Tuesday Poster Session
Category: IBD
P5298 - Predictors of Fecal Diversion in Perianal Crohn’s Disease: A Retrospective Review
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- LP
Lisa Pinero, MD (she/her/hers)
Icahn School of Medicine at Mount Sinai
New York City, NY
Presenting Author(s)
Lisa Pinero, MD1, Seth Bergenholtz, MD2, Kim P. Le, MD1, Jeffrey McCurdy, MD, PhD3, Serre-Yu Wong, MD, PhD2
1Icahn School of Medicine at Mount Sinai, New York City, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3University of Ottawa, Ottawa, ON, Canada
Introduction: Perianal fistulas (PAF) are a debilitating complication of Crohn’s disease (CD). Despite current therapies, up to one-third of patients with PAF undergo fecal diversion. To improve risk stratification, inform outcomes, and guide early management decisions, this single-center retrospective study aimed to identify predictors of diversion surgery in patients with perianal fistulizing Crohn’s disease (PFCD).
Methods: We conducted a retrospective study of 191 adult CD patients with PAF treated at Mount Sinai Hospital between 2005 and 2025. Patients were stratified by the outcome of fecal diversion for an indication of uncontrolled perianal disease. Univariate and multivariable logistic regression analyses identified predictors of fecal diversion.
Results: We analyzed 191 patients with PFCD: median age at PAF diagnosis of 29 (21-39); 57% male, 43% female; and included 66% White, 9% Black, 6% Asian, and 11% Hispanic patients. Overall, 35 patients (18%) required fecal diversion for PFCD. On univariate analysis, stricturing (B2) (p=0.018) and penetrating (B3) (p=0.036) phenotypes, colonic involvement (L2) (p=0.006), presence of continuous PAF activity with drainage during the first year or PAF diagnosis (p=0.002), and ≥2 ED visits in the first year of PAF diagnosis (p< 0.001) were associated with increased odds of fecal diversion.
On multivariable analysis, B2 (OR 10.61, p=0.003) and B3 (OR 8.54, p=0.003) phenotypes, colonic involvement (L2) involvement (OR 21.68, p=0.002), continuous PAF activity with drainage during the first year of PAF diagnosis (OR 10.92, p=0.024), and ≥2 ED visits within 1 year of PAF diagnosis (OR 33.32, p< 0.001) were independently associated with fecal diversion. Conversely, undergoing an exam under anesthesia (EUA) within 3 months of PAF diagnosis was associated with decreased odds of fecal diversion (OR 0.30, p=0.040).
Discussion: In this single-center study, stricturing and penetrating disease phenotypes, colonic involvement, continuous PAF activity, and frequent ED visits were independently associated with fecal diversion in patients with PFCD. Conversely, early EUAs were independently associated with reduced risk of fecal diversion. These data could help to identify at-risk patients who may benefit from early aggressive treatment strategies for PFCD.
