Tuesday Poster Session
Category: IBD
P5356 - Fecal Microbiota Transplantation in IBD: A Meta-Analysis of Remission and Mucosal Healing Outcomes From Randomized Trials
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Prince Shah-Riar, MD (he/him/his)
DHR Health, Edinburg, Tx
Edinburg, TX
Presenting Author(s)
Prince Shah-Riar, MD1, Sadeed Araf Reza, MBBS2, Mahanaz Nabi. Ansa, MBBS3, Syeda Salima Sultana, MD4, Asif Zamir, MD, FACG5
1DHR Health, Edinburg, Tx, McAllen, TX; 2Sir Salimullah Medical College (Mitford), Dhaka, Dhaka, Bangladesh; 3Sylhet MAG Osmani Medical College Hospital, Sylhet, Sylhet, Bangladesh; 4NYC Health + Hospitals/South Brooklyn Health, Brooklyn, NY; 5DHR Health Gastroenterology, Edinburg, TX
Introduction: Inflammatory Bowel Disease (IBD), encompassing ulcerative colitis (UC) and Crohn’s disease (CD), remains a chronic relapsing condition with significant morbidity. While standard therapies target immune dysregulation, mounting evidence suggests a pivotal role for microbial dysbiosis. Fecal Microbiota Transplantation (FMT), a microbial restoration therapy, has shown promise in Clostridioides difficile infection but its therapeutic utility in IBD remains unclear due to inconsistent findings and heterogeneous endpoints. This study aimed to evaluate the efficacy of FMT in inducing clinical remission and mucosal healing in patients with UC and CD by synthesizing randomized controlled trial (RCT) data from 2020 to 2025.
Methods: A systematic review and meta-analysis was conducted per PRISMA guidelines. Comprehensive searches were performed in PubMed, Cochrane, ClinicalTrials.gov, Google Scholar, and PLOS One using predefined Boolean strategies targeting FMT, IBD, remission, and mucosal healing. RCTs enrolling adult patients with UC or CD receiving FMT versus placebo or standard care were included. Primary endpoints were clinical remission and mucosal healing; secondary outcomes included adverse events and microbiome composition shifts. Data were pooled using random-effects models to generate risk ratios (RR) and 95% confidence intervals (CI).
