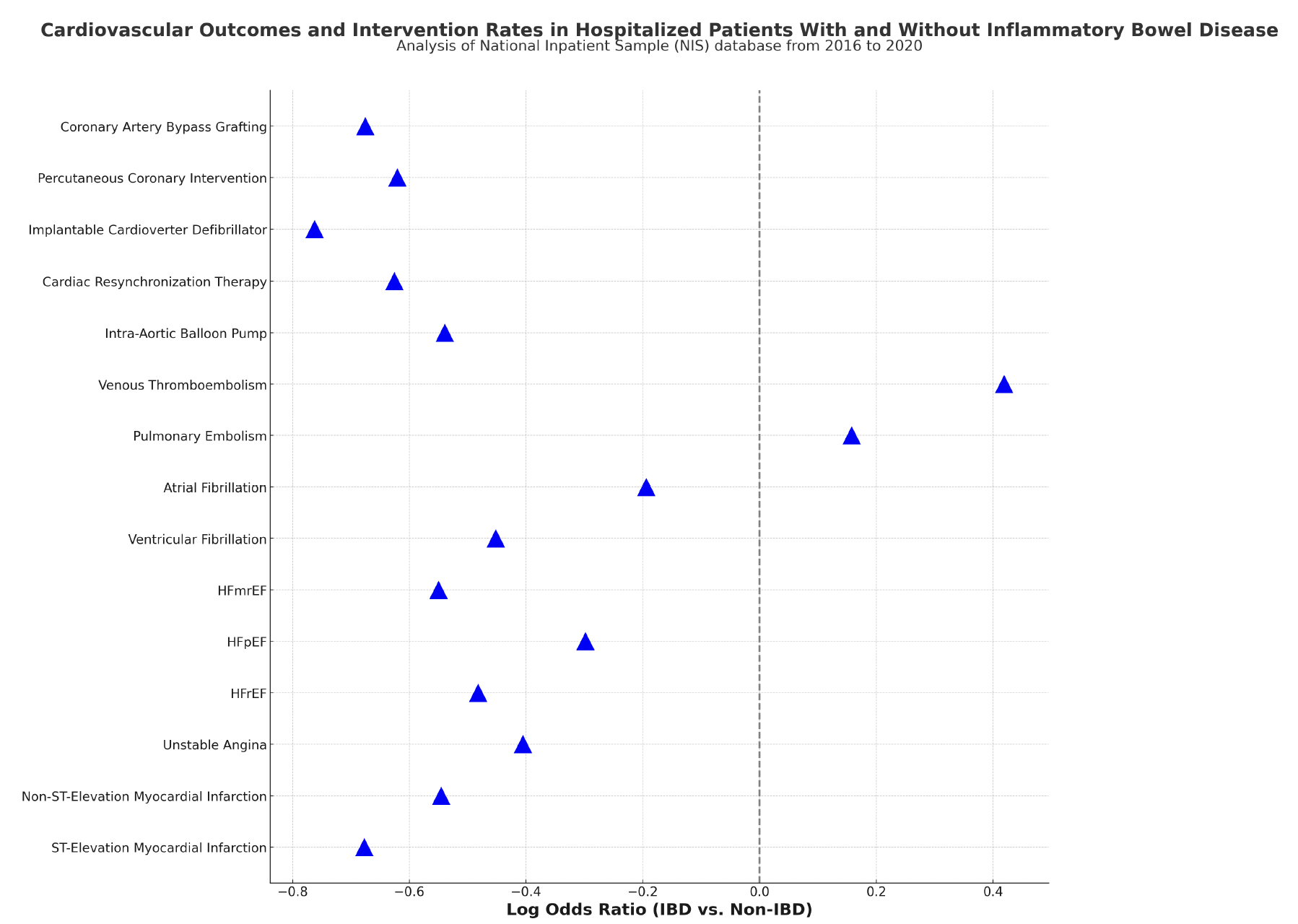
Figure: Figure 2: Log Odds Ratios of Cardiovascular Outcomes and Interventions in Hospitalized Patients With vs. Without Inflammatory Bowel Disease (IBD)
This figure presents the log odds ratios comparing the likelihood of various cardiovascular outcomes and interventions among hospitalized patients with IBD versus those without IBD, using data from the National Inpatient Sample (NIS) database from 2016 to 2020. Negative values indicate lower odds in patients with IBD, while positive values indicate higher odds.
Disclosures:
Sneh Sonaiya indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Magnus Chun indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Ahmad Gill indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Sneh Sonaiya, MD, MPH, MBA1, Raj H. Patel, MD2, Charmy Parikh, MD3, Magnus Chun, MD1, Pranav Patel, MD4, Ahmad Gill, MD5, Kyaw Min Tun, DO6. P5365 - Cardiovascular Outcomes and Intervention Rates in Hospitalized Patients With Inflammatory Bowel Disease: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