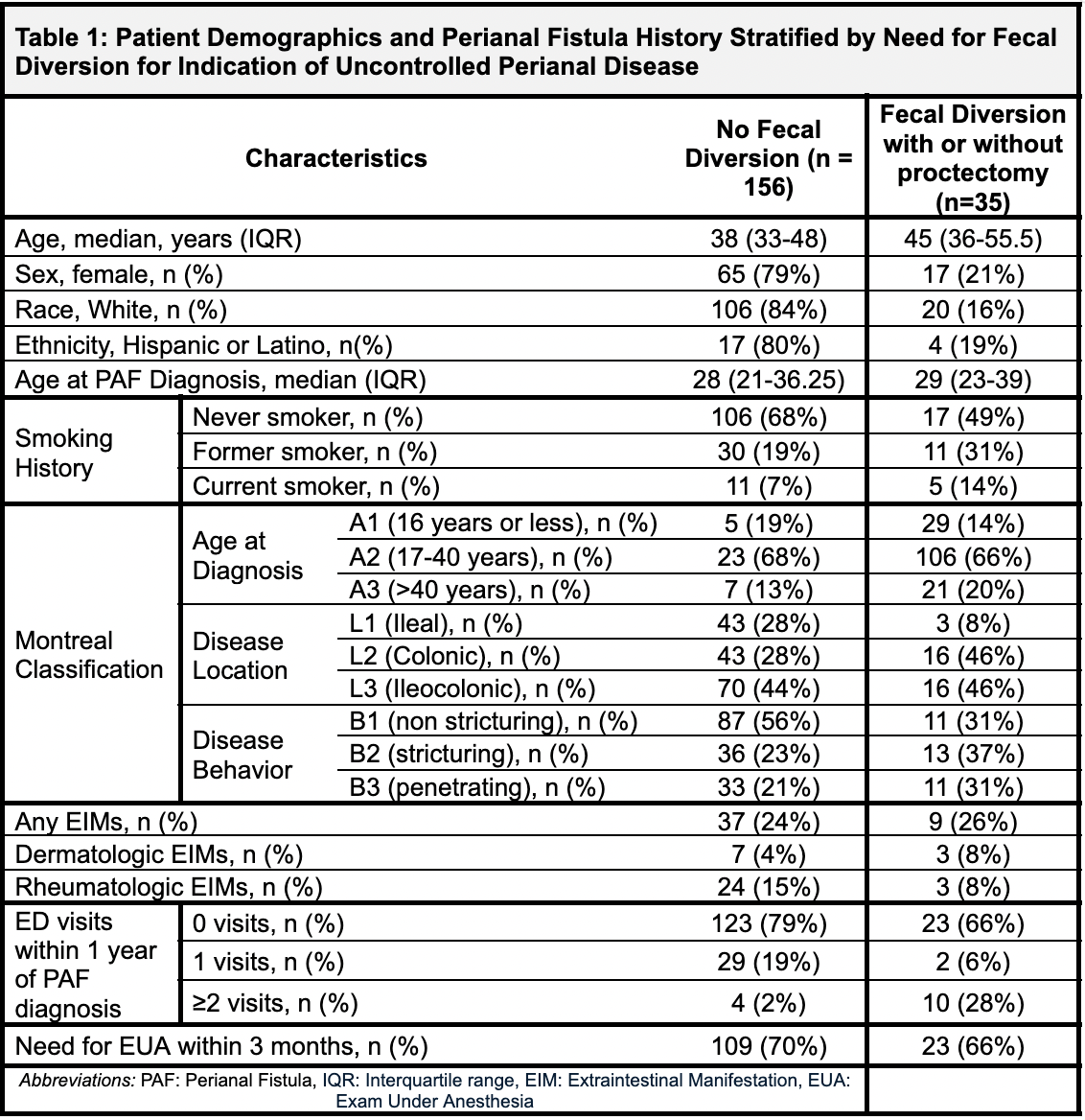
Figure: This table compares patients who required fecal diversion (with or without proctectomy) to those who did not, based on demographic data, smoking history, Montreal classification, extraintestinal manifestations (EIMs), emergency department (ED) visits, and need for exam under anesthesia (EUA).
