Tuesday Poster Session
Category: IBD
P5318 - Comparative Risk of Pulmonary Complications in Ulcerative Colitis vs Crohn’s Disease: A Nationwide Propensity-Matched Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohammad AbuAssi, MD (he/him/his)
University of Central Florida, HCA Healthcare GME
Gainesville, FL
Presenting Author(s)
Mohammad Abuassi, MD1, Hadi Khaled. Abou Zeid, MD2, Kinan Obeidat, MD3, Mahmoud Y. Madi, MD4
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Mayo Clinic, Rochester, MN; 3University of Texas Medical Branch, Santa Fe, TX; 4University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Inflammatory bowel disease (IBD) is known to involve extraintestinal manifestations, including pulmonary complications. However, comparative data delineating differences in pulmonary risks between ulcerative colitis (UC) and Crohn’s disease (CD) remain scarce.
Methods: A retrospective cohort study was performed utilizing the TriNetX Network, a de-identified electronic health records from 65 healthcare organizations. After 1:1 propensity score matching for age, sex, race, ethnicity, and non-pulmonary comorbidities, over 260,000 UC and CD patients were included with balanced baseline characteristics. Patients with overlapping diagnoses were excluded. Outcomes analyzed included asthma, COPD, bronchiectasis, emphysema, chronic sinusitis, atelectasis, acute and chronic respiratory failure, pleural effusion, pneumothorax, and all-cause mortality. Risk differences, risk ratios, and odds ratios were computed with 95% confidence intervals (CIs), and significance assessed via z-tests.
Results: Patients with UC had significantly lower risks for COPD (5.9% vs. 6.9%, OR 0.85, 95% CI 0.83–0.87), emphysema (2.5% vs. 2.8%, OR 0.89, 95% CI 0.86–0.92), and asthma (9.8% vs. 10.2%, OR 0.96, 95% CI 0.94–0.97) compared to those with CD. These differences remained statistically significant following adjustment for demographic and clinical covariates. Conversely, UC was associated with higher odds of bronchiectasis (0.9% vs. 0.8%, OR 1.11, 95% CI 1.05–1.18), atelectasis (5.1% vs. 4.8%, OR 1.07, 95% CI 1.04–1.09), pleural effusion (4.5% vs. 3.9%, OR 1.16, 95% CI 1.13–1.19), and chronic respiratory failure (1.3% vs. 1.1%, OR 1.11, 95% CI 1.06–1.17). Acute respiratory failure was also slightly more common in UC (4.9% vs. 4.6%, OR 1.05, 95% CI 1.03–1.08). No significant difference was observed in pneumothorax rates. Mortality was notably lower in UC (1.9% vs. 2.9%, OR 0.67, 95% CI 0.64–0.69).
Discussion: In this large-scale matched cohort, pulmonary complications differed by IBD subtype. UC demonstrated a lower likelihood of COPD, emphysema, and all-cause mortality relative to CD. However, patients with UC exhibited a greater risk of bronchiectasis, pleural effusion, and atelectasis. Our findings highlight the necessity for tailored pulmonary monitoring in patients with IBD, with distinct considerations for UC and CD subtypes. Future research should explore mechanistic pathways underlying these observed differences to enhance targeted interventions.
