Tuesday Poster Session
Category: IBD
P5305 - Crohn’s Disease With Comorbid Generalized Anxiety Disorder: A Retrospective Analysis of Inpatient Outcomes in a National Cohort
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MA
Madia Ahad, MD
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Anwar Uddin, MD, Madia Ahad, MD, Rafat Uddin, MS, Xavier Aguayoarguello, MD, Savanna Thor, DO, MPH
SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Crohn’s disease (CD) is a chronic inflammatory bowel disease often associated with psychiatric conditions, including generalized anxiety disorder (GAD). GAD is highly prevalent among patients with chronic illness and may influence inflammatory activity, treatment adherence, and hospitalization outcomes. However, its impact on inpatient outcomes among patients with CD remains insufficiently explored. This study aimed to evaluate clinical outcomes in hospitalized adults with CD, comparing those with and without comorbid GAD.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample (2016–2020). Adults (≥18 years) with Crohn’s disease (ICD-10 K50.xx) listed among the first ten discharge diagnoses were included. Comorbid GAD was identified by ICD-10 code F41.1. Outcomes included inpatient mortality, length of stay (LOS), total hospital cost, sepsis, electrolyte abnormalities, malnutrition, intestinal abscess, colonic perforation, and depression. Multivariable logistic regression adjusted for age, sex, race, and Charlson Comorbidity Index. Hospital costs were modeled with gamma regression (log-link) and adjusted to 2020 U.S. dollars using the Consumer Price Index.
Results: Among 856,395 hospitalized patients with CD, 18,115 (2.1 percent) had comorbid GAD. Among hospitalized CD patients, those with comorbid GAD had significantly lower in-hospital mortality (0.2% vs. 1.0%; OR 0.26, 95% CI: 0.13–0.52) and lower rates of sepsis (6.5% vs. 8.6%; OR 0.77, 95% CI: 0.67–0.88) compared to those without GAD. This lower mortality may