Results: Out of 537 screened studies, 7 high-quality RCTs (n=542) met inclusion criteria.
Discussion: FMT improves both clinical and endoscopic outcomes in IBD, with acceptable safety. These findings support further investigation in biomarker-stratified populations and optimization of donor selection. Importantly, this study addresses the research gap between proof-of-concept studies and therapeutic standardization. FMT represents a viable adjunctive therapy for IBD algorithms., particularly UC, with demonstrable efficacy in remission induction and mucosal healing. Large-scale, multi-center trials with unified endpoints are now essential to refine its role in IBD treatment
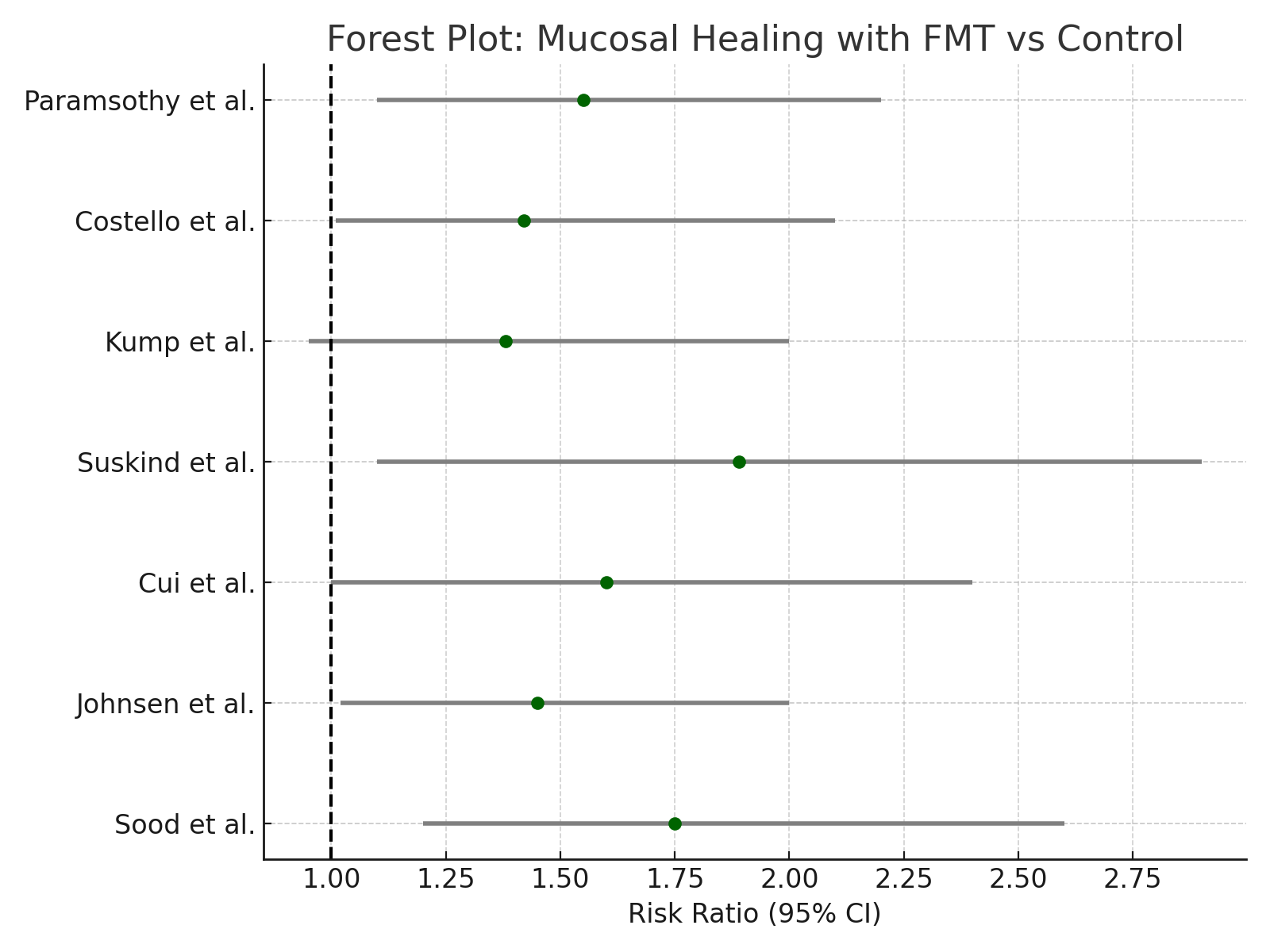
Figure: Figure 1: Forest Plot of Mucosal Healing Rates: Fecal Microbiota Transplantation vs. Control
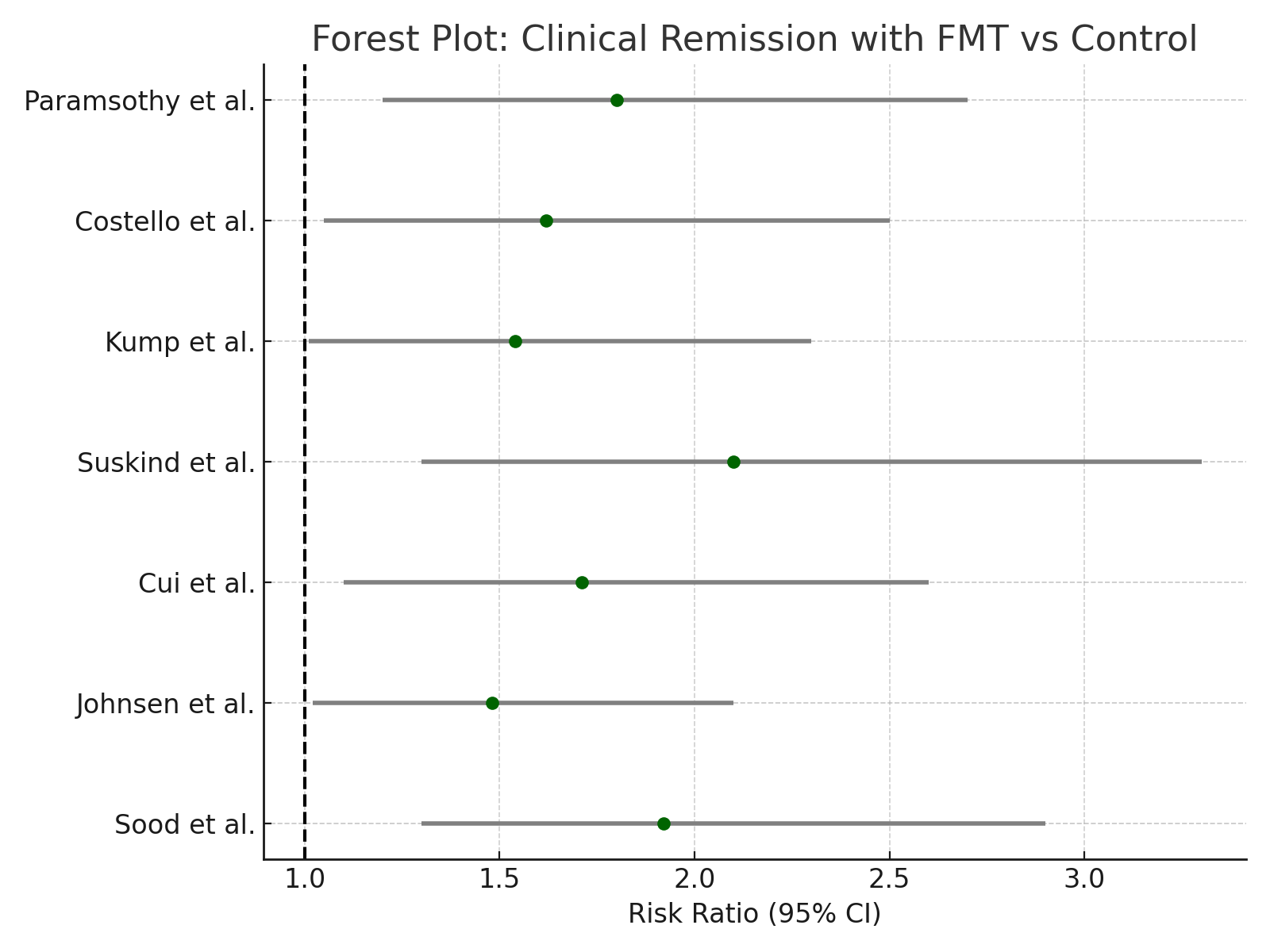
Figure: Figure 2: Forest Plot of Clinical Remission Rates: Fecal Microbiota Transplantation vs. Control
Disclosures:
Prince Shah-Riar indicated no relevant financial relationships.
Sadeed Araf Reza indicated no relevant financial relationships.
Mahanaz Ansa indicated no relevant financial relationships.
Syeda Salima Sultana indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Prince Shah-Riar, MD1, Sadeed Araf Reza, MBBS2, Mahanaz Nabi. Ansa, MBBS3, Syeda Salima Sultana, MD4, Asif Zamir, MD, FACG5. P5356 - Fecal Microbiota Transplantation in IBD: A Meta-Analysis of Remission and Mucosal Healing Outcomes From Randomized Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1DHR Health, Edinburg, Tx, McAllen, TX; 2Sir Salimullah Medical College (Mitford), Dhaka, Dhaka, Bangladesh; 3Sylhet MAG Osmani Medical College Hospital, Sylhet, Sylhet, Bangladesh; 4NYC Health + Hospitals/South Brooklyn Health, Brooklyn, NY; 5DHR Health Gastroenterology, Edinburg, TX
