Tuesday Poster Session
Category: IBD
P5359 - Elderly Onset versus Adult Onset Inflammatory Bowel Disease: A Retrospective Comparative Analysis of Clinical Characteristics, Treatment Patterns, and Outcomes
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Fariha Hasan, MD
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Fariha Hasan, MD1, Julia Pierson, BS2, Rebecca Case, BS2, Krystal Hunter, PhD, MBA1, Sangita Phadtare, BS, MS, PhD2, Thomas Judge, MD1
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ
Introduction: The prevalence of inflammatory bowel disease (IBD) in older adults is rising, yet elderly-onset IBD remains undercharacterized due to limited trial inclusion. Understanding disease behavior and treatment patterns in this population is essential for improving outcomes.
Methods: We conducted a retrospective review of 180 patients aged ≥60 years with confirmed Crohn’s disease (CD) or ulcerative colitis (UC) at a tertiary care center between 2015 and 2024. Patients were stratified by age at diagnosis: elderly-onset (≥65 years) and adult-onset (< 65 years). Disease extent, severity, treatment regimens, and surgical history were extracted. Subgroup comparisons between UC and CD, and multivariable logistic regression identified predictors of remission, surgery, and biologic use. Chi-square test was used for categorical variables and independent t-test for continuous variables.
Results: Of 180 patients, 26 (14.4%) had elderly-onset IBD. These patients were older at review (mean 81.5 vs. 67.4 years, p< 0.001) and had shorter disease duration (10.5 vs. 23.0 years, p< 0.001). Cardiac disease (69.2% vs. 42.2%, p=0.011) and malignancy (80.8% vs. 59.7%, p=0.040) were more common in elderly-onset IBD. Depression was less prevalent (11.5% vs. 35.1%, p=0.017). Surgical rates and biologic use were similar, though elderly patients had lower odds of receiving immune-modifying therapies (OR=0.916, p=0.016), and advanced therapy use with age (OR=0.908, p=0.024). CD patients were more likely to undergo surgery (57.8% vs. 25.3%, p< 0.001), while UC patients had higher rates of mesalamine and vedolizumab use. Regression analysis showed elderly-onset UC was independently associated with higher odds of remission (OR=18.69, p=0.024), while cancer history predicted increased surgical risk (OR=3.98, p< 0.001) and reduced remission in CD (OR=0.30, p=0.044). Increasing age was inversely associated with use of advanced therapies. Biologic preferences differed by disease type, with vedolizumab more commonly used in UC, and newer agents like risankizumab and tofacitinib favored in CD.
Discussion: Elderly-onset IBD patients exhibit distinct clinical features, including higher comorbidity burden and different treatment patterns. Despite lower use of advanced therapies, remission rates were comparable, suggesting a potentially less aggressive disease course or more conservative management. These findings underscore the need for age-tailored treatment approaches and greater inclusion of elderly patients in IBD trials.
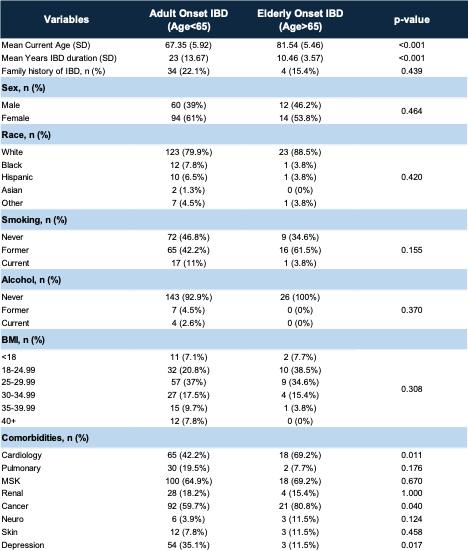
Figure: Table 1: Demographics between adult-onset and elderly-onset IBD
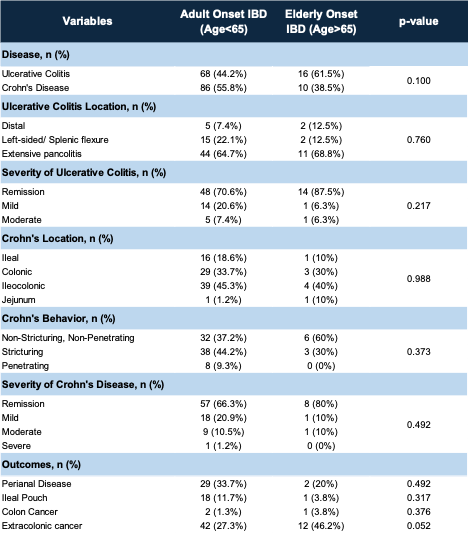
Figure: Table 2: Outcomes between adult-onset and elderly-onset IBD
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Julia Pierson indicated no relevant financial relationships.
Rebecca Case indicated no relevant financial relationships.
Krystal Hunter indicated no relevant financial relationships.
Sangita Phadtare indicated no relevant financial relationships.
Thomas Judge indicated no relevant financial relationships.