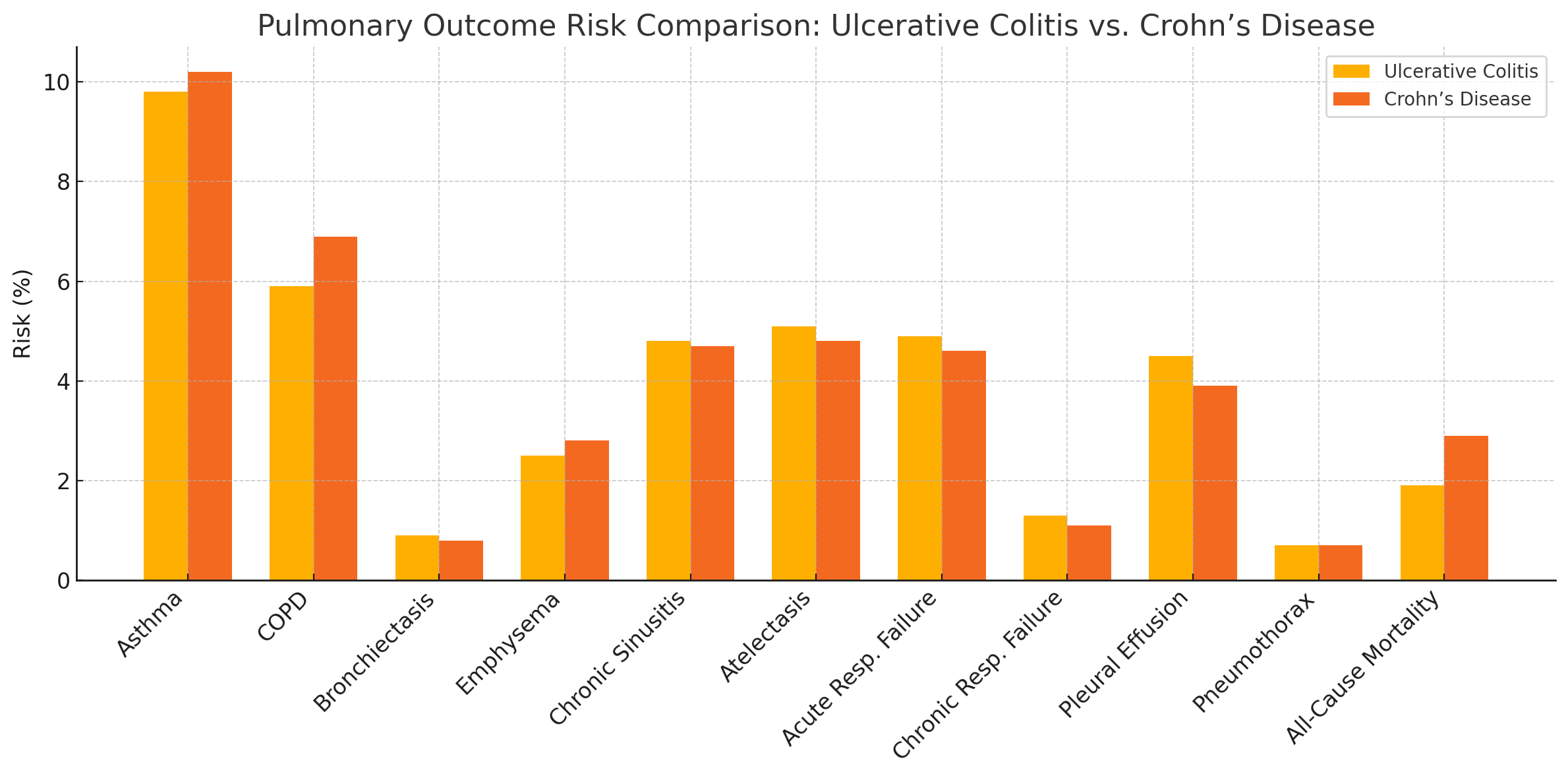
Figure: Forest plot displaying adjusted odds ratios (ORs) with 95% confidence intervals comparing the risk of pulmonary complications in ulcerative colitis (UC) versus Crohn’s disease (CD).