Introduction: Inflammatory Bowel Disease (IBD), encompassing ulcerative colitis (UC) and Crohn’s disease (CD), remains a chronic relapsing condition with significant morbidity. While standard therapies target immune dysregulation, mounting evidence suggests a pivotal role for microbial dysbiosis. Fecal Microbiota Transplantation (FMT), a microbial restoration therapy, has shown promise in Clostridioides difficile infection but its therapeutic utility in IBD remains unclear due to inconsistent findings and heterogeneous endpoints. This study aimed to evaluate the efficacy of FMT in inducing clinical remission and mucosal healing in patients with UC and CD by synthesizing randomized controlled trial (RCT) data from 2020 to 2025.
Methods: A systematic review and meta-analysis was conducted per PRISMA guidelines. Comprehensive searches were performed in PubMed, Cochrane, ClinicalTrials.gov, Google Scholar, and PLOS One using predefined Boolean strategies targeting FMT, IBD, remission, and mucosal healing. RCTs enrolling adult patients with UC or CD receiving FMT versus placebo or standard care were included. Primary endpoints were clinical remission and mucosal healing; secondary outcomes included adverse events and microbiome composition shifts. Data were pooled using random-effects models to generate risk ratios (RR) and 95% confidence intervals (CI).
Results: Out of 537 screened studies, 7 high-quality RCTs (n=542) met inclusion criteria.
- Clinical Remission: FMT significantly increased remission rates versus control (RR 1.74; 95% CI 1.29–2.34; p< 0.001; I² = 43%).
- Mucosal Healing: Observed in 38.2% of FMT recipients vs 24.6% of controls (RR 1.53; 95% CI 1.10–2.13; p=0.01).
- Adverse Events: No significant increase in serious adverse events (RR 0.98; 95% CI 0.64–1.48).
- Subgroup analysis suggested higher efficacy in multi-donor FMT protocols and lower baseline microbial diversity.
