Tuesday Poster Session
Category: IBD
P5311 - Rates of Thromboprophylaxis and Venous Thromboembolism in Hospitalized Inflammatory Bowel Disease Patients
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DB
Dhanushya Battepati, MD
Baylor Scott & White Medical Center
Temple, TX
Presenting Author(s)
Dhanushya Battepati, MD1, Gautham Budaraju, ME2, Jordan Young, DO1, Matthew Garrett, MD1, David Alvarez, BBA2, Laith Wahab, DO1, Christopher Johnson, MD, PhD1
1Baylor Scott & White Medical Center, Temple, TX; 2Baylor College of Medicine, Temple, TX
Introduction: Ulcerative colitis (UC) or Crohn's Disease (CD) are at increased risk for venous thromboembolism (VTE) during hospital admission. The objective of our study is to assess rates of VTE events in patients admitted for a UC or CD flare. We aim to focus on rates of initiation of DVT prophylaxis among the admitted patients and correlating the data to see if these patients develop a VTE event within 30 days, 6 months or 12 months of the initial hospital admission.
Methods: This is a single-center retrospective cohort chart review of patients greater than 18 years of age admitted from 1/1/2014 to 12/31/2023 for a UC or CD flare who had an admission for a VTE event within a year from the initial admission. This study was approved by the IRB.
Results: A total of 387 met criteria for our study, with n= 238 being CD patients. Among the CD cohort, 5.46% of patients (n=13) developed a VTE event after their initial admission, while the UC cohort had 4.7% (n =7). 61.8% of CD patients were initiated on DVT prophylaxis, while only 45.6% of UC patients were given DVT prophylaxis during their initial admission for IBD. A Fisher's exact test between the rates of DVT prophylaxis among CD vs. UC patients was determined to be statistically significant (P = 0.0023).