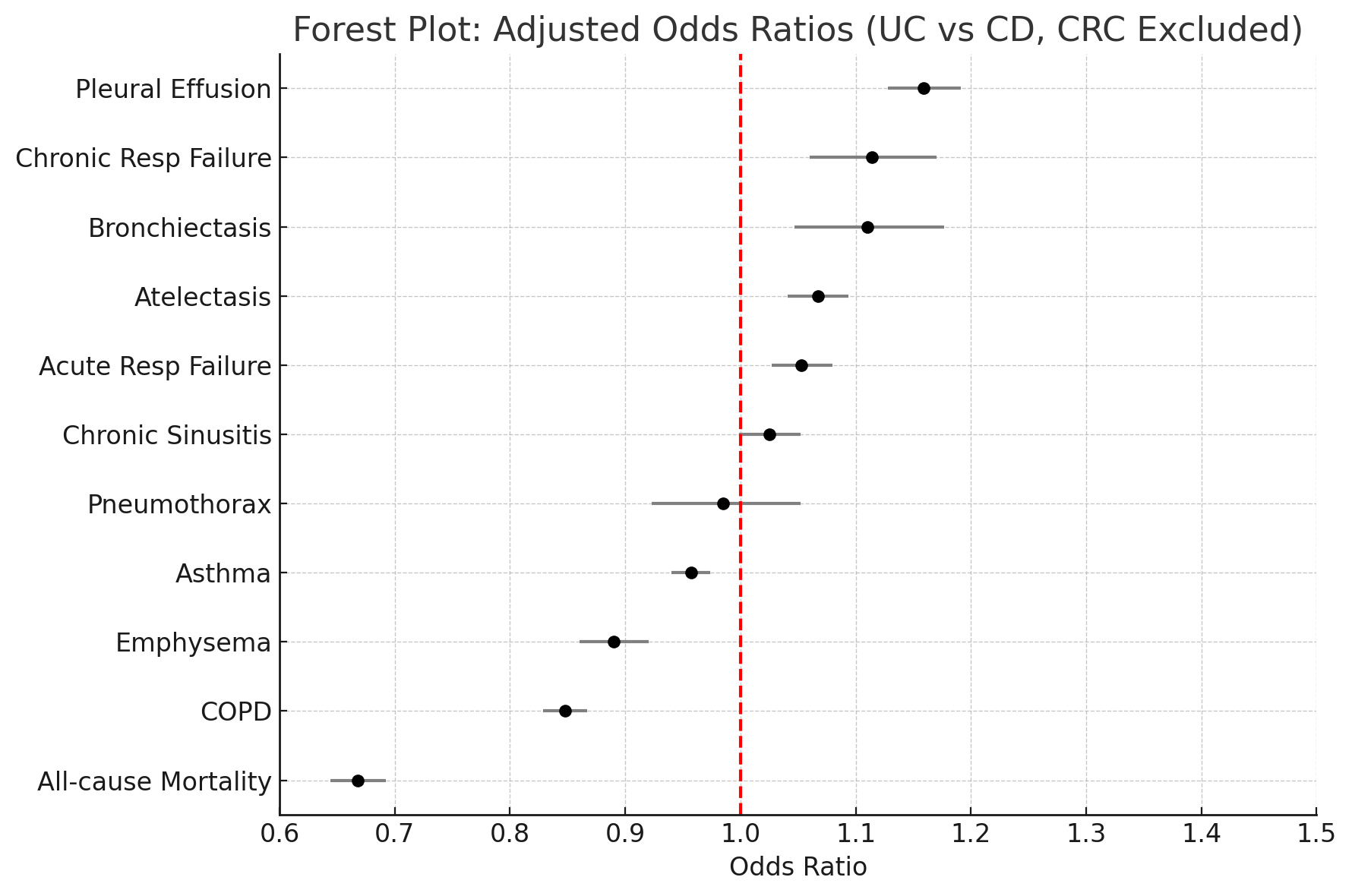
Figure: Bar graph comparing absolute risk (%) of pulmonary outcomes between patients with ulcerative colitis (yellow) and Crohn’s disease (orange).
Disclosures:
Mohammad Abuassi indicated no relevant financial relationships.
Hadi Abou Zeid indicated no relevant financial relationships.
