Tuesday Poster Session
Category: IBD
P5319 - Overall and Comparative Risk of Shingles With Advanced Therapies in Patients with Inflammatory Bowel Diseases
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SP
Soo-Kyung Park, MD, PhD (she/her/hers)
University of California San Diego
San Diego, CA
Presenting Author(s)
Dhruv Ahuja, MBBS1, Soo-Kyung Park, MD, PhD2, Kuan-Hung Yeh, 3, Sagar Patel, BS2, Shane Goodwin, PhD4, Christopher Ma, MD, MPH5, Namrata Singh, MD6, Ashwin Ananthakrishnan, 7, Vipul Jairath, MBChB, DPhil, MRCP8, Ronghui Xu, PhD2, Siddharth Singh, MD, MS2
1University of California San Diego, Delhi, Delhi, India; 2University of California San Diego, San Diego, CA; 3University of California San Diego, La Jolla, CA; 4Western University, London, ON, Canada; 5University of Calgary, Calgary, AB, Canada; 6University of Washington, Seattle, WA; 7Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA; 8Department of Medicine and Department of Epidemiology and Biostatistics, Western University, London, ON, Canada
Introduction: We conducted a retrospective cohort study comparing the risk of shingles with advanced therapies in patients with Inflammatory bowel disease (IBD)
Methods: Using an administrative claims database, we identified patients with IBD who initiated treatment with either tumor necrosis factor-α (TNF) antagonists (infliximab, adalimumab, golimumab and certolizumab pegol), anti-integrin agents (vedolizumab), anti-interleukin (IL)-12/23p40 or anti-IL-23p19 agents (ustekinumab, risankizumab, mirikizumab, collectively labeled anti-interleukins), or Janus kinase (JAK) inhibitors (tofacitinib, upadacitinib) between 2016 and 2023, and had insurance coverage for at least 1y before and after treatment initiation. We assessed the incidence rate (IR per 100 person-year [PY]) of shingles (overall and complicated, including post herpetic neuralgia ocular and neurologic involvement) and compared risks using inverse probability of treatment weighting (IPTW). Propensity scores were estimated through generalized boosted models incorporating demographics, comorbidities, healthcare utilization, and prior/concomitant IBD therapies. Weighted Cox models estimated hazard ratios (HR) and 95% confidence intervals (CI).
Results: We included 21,564 patients with IBD (mean age range, 45-49 years; 51-53% females; 6% with zoster vaccination) followed over 27 months. The incidence of shingles and complicated shingles varied with difference advanced therapies: TNF antagonists (n=9,385; IR of shingles/complicated shingles per 100-py, 1.00/0.30), anti-integrin agents (n=5,881; IR, 1.38/0.43), anti-interleukins (n=5,445; IR, 1.24/0.45) and JAK inhibitors (n=853; IR, 3.33/0.88). After adjusting for confounding variables using IPTW, JAK inhibitors were associated with higher risks of shingles compared with TNF antagonists (HR, 2.72 [95% CI, 1.67-4.43]), anti-integrin agents (HR, 2.41 [1.51-3.84]) and anti-IL 12/23p40 agents or anti-IL-23p19 (HR, 2.45 [1.53-3.95]). Similar trends were observed for risk of complicated shingles. No differences were observed in the risk of shingles between TNF antagonists, anti-integrins and anti-interleukins (Figure 1).
Discussion: In this large real-world cohort of patients with IBD, JAK inhibitors were associated with higher risks of overall shingles compared to other advanced therapies. No differences were observed in the risk of shingles with other advanced therapies, with overall incidence ranging from 1.0-1.4 per 100-py.