be partly explained by increased healthcare utilization and patient hypervigilance, potentially leading to evaluation at an earlier stage of disease. However, GAD was associated with longer LOS (5.4 vs. 4.9 days; OR 1.13, 95% CI: 1.09–1.17) and a markedly higher prevalence of comorbid depression (27% vs. 14%; OR 2.01, 95% CI: 1.85–2.18). No significant differences were observed in hospital costs, electrolyte derangements, malnutrition, intestinal abscess, or colonic perforation between the groups.
Discussion: Hospitalized patients with Crohn’s disease and comorbid GAD had lower inpatient mortality and reduced odds of sepsis, despite longer hospital stays and higher rates of depression. No significant differences were seen in hospital cost, malnutrition, or procedural complications. Further study is needed to examine the potential relationship between psychiatric comorbidities and inflammatory disease outcomes in this population.
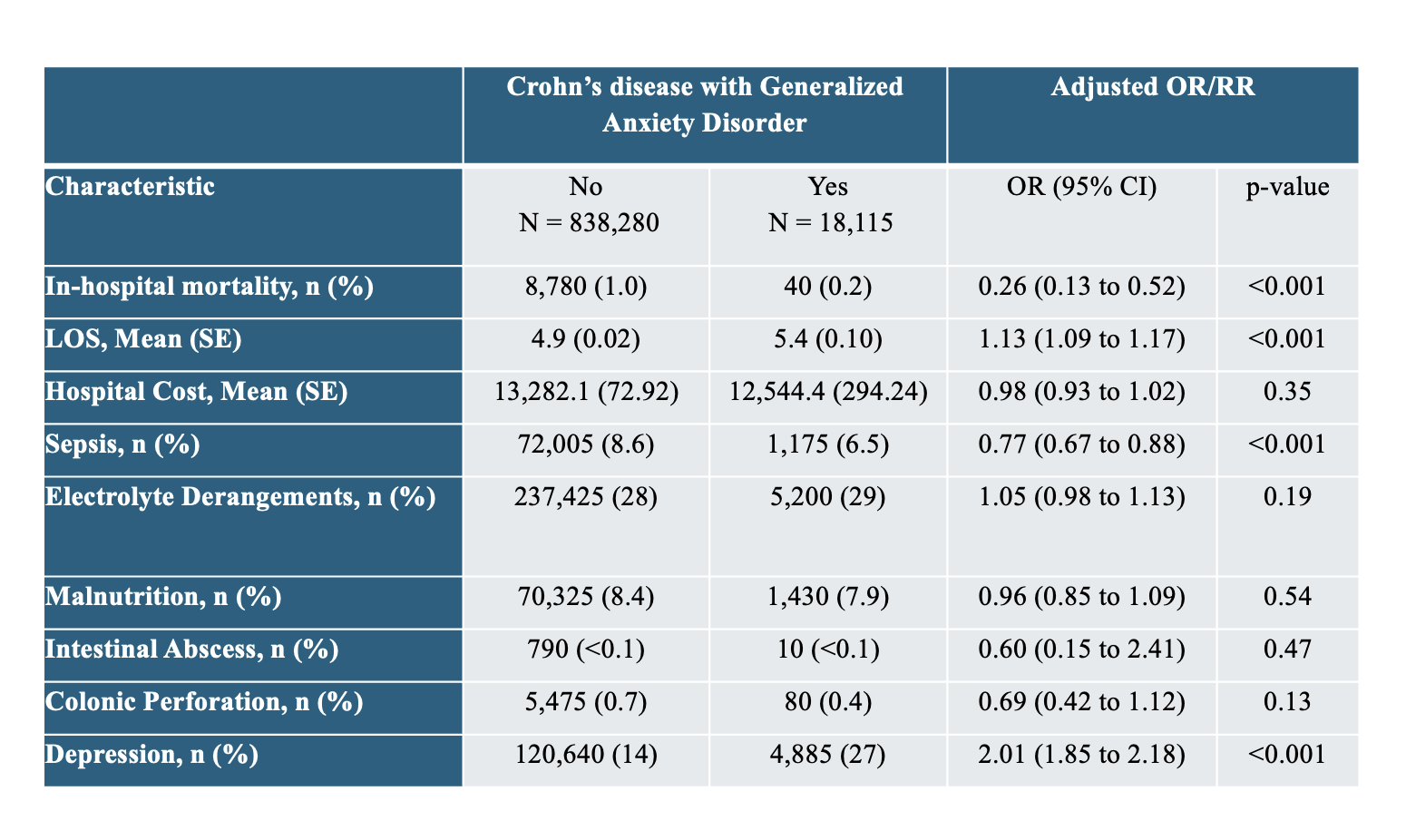
Figure: Table 1: Comparison of in-hospital outcomes among hospitalized patients with Crohn's disease by comorbid generalized anxiety disorder
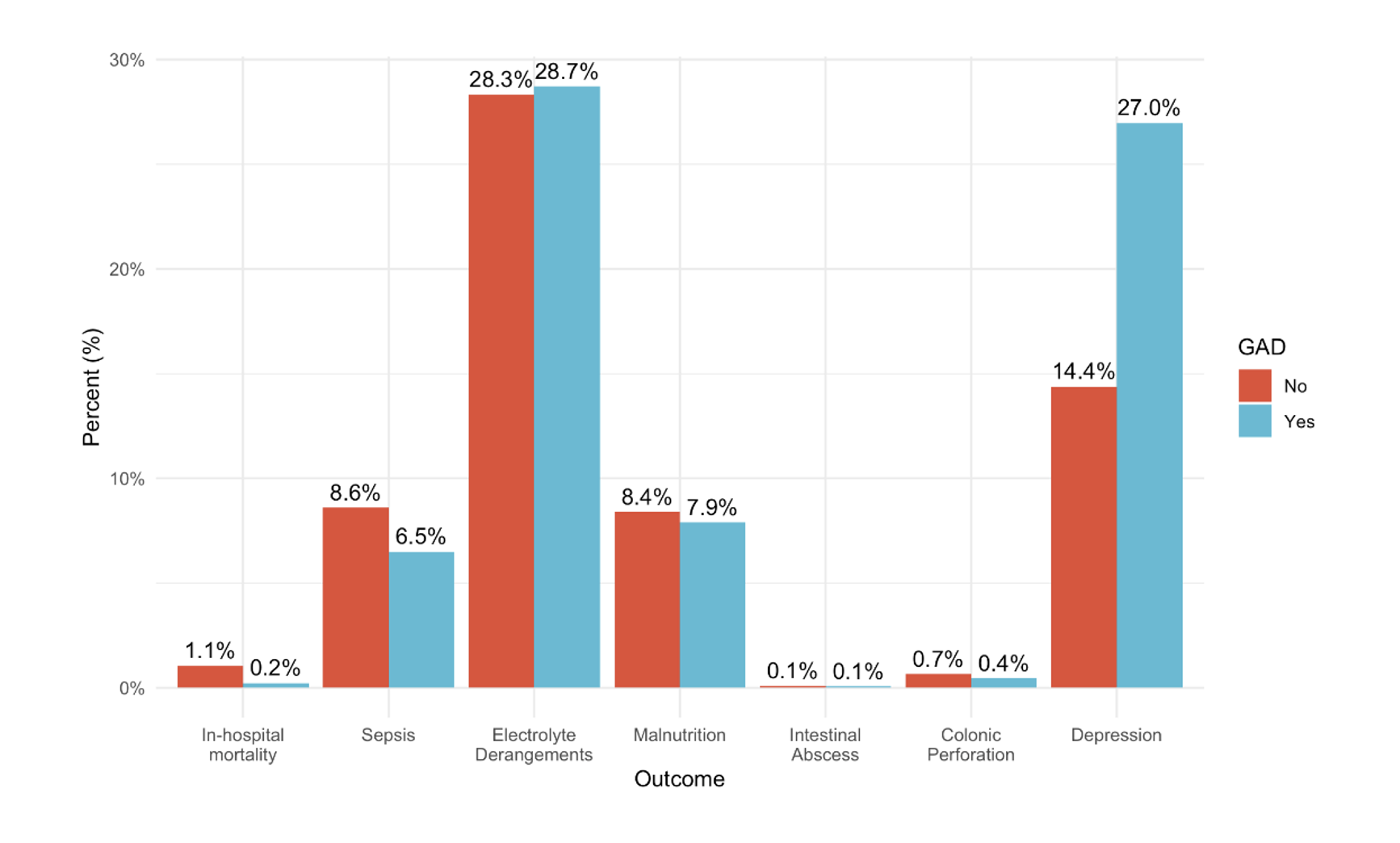
Figure: Figure 1: Bar Chart of in-hospital outcomes among hospitalized patients with Crohn's disease by comorbid generalized anxiety disorder
Disclosures:
Anwar Uddin indicated no relevant financial relationships.
Madia Ahad indicated no relevant financial relationships.
Rafat Uddin indicated no relevant financial relationships.
Xavier Aguayoarguello indicated no relevant financial relationships.
Savanna Thor indicated no relevant financial relationships.
Anwar Uddin, MD, Madia Ahad, MD, Rafat Uddin, MS, Xavier Aguayoarguello, MD, Savanna Thor, DO, MPH. P5305 - Crohn’s Disease With Comorbid Generalized Anxiety Disorder: A Retrospective Analysis of Inpatient Outcomes in a National Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Crohn’s disease (CD) is a chronic inflammatory bowel disease often associated with