Discussion: FMT improves both clinical and endoscopic outcomes in IBD, with acceptable safety. These findings support further investigation in biomarker-stratified populations and optimization of donor selection. Importantly, this study addresses the research gap between proof-of-concept studies and therapeutic standardization. FMT represents a viable adjunctive therapy for IBD algorithms., particularly UC, with demonstrable efficacy in remission induction and mucosal healing. Large-scale, multi-center trials with unified endpoints are now essential to refine its role in IBD treatment
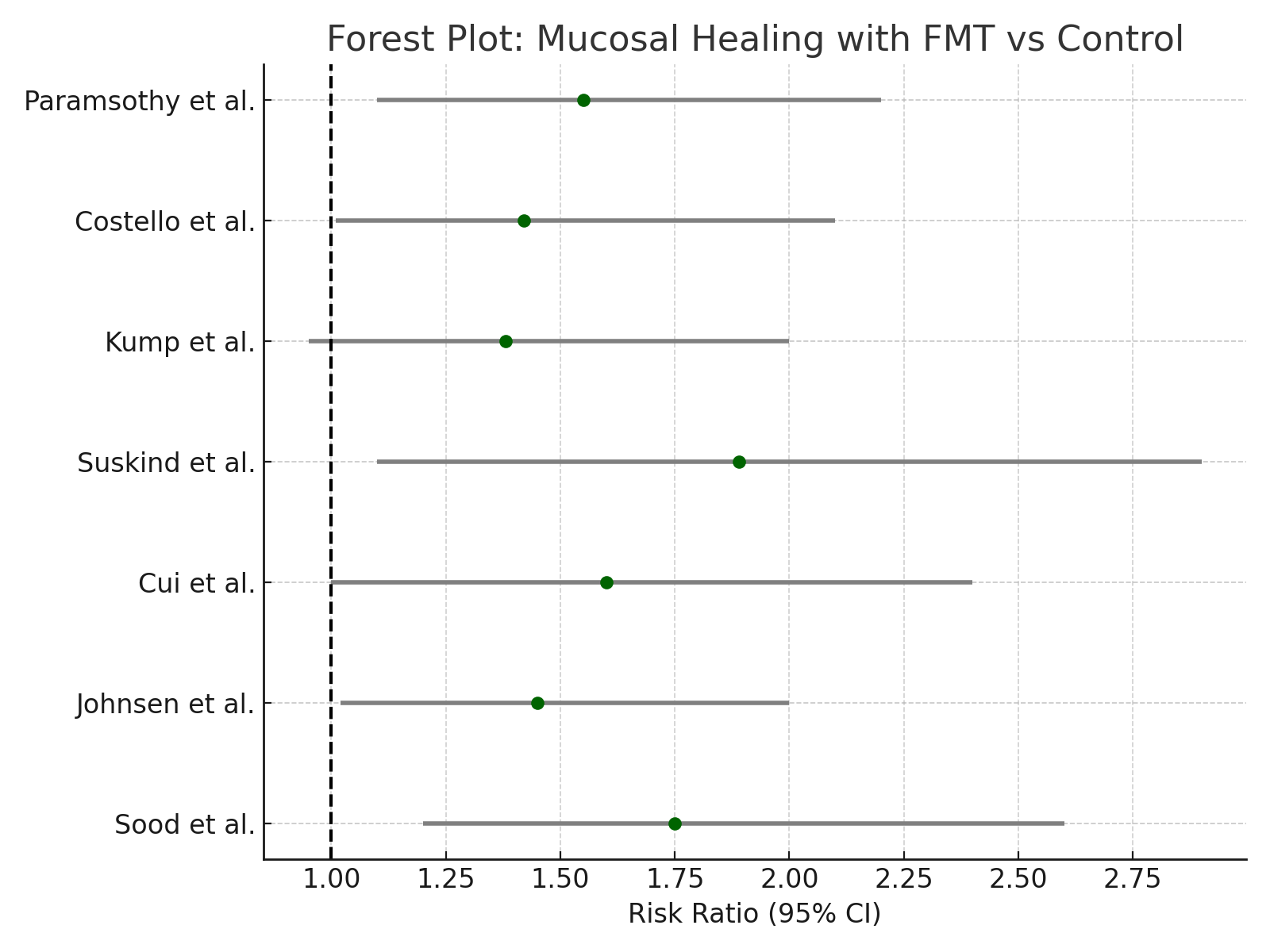
Figure: Figure 1: Forest Plot of Mucosal Healing Rates: Fecal Microbiota Transplantation vs. Control