Discussion: Our study showed that there is a statistically significant decrease in rates of DVT prophylaxis initiation in patients admitted for a UC flare, compared to their CD counterparts. There is no statistically significant difference between the rates of VTE among the CD and UC cohort, although numerically there were more CD patients who developed a VTE. It is imperative that these patients are promptly initiated on DVT prophylaxis upon admission to the hospital. Our institution is in the process of implementing a protocol to ensure that best practices are being followed for IBD patients who are admitted to the hospital, to further prevent VTE events as well as IBD related readmissions to the hospital.
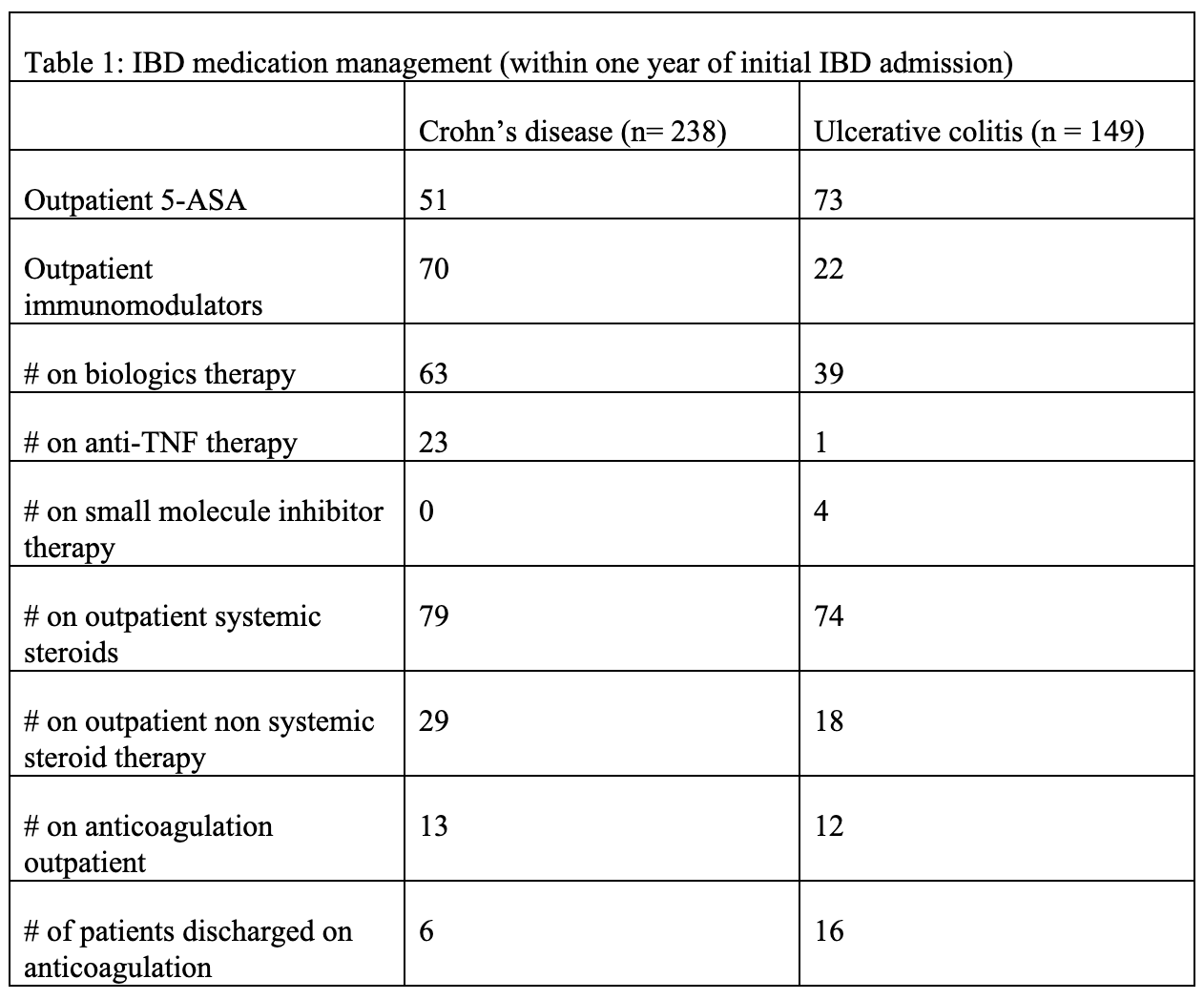
Figure: Table 1 describes the medications our cohort of patients were treated with.
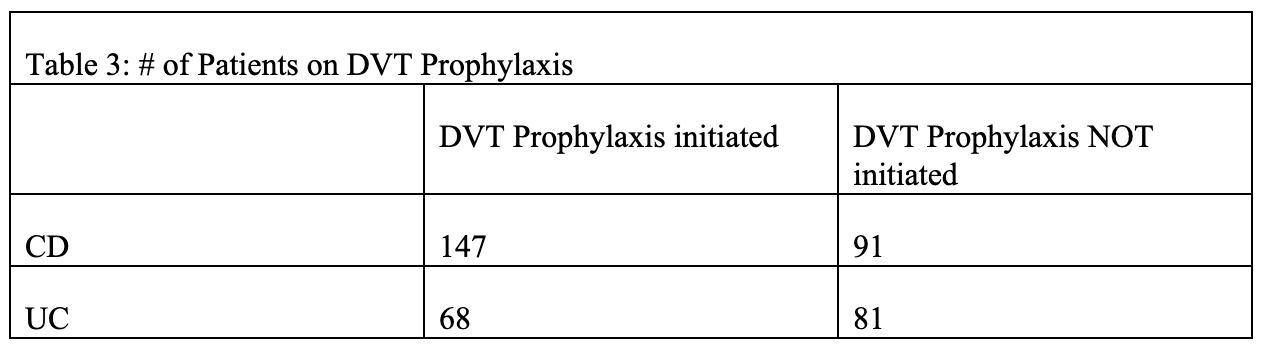
Figure: This table describes the rates of initiation of DVT prophylaxis between CD and UC patients in the study's cohort.
Disclosures:
Dhanushya Battepati indicated no relevant financial relationships.
Gautham Budaraju indicated no relevant financial relationships.
Jordan Young indicated no relevant financial relationships.
Matthew Garrett indicated no relevant financial relationships.
David Alvarez indicated no relevant financial relationships.
Laith Wahab indicated no relevant financial relationships.
Christopher Johnson indicated no relevant financial relationships.