psychiatric conditions, including generalized anxiety disorder (GAD). GAD is highly prevalent among patients with chronic illness and may influence inflammatory activity, treatment adherence, and hospitalization outcomes. However, its impact on inpatient outcomes among patients with CD remains insufficiently explored. This study aimed to evaluate clinical outcomes in hospitalized adults with CD, comparing those with and without comorbid GAD.
Methods: We conducted a retrospective cohort study using the National Inpatient Sample (2016–2020). Adults (≥18 years) with Crohn’s disease (ICD-10 K50.xx) listed among the first ten discharge diagnoses were included. Comorbid GAD was identified by ICD-10 code F41.1. Outcomes included inpatient mortality, length of stay (LOS), total hospital cost, sepsis, electrolyte abnormalities, malnutrition, intestinal abscess, colonic perforation, and depression. Multivariable logistic regression adjusted for age, sex, race, and Charlson Comorbidity Index. Hospital costs were modeled with gamma regression (log-link) and adjusted to 2020 U.S. dollars using the Consumer Price Index.
Results: Among 856,395 hospitalized patients with CD, 18,115 (2.1 percent) had comorbid GAD. Among hospitalized CD patients, those with comorbid GAD had significantly lower in-hospital mortality (0.2% vs. 1.0%; OR 0.26, 95% CI: 0.13–0.52) and lower rates of sepsis (6.5% vs. 8.6%; OR 0.77, 95% CI: 0.67–0.88) compared to those without GAD. This lower mortality may be partly explained by increased healthcare utilization and patient hypervigilance, potentially leading to evaluation at an earlier stage of disease. However, GAD was associated with longer LOS (5.4 vs. 4.9 days; OR 1.13, 95% CI: 1.09–1.17) and a markedly higher prevalence of comorbid depression (27% vs. 14%; OR 2.01, 95% CI: 1.85–2.18). No significant differences were observed in hospital costs, electrolyte derangements, malnutrition, intestinal abscess, or colonic perforation between the groups.