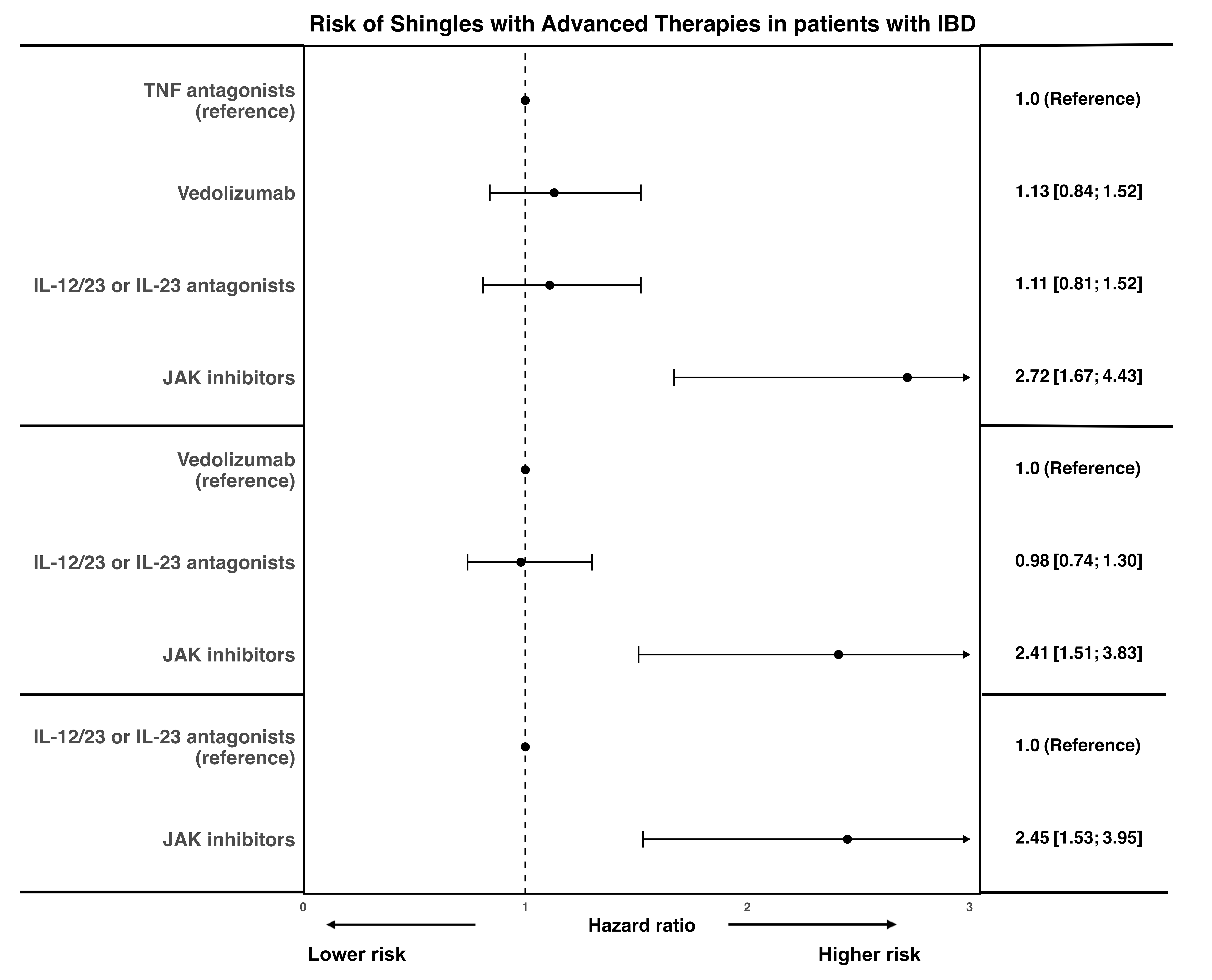
Figure: Figure 1. Comparative risk of shingles with advanced therapies in patients with IBD
Disclosures:
Dhruv Ahuja indicated no relevant financial relationships.
Soo-Kyung Park indicated no relevant financial relationships.
Kuan-Hung Yeh indicated no relevant financial relationships.
Sagar Patel indicated no relevant financial relationships.
Shane Goodwin indicated no relevant financial relationships.