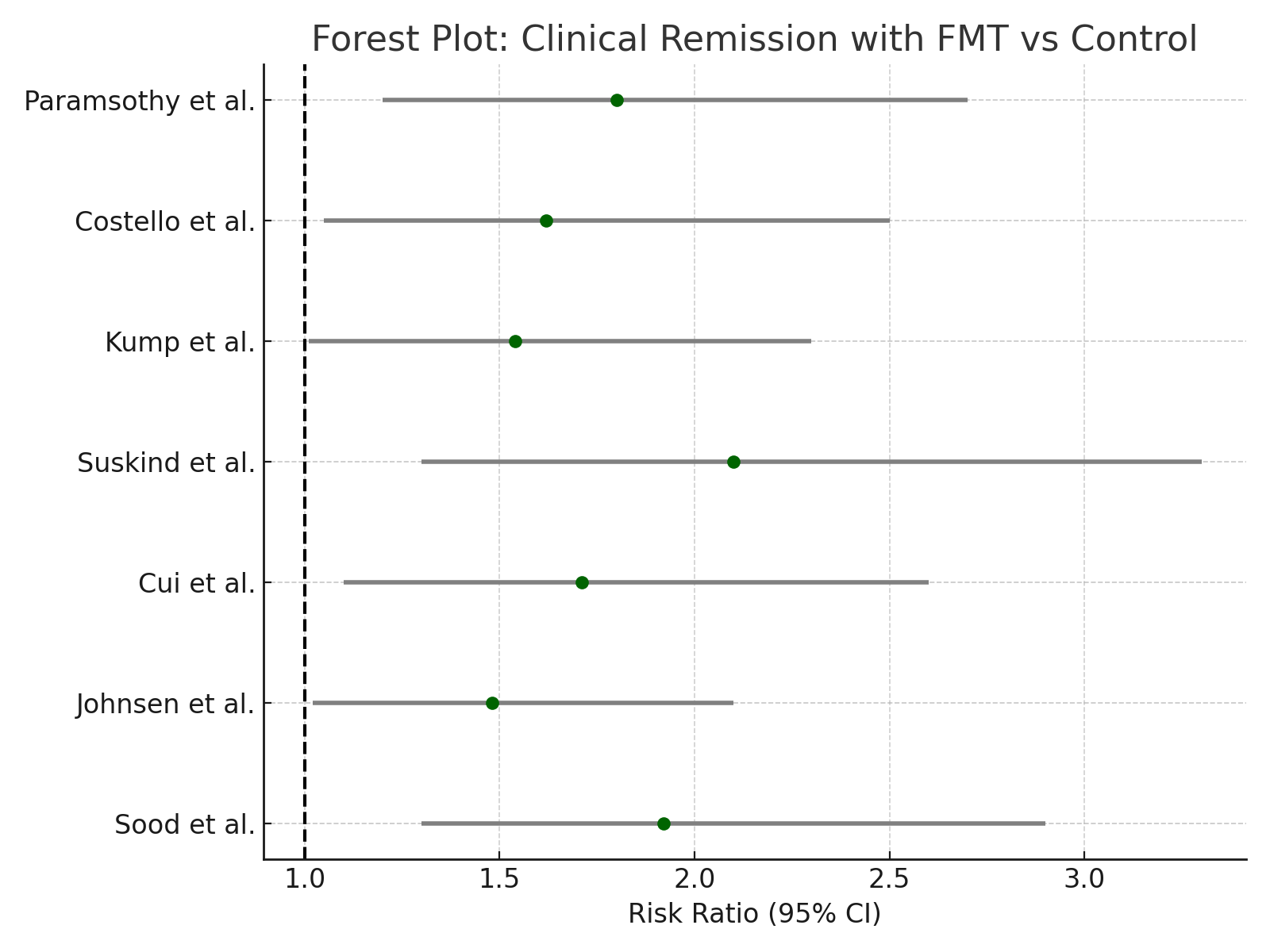
Figure: Figure 2: Forest Plot of Clinical Remission Rates: Fecal Microbiota Transplantation vs. Control
Disclosures:
Prince Shah-Riar indicated no relevant financial relationships.
Sadeed Araf Reza indicated no relevant financial relationships.
Mahanaz Ansa indicated no relevant financial relationships.
Syeda Salima Sultana indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Prince Shah-Riar, MD1, Sadeed Araf Reza, MBBS2, Mahanaz Nabi. Ansa, MBBS3, Syeda Salima Sultana, MD4, Asif Zamir, MD, FACG5. P5356 - Fecal Microbiota Transplantation in IBD: A Meta-Analysis of Remission and Mucosal Healing Outcomes From Randomized Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