Kinan Obeidat indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Mohammad Abuassi, MD1, Hadi Khaled. Abou Zeid, MD2, Kinan Obeidat, MD3, Mahmoud Y. Madi, MD4. P5318 - Comparative Risk of Pulmonary Complications in Ulcerative Colitis vs Crohn’s Disease: A Nationwide Propensity-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Mayo Clinic, Rochester, MN; 3University of Texas Medical Branch, Santa Fe, TX; 4University of Texas at Austin Dell Medical School, Austin, TX
Introduction: Inflammatory bowel disease (IBD) is known to involve extraintestinal manifestations, including pulmonary complications. However, comparative data delineating differences in pulmonary risks between ulcerative colitis (UC) and Crohn’s disease (CD) remain scarce.
Methods: A retrospective cohort study was performed utilizing the TriNetX Network, a de-identified electronic health records from 65 healthcare organizations. After 1:1 propensity score matching for age, sex, race, ethnicity, and non-pulmonary comorbidities, over 260,000 UC and CD patients were included with balanced baseline characteristics. Patients with overlapping diagnoses were excluded. Outcomes analyzed included asthma, COPD, bronchiectasis, emphysema, chronic sinusitis, atelectasis, acute and chronic respiratory failure, pleural effusion, pneumothorax, and all-cause mortality. Risk differences, risk ratios, and odds ratios were computed with 95% confidence intervals (CIs), and significance assessed via z-tests.
Results: Patients with UC had significantly lower risks for COPD (5.9% vs. 6.9%, OR 0.85, 95% CI 0.83–0.87), emphysema (2.5% vs. 2.8%, OR 0.89, 95% CI 0.86–0.92), and asthma (9.8% vs. 10.2%, OR 0.96, 95% CI 0.94–0.97) compared to those with CD. These differences remained statistically significant following adjustment for demographic and clinical covariates. Conversely, UC was associated with higher odds of bronchiectasis (0.9% vs. 0.8%, OR 1.11, 95% CI 1.05–1.18), atelectasis (5.1% vs. 4.8%, OR 1.07, 95% CI 1.04–1.09), pleural effusion (4.5% vs. 3.9%, OR 1.16, 95% CI 1.13–1.19), and chronic respiratory failure (1.3% vs. 1.1%, OR 1.11, 95% CI 1.06–1.17). Acute respiratory failure was also slightly more common in UC (4.9% vs. 4.6%, OR 1.05, 95% CI 1.03–1.08). No significant difference was observed in pneumothorax rates. Mortality was notably lower in UC (1.9% vs. 2.9%, OR 0.67, 95% CI 0.64–0.69).
Discussion: In this large-scale matched cohort, pulmonary complications differed by IBD subtype. UC demonstrated a lower likelihood of COPD, emphysema, and all-cause mortality relative to CD. However, patients with UC exhibited a greater risk of bronchiectasis, pleural effusion, and atelectasis. Our findings highlight the necessity for tailored pulmonary monitoring in patients with IBD, with distinct considerations for UC and CD subtypes. Future research should explore mechanistic pathways underlying these observed differences to enhance targeted interventions.