Christopher Ma: Abbvie – Consultant, Grant/Research Support, speaker's fee. Alimentiv – Consultant, speaker's fee. Amgen – Consultant, speaker's fee. AVIR Pharma Inc. – Consultant, speaker's fee. Bristol Myers Squibb – Consultant, speaker's fee. Celltrion – Consultant. Eli Lilly – Consultant, Grant/Research Support, speaker's fee. Ferring – Consultant, Grant/Research Support, speaker's fee. Forte Biosciences – Consultant. Fresenius Kabi – Consultant, speaker's fee. Gilead – Consultant. Janssen – Consultant, speaker's fee. McKesson – Consultant. Merck – Speaker's fee. Mirador Therapeutics – Consultant. Mylan – Consultant. Organon – speaker's fee. Pendopharm – Consultant, speaker's fee. Pfizer – Consultant, Grant/Research Support, speaker's fee. Prometheus Biosciences Inc. – Consultant. Roche – Consultant. Sanofi – Consultant, speaker's fee. Springer Publishing – Royalties. Takeda – Consultant, speaker's fee. Tillotts Pharma – Consultant, speaker's fee.
Namrata Singh indicated no relevant financial relationships.
Ashwin Ananthakrishnan: Takeda – Grant/Research Support.
Vipul Jairath: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. Alimentiv – Consultant, Grant/Research Support. Arena Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Asahi Kasei Pharma – Consultant, Grant/Research Support, Speakers Bureau. Asieris Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. AstraZeneca – Consultant, Grant/Research Support, Speakers Bureau. Avoro Capital – Consultant. Bristol Myers Squibb – Consultant, Grant/Research Support, Speakers Bureau. Celltrion – Consultant, Grant/Research Support, Speakers Bureau. Eli Lilly and Company – Consultant, Grant/Research Support, Speakers Bureau. Endpoint Health – Consultant. Enthera – Consultant. Ferring Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Flagship Pioneering – Consultant, Grant/Research Support, Speakers Bureau. Fresenius Kabi – Consultant, Grant/Research Support, Speakers Bureau. Galapagos NV – Consultant, Grant/Research Support, Speakers Bureau. Genentech – Consultant, Grant/Research Support, Speakers Bureau. Gilde Healthcare – Consultant. Gilead Sciences – Consultant, Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Consultant, Grant/Research Support, Speakers Bureau. Innomar – Consultant. JAMP – Consultant. Johnson & Johnson – Advisor or Review Panel Member, Speakers Bureau. Merck – Consultant, Grant/Research Support, Speakers Bureau. Metacrine – Consultant, Grant/Research Support, Speakers Bureau. Mylan – Consultant, Grant/Research Support, Speakers Bureau. Pandion Therapeutics – Consultant, Grant/Research Support, Speakers Bureau. Pendopharm – Consultant, Grant/Research Support, Speakers Bureau. Pfizer – Consultant, Grant/Research Support, Speakers Bureau. Prometheus Therapeutics and Diagnostics – Consultant, Grant/Research Support, Speakers Bureau. Protagonist Therapeutics – Consultant, Grant/Research Support, Speakers Bureau. Reistone Biopharma – Consultant, Grant/Research Support, Speakers Bureau. Roche – Consultant, Grant/Research Support, Speakers Bureau. Roivant – Consultant. Sandoz – Consultant, Grant/Research Support, Speakers Bureau. Second Genome – Consultant, Grant/Research Support, Speakers Bureau. Shire – Speakers Bureau. Sorriso Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Syndegen – Consultant. Takeda – Consultant, Intellectual Property/Patents, Speakers Bureau. TD Securities – Consultant. Teva – Consultant, Grant/Research Support, Speakers Bureau. Topivert – Consultant, Grant/Research Support, Speakers Bureau. Ventyx Biosciences – Consultant, Grant/Research Support, Speakers Bureau. Vividion Therapeutics – Consultant, Grant/Research Support, Speakers Bureau.
Ronghui Xu indicated no relevant financial relationships.
Siddharth Singh indicated no relevant financial relationships.