Fariha Hasan, MD1, Julia Pierson, BS2, Rebecca Case, BS2, Krystal Hunter, PhD, MBA1, Sangita Phadtare, BS, MS, PhD2, Thomas Judge, MD1. P5359 - Elderly Onset versus Adult Onset Inflammatory Bowel Disease: A Retrospective Comparative Analysis of Clinical Characteristics, Treatment Patterns, and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School of Rowan University, Camden, NJ
Introduction: The prevalence of inflammatory bowel disease (IBD) in older adults is rising, yet elderly-onset IBD remains undercharacterized due to limited trial inclusion. Understanding disease behavior and treatment patterns in this population is essential for improving outcomes.
Methods: We conducted a retrospective review of 180 patients aged ≥60 years with confirmed Crohn’s disease (CD) or ulcerative colitis (UC) at a tertiary care center between 2015 and 2024. Patients were stratified by age at diagnosis: elderly-onset (≥65 years) and adult-onset (< 65 years). Disease extent, severity, treatment regimens, and surgical history were extracted. Subgroup comparisons between UC and CD, and multivariable logistic regression identified predictors of remission, surgery, and biologic use. Chi-square test was used for categorical variables and independent t-test for continuous variables.
Results: Of 180 patients, 26 (14.4%) had elderly-onset IBD. These patients were older at review (mean 81.5 vs. 67.4 years, p< 0.001) and had shorter disease duration (10.5 vs. 23.0 years, p< 0.001). Cardiac disease (69.2% vs. 42.2%, p=0.011) and malignancy (80.8% vs. 59.7%, p=0.040) were more common in elderly-onset IBD. Depression was less prevalent (11.5% vs. 35.1%, p=0.017). Surgical rates and biologic use were similar, though elderly patients had lower odds of receiving immune-modifying therapies (OR=0.916, p=0.016), and advanced therapy use with age (OR=0.908, p=0.024). CD patients were more likely to undergo surgery (57.8% vs. 25.3%, p< 0.001), while UC patients had higher rates of mesalamine and vedolizumab use. Regression analysis showed elderly-onset UC was independently associated with higher odds of remission (OR=18.69, p=0.024), while cancer history predicted increased surgical risk (OR=3.98, p< 0.001) and reduced remission in CD (OR=0.30, p=0.044). Increasing age was inversely associated with use of advanced therapies. Biologic preferences differed by disease type, with vedolizumab more commonly used in UC, and newer agents like risankizumab and tofacitinib favored in CD.
Discussion: Elderly-onset IBD patients exhibit distinct clinical features, including higher comorbidity burden and different treatment patterns. Despite lower use of advanced therapies, remission rates were comparable, suggesting a potentially less aggressive disease course or more conservative management. These findings underscore the need for age-tailored treatment approaches and greater inclusion of elderly patients in IBD trials.
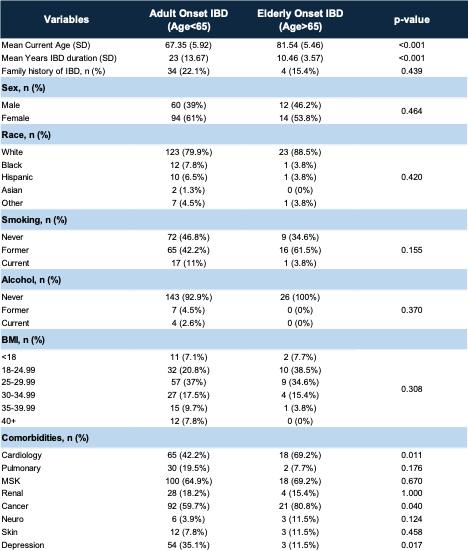
Figure: Table 1: Demographics between adult-onset and elderly-onset IBD
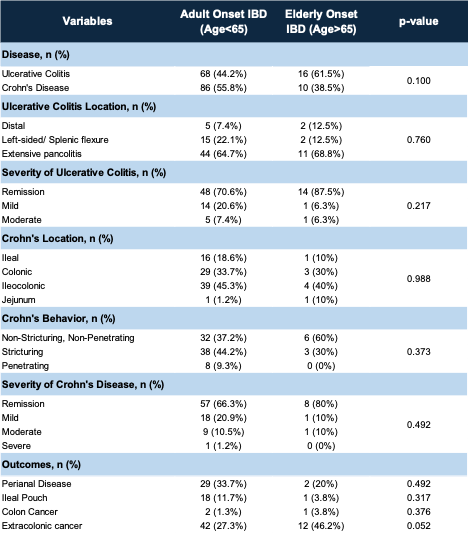
Figure: Table 2: Outcomes between adult-onset and elderly-onset IBD
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Julia Pierson indicated no relevant financial relationships.
Rebecca Case indicated no relevant financial relationships.
Krystal Hunter indicated no relevant financial relationships.
Sangita Phadtare indicated no relevant financial relationships.
Thomas Judge indicated no relevant financial relationships.
Fariha Hasan, MD1, Julia Pierson, BS2, Rebecca Case, BS2, Krystal Hunter, PhD, MBA1, Sangita Phadtare, BS, MS, PhD2, Thomas Judge, MD1. P5359 - Elderly Onset versus Adult Onset Inflammatory Bowel Disease: A Retrospective Comparative Analysis of Clinical Characteristics, Treatment Patterns, and Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