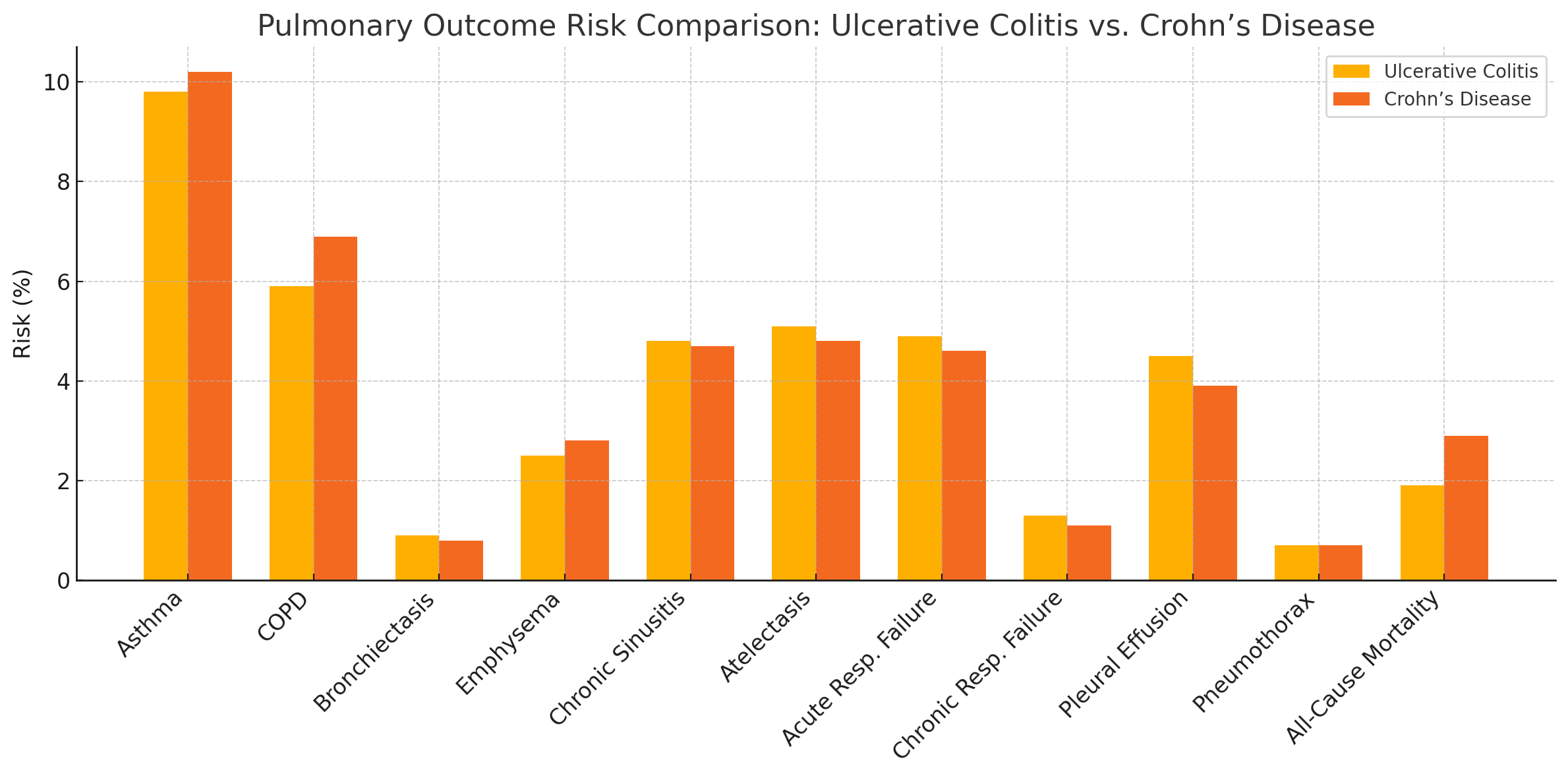
Figure: Forest plot displaying adjusted odds ratios (ORs) with 95% confidence intervals comparing the risk of pulmonary complications in ulcerative colitis (UC) versus Crohn’s disease (CD).