Dhanushya Battepati, MD1, Gautham Budaraju, ME2, Jordan Young, DO1, Matthew Garrett, MD1, David Alvarez, BBA2, Laith Wahab, DO1, Christopher Johnson, MD, PhD1. P5311 - Rates of Thromboprophylaxis and Venous Thromboembolism in Hospitalized Inflammatory Bowel Disease Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Baylor Scott & White Medical Center, Temple, TX; 2Baylor College of Medicine, Temple, TX
Introduction: Ulcerative colitis (UC) or Crohn's Disease (CD) are at increased risk for venous thromboembolism (VTE) during hospital admission. The objective of our study is to assess rates of VTE events in patients admitted for a UC or CD flare. We aim to focus on rates of initiation of DVT prophylaxis among the admitted patients and correlating the data to see if these patients develop a VTE event within 30 days, 6 months or 12 months of the initial hospital admission.
Methods: This is a single-center retrospective cohort chart review of patients greater than 18 years of age admitted from 1/1/2014 to 12/31/2023 for a UC or CD flare who had an admission for a VTE event within a year from the initial admission. This study was approved by the IRB.
Results: A total of 387 met criteria for our study, with n= 238 being CD patients. Among the CD cohort, 5.46% of patients (n=13) developed a VTE event after their initial admission, while the UC cohort had 4.7% (n =7). 61.8% of CD patients were initiated on DVT prophylaxis, while only 45.6% of UC patients were given DVT prophylaxis during their initial admission for IBD. A Fisher's exact test between the rates of DVT prophylaxis among CD vs. UC patients was determined to be statistically significant (P = 0.0023).