Dhruv Ahuja, MBBS1, Soo-Kyung Park, MD, PhD2, Kuan-Hung Yeh, 3, Sagar Patel, BS2, Shane Goodwin, PhD4, Christopher Ma, MD, MPH5, Namrata Singh, MD6, Ashwin Ananthakrishnan, 7, Vipul Jairath, MBChB, DPhil, MRCP8, Ronghui Xu, PhD2, Siddharth Singh, MD, MS2. P5319 - Overall and Comparative Risk of Shingles With Advanced Therapies in Patients with Inflammatory Bowel Diseases, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California San Diego, Delhi, Delhi, India; 2University of California San Diego, San Diego, CA; 3University of California San Diego, La Jolla, CA; 4Western University, London, ON, Canada; 5University of Calgary, Calgary, AB, Canada; 6University of Washington, Seattle, WA; 7Division of Gastroenterology, Massachusetts General Hospital and Harvard Medical School, Boston, MA; 8Department of Medicine and Department of Epidemiology and Biostatistics, Western University, London, ON, Canada
Introduction: We conducted a retrospective cohort study comparing the risk of shingles with advanced therapies in patients with Inflammatory bowel disease (IBD)
Methods: Using an administrative claims database, we identified patients with IBD who initiated treatment with either tumor necrosis factor-α (TNF) antagonists (infliximab, adalimumab, golimumab and certolizumab pegol), anti-integrin agents (vedolizumab), anti-interleukin (IL)-12/23p40 or anti-IL-23p19 agents (ustekinumab, risankizumab, mirikizumab, collectively labeled anti-interleukins), or Janus kinase (JAK) inhibitors (tofacitinib, upadacitinib) between 2016 and 2023, and had insurance coverage for at least 1y before and after treatment initiation. We assessed the incidence rate (IR per 100 person-year [PY]) of shingles (overall and complicated, including post herpetic neuralgia ocular and neurologic involvement) and compared risks using inverse probability of treatment weighting (IPTW). Propensity scores were estimated through generalized boosted models incorporating demographics, comorbidities, healthcare utilization, and prior/concomitant IBD therapies. Weighted Cox models estimated hazard ratios (HR) and 95% confidence intervals (CI).
Results: We included 21,564 patients with IBD (mean age range, 45-49 years; 51-53% females; 6% with zoster vaccination) followed over 27 months. The incidence of shingles and complicated shingles varied with difference advanced therapies: TNF antagonists (n=9,385; IR of shingles/complicated shingles per 100-py, 1.00/0.30), anti-integrin agents (n=5,881; IR, 1.38/0.43), anti-interleukins (n=5,445; IR, 1.24/0.45) and JAK inhibitors (n=853; IR, 3.33/0.88). After adjusting for confounding variables using IPTW, JAK inhibitors were associated with higher risks of shingles compared with TNF antagonists (HR, 2.72 [95% CI, 1.67-4.43]), anti-integrin agents (HR, 2.41 [1.51-3.84]) and anti-IL 12/23p40 agents or anti-IL-23p19 (HR, 2.45 [1.53-3.95]). Similar trends were observed for risk of complicated shingles. No differences were observed in the risk of shingles between TNF antagonists, anti-integrins and anti-interleukins (Figure 1).
Discussion: In this large real-world cohort of patients with IBD, JAK inhibitors were associated with higher risks of overall shingles compared to other advanced therapies. No differences were observed in the risk of shingles with other advanced therapies, with overall incidence ranging from 1.0-1.4 per 100-py.