Discussion: Hospitalized patients with Crohn’s disease and comorbid GAD had lower inpatient mortality and reduced odds of sepsis, despite longer hospital stays and higher rates of depression. No significant differences were seen in hospital cost, malnutrition, or procedural complications. Further study is needed to examine the potential relationship between psychiatric comorbidities and inflammatory disease outcomes in this population.
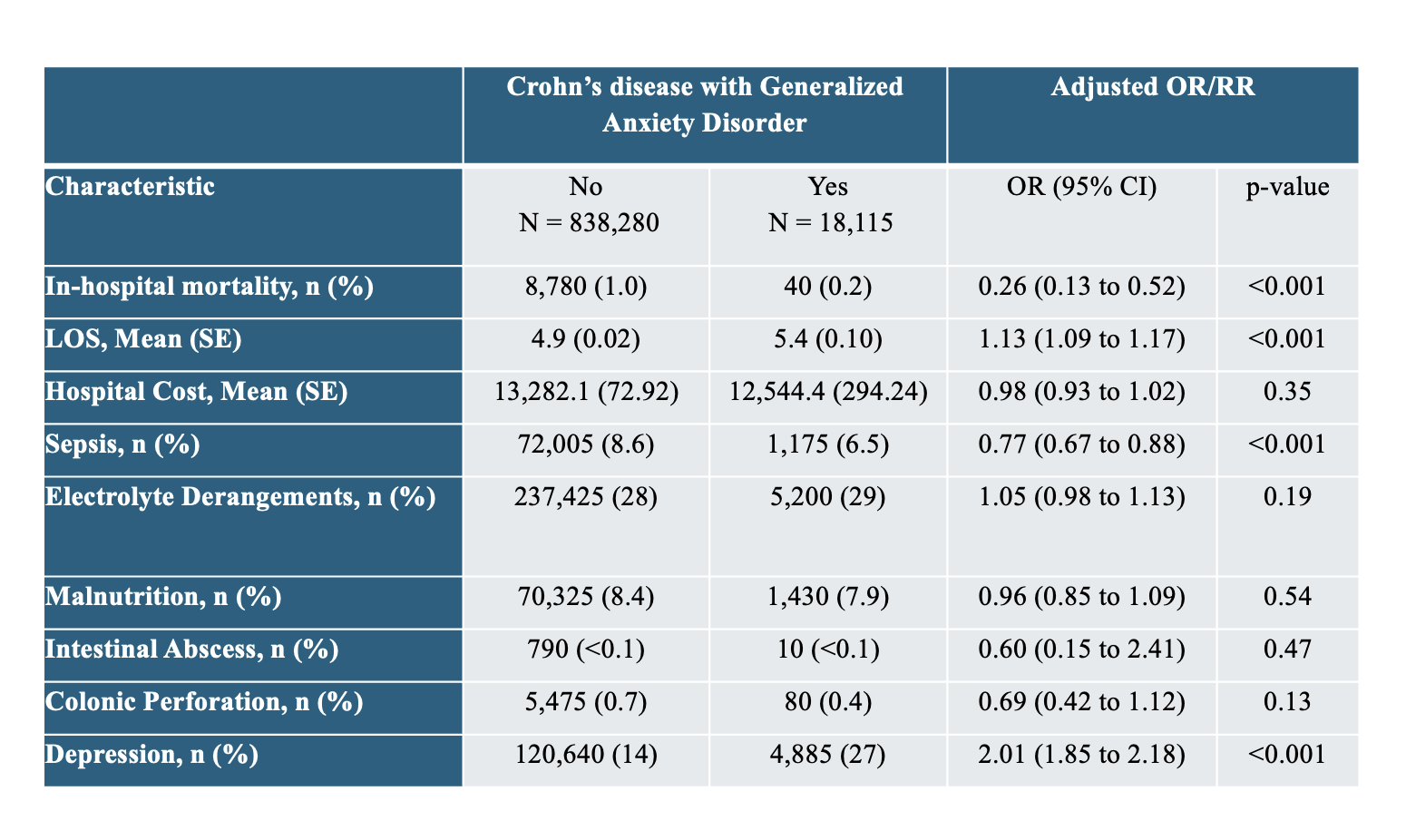
Figure: Table 1: Comparison of in-hospital outcomes among hospitalized patients with Crohn's disease by comorbid generalized anxiety disorder
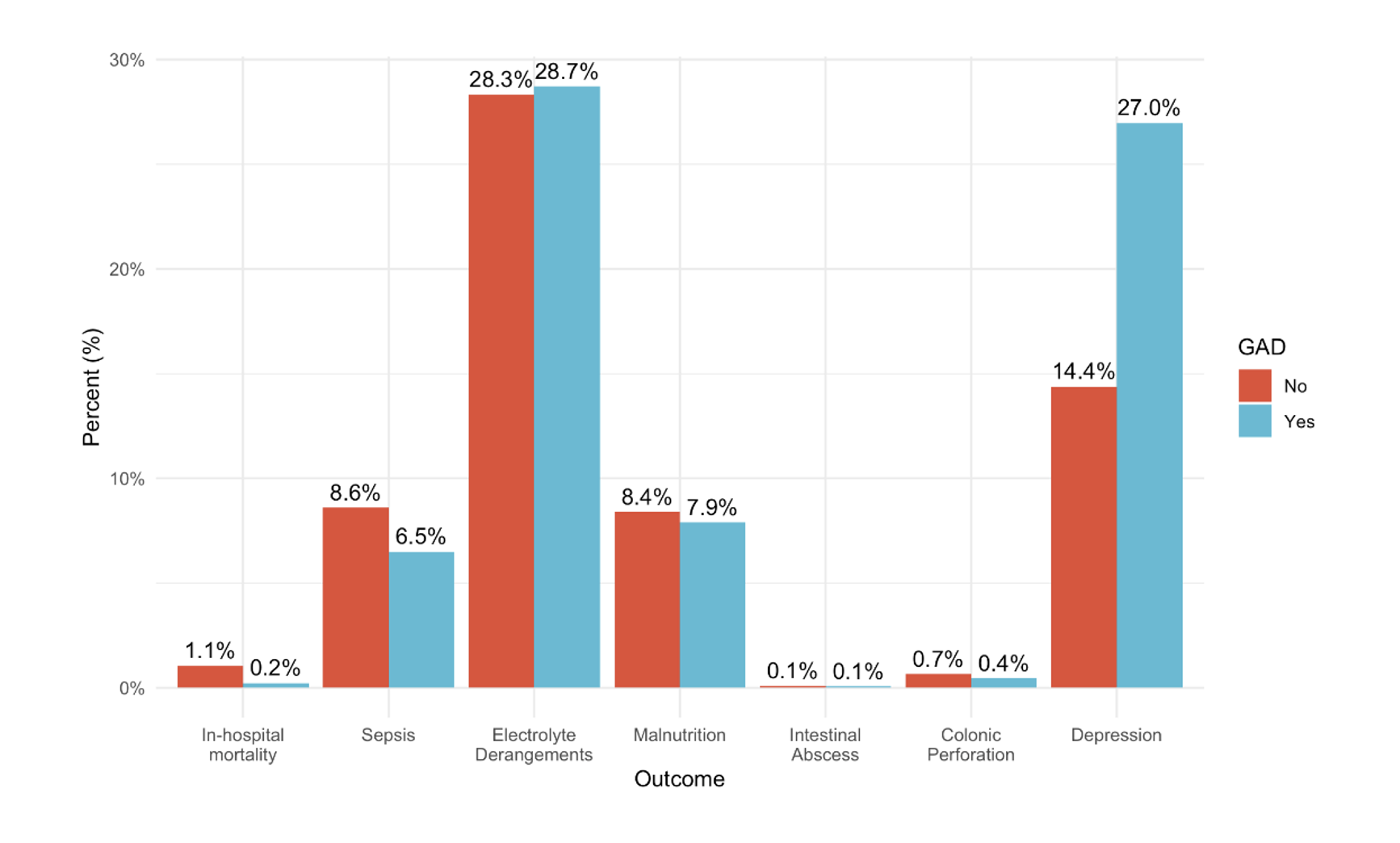
Figure: Figure 1: Bar Chart of in-hospital outcomes among hospitalized patients with Crohn's disease by comorbid generalized anxiety disorder
Disclosures:
Anwar Uddin indicated no relevant financial relationships.
Madia Ahad indicated no relevant financial relationships.
Rafat Uddin indicated no relevant financial relationships.
Xavier Aguayoarguello indicated no relevant financial relationships.
Savanna Thor indicated no relevant financial relationships.
Anwar Uddin, MD, Madia Ahad, MD, Rafat Uddin, MS, Xavier Aguayoarguello, MD, Savanna Thor, DO, MPH. P5305 - Crohn’s Disease With Comorbid Generalized Anxiety Disorder: A Retrospective Analysis of Inpatient Outcomes in a National Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