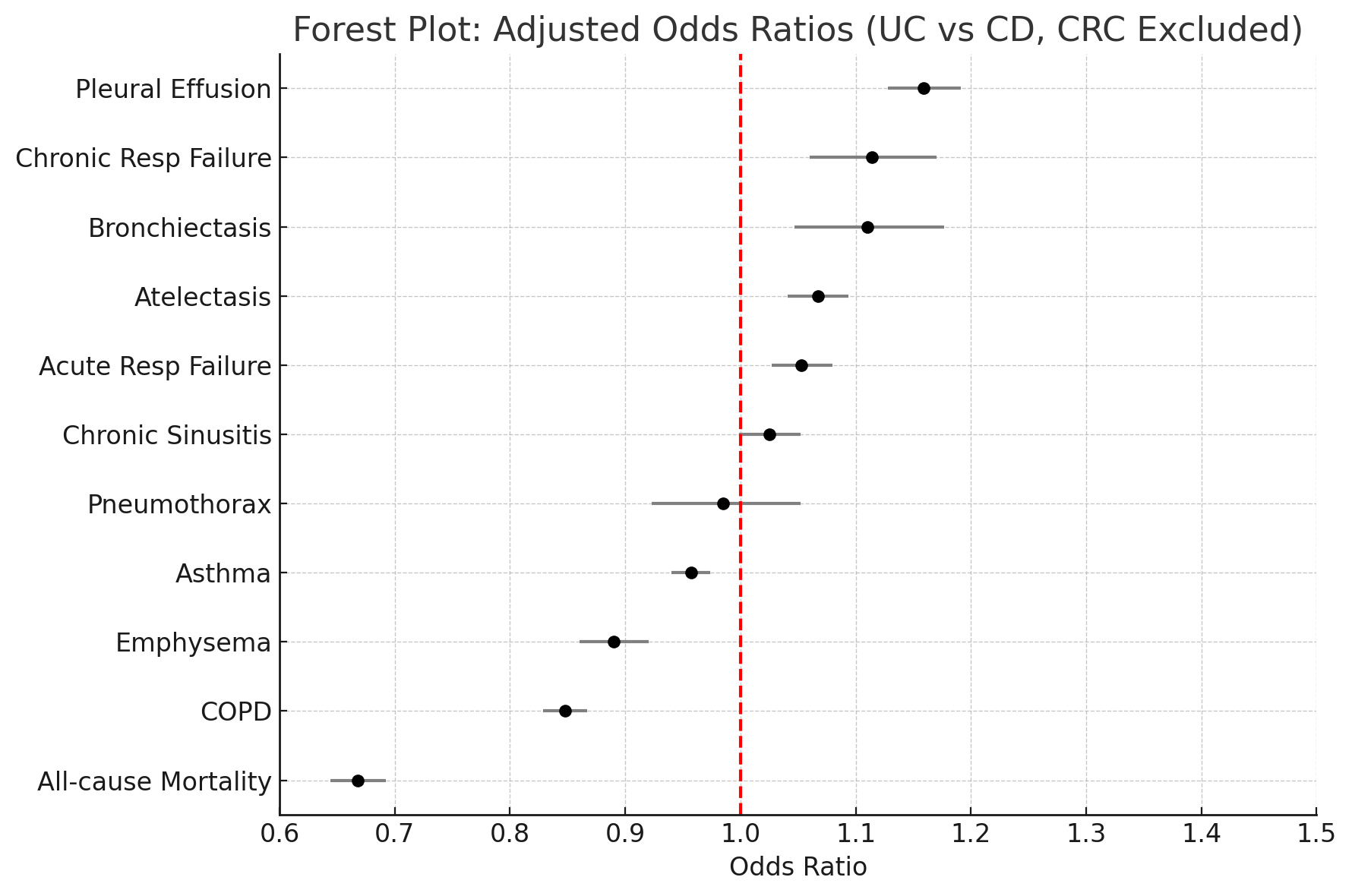
Figure: Bar graph comparing absolute risk (%) of pulmonary outcomes between patients with ulcerative colitis (yellow) and Crohn’s disease (orange).
Disclosures:
Mohammad Abuassi indicated no relevant financial relationships.
Hadi Abou Zeid indicated no relevant financial relationships.
Kinan Obeidat indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Mohammad Abuassi, MD1, Hadi Khaled. Abou Zeid, MD2, Kinan Obeidat, MD3, Mahmoud Y. Madi, MD4. P5318 - Comparative Risk of Pulmonary Complications in Ulcerative Colitis vs Crohn’s Disease: A Nationwide Propensity-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