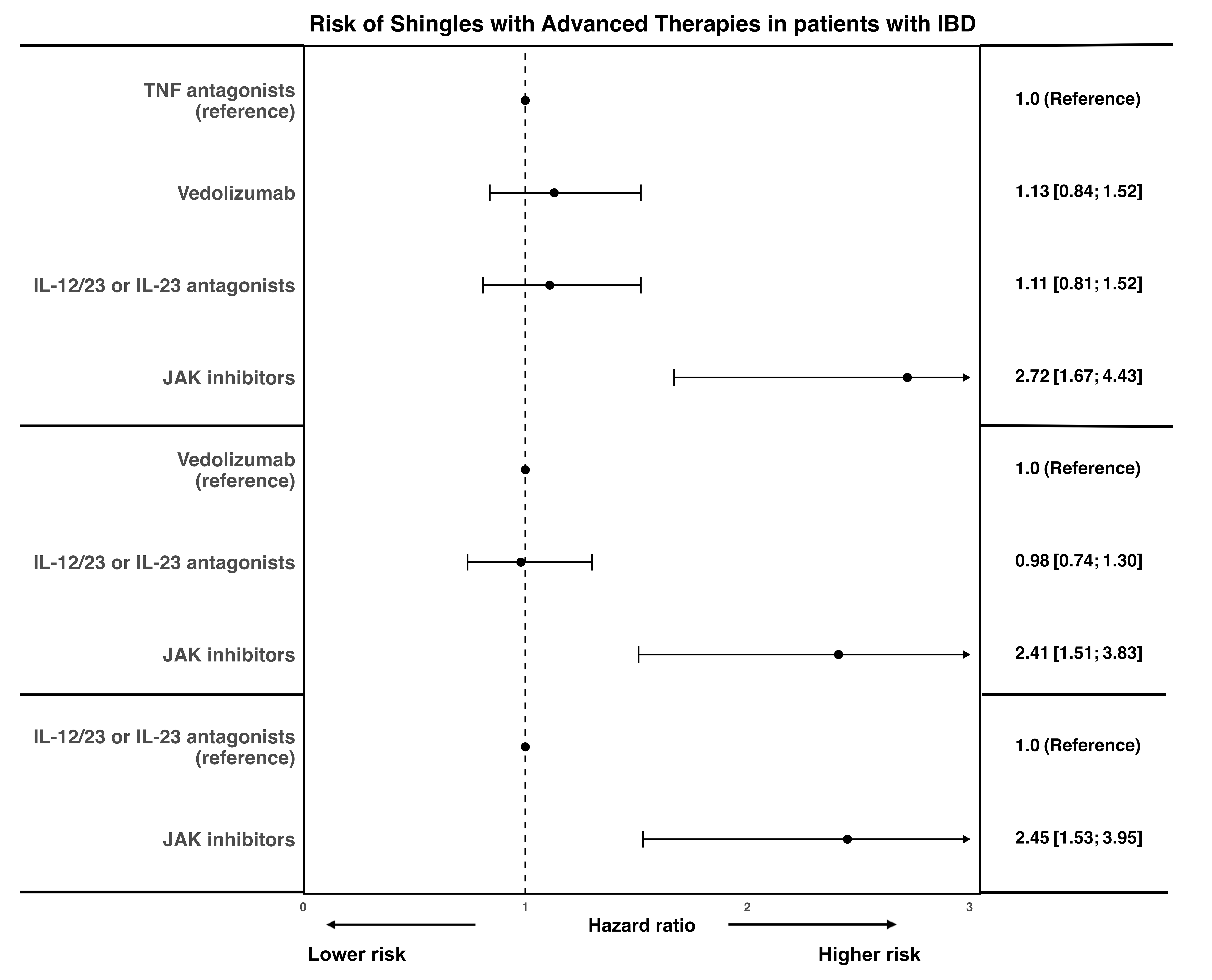
Figure: Figure 1. Comparative risk of shingles with advanced therapies in patients with IBD
Disclosures:
Dhruv Ahuja indicated no relevant financial relationships.
Soo-Kyung Park indicated no relevant financial relationships.
Kuan-Hung Yeh indicated no relevant financial relationships.
Sagar Patel indicated no relevant financial relationships.
Shane Goodwin indicated no relevant financial relationships.
Christopher Ma: Abbvie – Consultant, Grant/Research Support, speaker's fee. Alimentiv – Consultant, speaker's fee. Amgen – Consultant, speaker's fee. AVIR Pharma Inc. – Consultant, speaker's fee. Bristol Myers Squibb – Consultant, speaker's fee. Celltrion – Consultant. Eli Lilly – Consultant, Grant/Research Support, speaker's fee. Ferring – Consultant, Grant/Research Support, speaker's fee. Forte Biosciences – Consultant. Fresenius Kabi – Consultant, speaker's fee. Gilead – Consultant. Janssen – Consultant, speaker's fee. McKesson – Consultant. Merck – Speaker's fee. Mirador Therapeutics – Consultant. Mylan – Consultant. Organon – speaker's fee. Pendopharm – Consultant, speaker's fee. Pfizer – Consultant, Grant/Research Support, speaker's fee. Prometheus Biosciences Inc. – Consultant. Roche – Consultant. Sanofi – Consultant, speaker's fee. Springer Publishing – Royalties. Takeda – Consultant, speaker's fee. Tillotts Pharma – Consultant, speaker's fee.