Discussion: Our study showed that there is a statistically significant decrease in rates of DVT prophylaxis initiation in patients admitted for a UC flare, compared to their CD counterparts. There is no statistically significant difference between the rates of VTE among the CD and UC cohort, although numerically there were more CD patients who developed a VTE. It is imperative that these patients are promptly initiated on DVT prophylaxis upon admission to the hospital. Our institution is in the process of implementing a protocol to ensure that best practices are being followed for IBD patients who are admitted to the hospital, to further prevent VTE events as well as IBD related readmissions to the hospital.
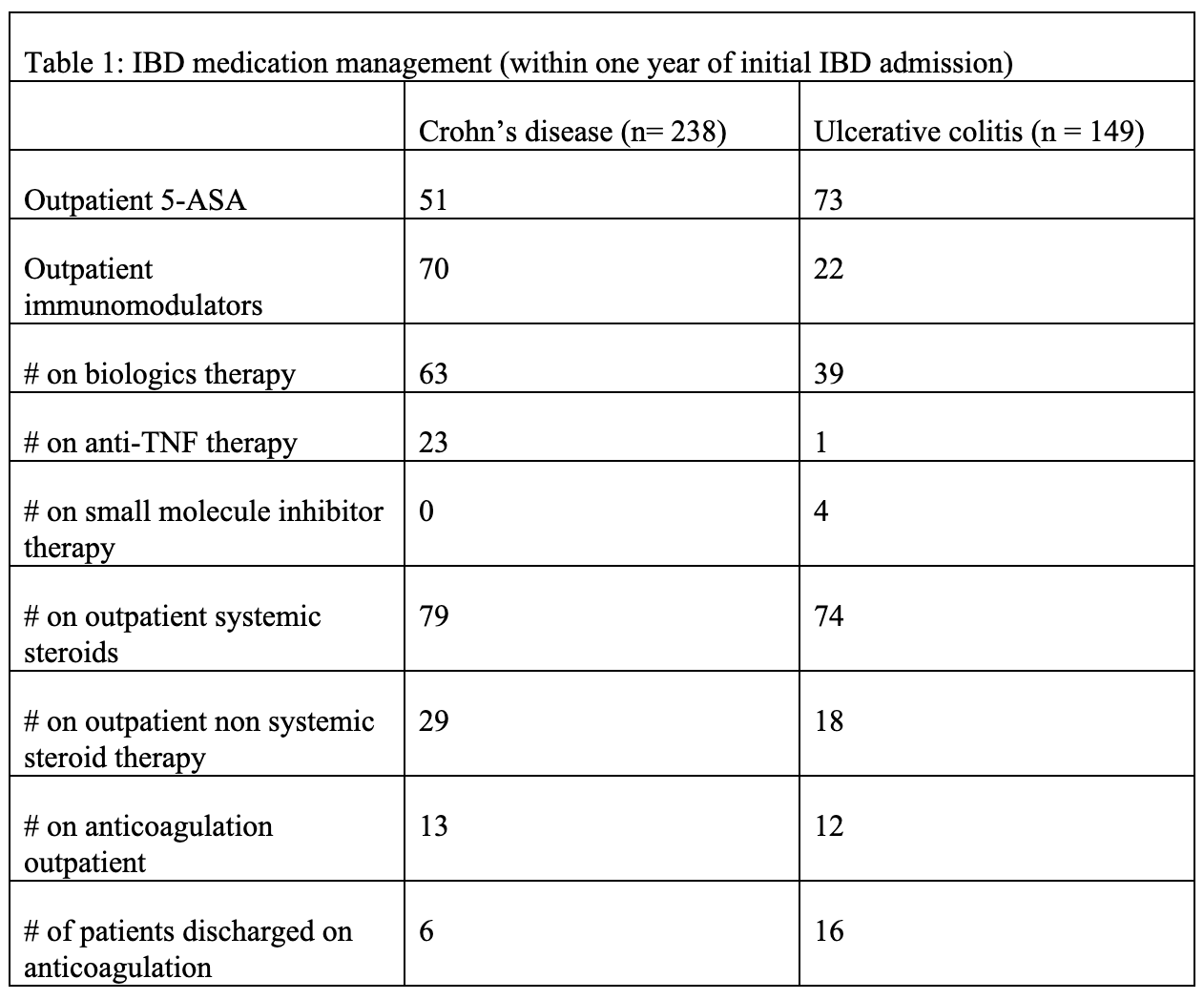
Figure: Table 1 describes the medications our cohort of patients were treated with.
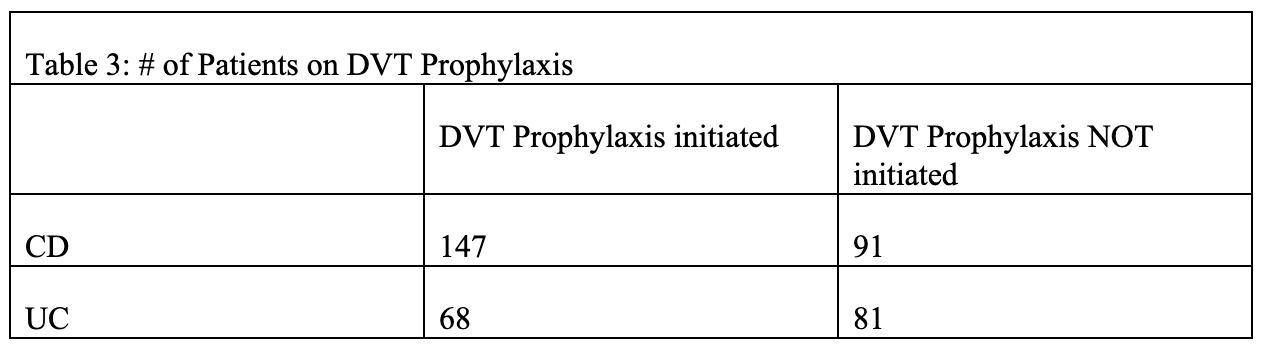
Figure: This table describes the rates of initiation of DVT prophylaxis between CD and UC patients in the study's cohort.
Disclosures:
Dhanushya Battepati indicated no relevant financial relationships.
Gautham Budaraju indicated no relevant financial relationships.
Jordan Young indicated no relevant financial relationships.
Matthew Garrett indicated no relevant financial relationships.
David Alvarez indicated no relevant financial relationships.
Laith Wahab indicated no relevant financial relationships.
Christopher Johnson indicated no relevant financial relationships.
Dhanushya Battepati, MD1, Gautham Budaraju, ME2, Jordan Young, DO1, Matthew Garrett, MD1, David Alvarez, BBA2, Laith Wahab, DO1, Christopher Johnson, MD, PhD1. P5311 - Rates of Thromboprophylaxis and Venous Thromboembolism in Hospitalized Inflammatory Bowel Disease Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