Namrata Singh indicated no relevant financial relationships.
Ashwin Ananthakrishnan: Takeda – Grant/Research Support.
Vipul Jairath: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. Alimentiv – Consultant, Grant/Research Support. Arena Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Asahi Kasei Pharma – Consultant, Grant/Research Support, Speakers Bureau. Asieris Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. AstraZeneca – Consultant, Grant/Research Support, Speakers Bureau. Avoro Capital – Consultant. Bristol Myers Squibb – Consultant, Grant/Research Support, Speakers Bureau. Celltrion – Consultant, Grant/Research Support, Speakers Bureau. Eli Lilly and Company – Consultant, Grant/Research Support, Speakers Bureau. Endpoint Health – Consultant. Enthera – Consultant. Ferring Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Flagship Pioneering – Consultant, Grant/Research Support, Speakers Bureau. Fresenius Kabi – Consultant, Grant/Research Support, Speakers Bureau. Galapagos NV – Consultant, Grant/Research Support, Speakers Bureau. Genentech – Consultant, Grant/Research Support, Speakers Bureau. Gilde Healthcare – Consultant. Gilead Sciences – Consultant, Grant/Research Support, Speakers Bureau. GlaxoSmithKline – Consultant, Grant/Research Support, Speakers Bureau. Innomar – Consultant. JAMP – Consultant. Johnson & Johnson – Advisor or Review Panel Member, Speakers Bureau. Merck – Consultant, Grant/Research Support, Speakers Bureau. Metacrine – Consultant, Grant/Research Support, Speakers Bureau. Mylan – Consultant, Grant/Research Support, Speakers Bureau. Pandion Therapeutics – Consultant, Grant/Research Support, Speakers Bureau. Pendopharm – Consultant, Grant/Research Support, Speakers Bureau. Pfizer – Consultant, Grant/Research Support, Speakers Bureau. Prometheus Therapeutics and Diagnostics – Consultant, Grant/Research Support, Speakers Bureau. Protagonist Therapeutics – Consultant, Grant/Research Support, Speakers Bureau. Reistone Biopharma – Consultant, Grant/Research Support, Speakers Bureau. Roche – Consultant, Grant/Research Support, Speakers Bureau. Roivant – Consultant. Sandoz – Consultant, Grant/Research Support, Speakers Bureau. Second Genome – Consultant, Grant/Research Support, Speakers Bureau. Shire – Speakers Bureau. Sorriso Pharmaceuticals – Consultant, Grant/Research Support, Speakers Bureau. Syndegen – Consultant. Takeda – Consultant, Intellectual Property/Patents, Speakers Bureau. TD Securities – Consultant. Teva – Consultant, Grant/Research Support, Speakers Bureau. Topivert – Consultant, Grant/Research Support, Speakers Bureau. Ventyx Biosciences – Consultant, Grant/Research Support, Speakers Bureau. Vividion Therapeutics – Consultant, Grant/Research Support, Speakers Bureau.
Ronghui Xu indicated no relevant financial relationships.
Siddharth Singh indicated no relevant financial relationships.
Dhruv Ahuja, MBBS1, Soo-Kyung Park, MD, PhD2, Kuan-Hung Yeh, 3, Sagar Patel, BS2, Shane Goodwin, PhD4, Christopher Ma, MD, MPH5, Namrata Singh, MD6, Ashwin Ananthakrishnan, 7, Vipul Jairath, MBChB, DPhil, MRCP8, Ronghui Xu, PhD2, Siddharth Singh, MD, MS2. P5319 - Overall and Comparative Risk of Shingles With Advanced Therapies in Patients with Inflammatory Bowel Diseases, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