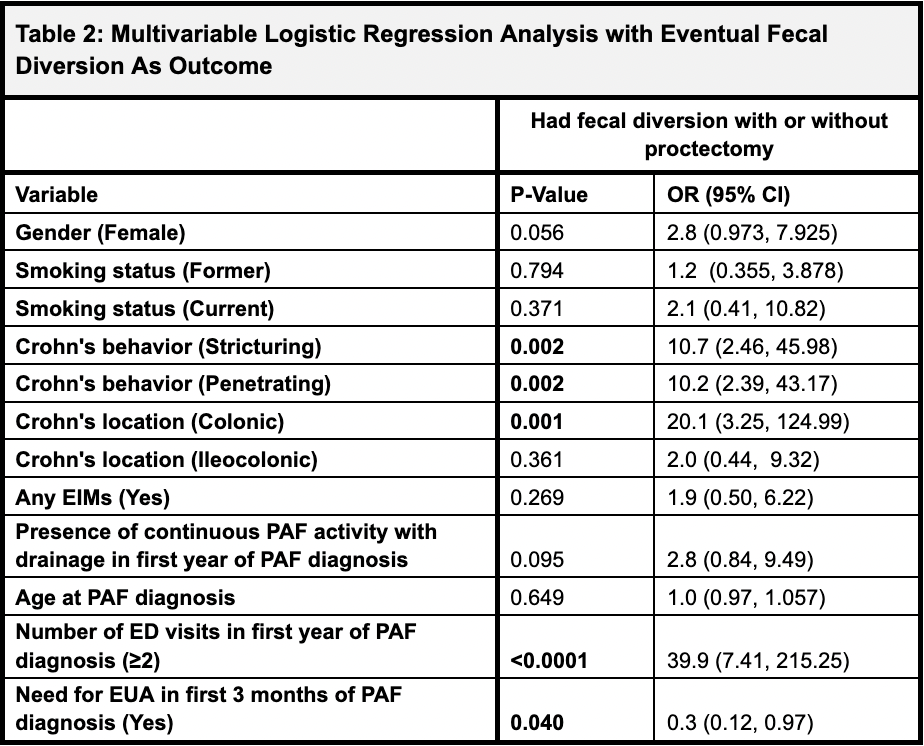
Figure: This table identifies predictors of fecal diversion (with or without proctectomy). Statistically significant predictors include stricturing behavior (OR 10.7, p=0.002), penetrating behavior (OR 10.2, p=0.002), colonic disease location (OR 20.1, p=0.001), ≥2 ED visits within the first year of perianal fistula (PAF) diagnosis (OR 39.9, p<0.0001), and need for EUA within 3 months (OR 0.3, p=0.040, indicating a protective association). Female gender showed a trend toward significance (p=0.056), while smoking status, EIMs, presence of continuous perianal fistula (PAF) activity, and age at diagnosis were not significant predictors.
Disclosures:
Lisa Pinero indicated no relevant financial relationships.
Seth Bergenholtz indicated no relevant financial relationships.
Kim Le indicated no relevant financial relationships.
Jeffrey McCurdy: Abbvie – Consultant. Amgen – Consultant. Celltrion – Consultant. Eli – Consultant. Fresenius – Consultant. Jannsen – Consultant. Kabi – Consultant. Lilly – Consultant. MERK – Consultant. Pfizer – Consultant. Takeda – Consultant.
Serre-Yu Wong: BMS – Advisory Committee/Board Member. Eli Lilly and Company – Grant/Research Support. Takeda/Trinetx – Grant/Research Support.
Lisa Pinero, MD1, Seth Bergenholtz, MD2, Kim P. Le, MD1, Jeffrey McCurdy, MD, PhD3, Serre-Yu Wong, MD, PhD2. P5298 - Predictors of Fecal Diversion in Perianal Crohn’s Disease: A Retrospective Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York City, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3University of Ottawa, Ottawa, ON, Canada
Introduction: Perianal fistulas (PAF) are a debilitating complication of Crohn’s disease (CD). Despite current therapies, up to one-third of patients with PAF undergo fecal diversion. To improve risk stratification, inform outcomes, and guide early management decisions, this single-center retrospective study aimed to identify predictors of diversion surgery in patients with perianal fistulizing Crohn’s disease (PFCD).
Methods: We conducted a retrospective study of 191 adult CD patients with PAF treated at Mount Sinai Hospital between 2005 and 2025. Patients were stratified by the outcome of fecal diversion for an indication of uncontrolled perianal disease. Univariate and multivariable logistic regression analyses identified predictors of fecal diversion.
Results: We analyzed 191 patients with PFCD: median age at PAF diagnosis of 29 (21-39); 57% male, 43% female; and included 66% White, 9% Black, 6% Asian, and 11% Hispanic patients. Overall, 35 patients (18%) required fecal diversion for PFCD. On univariate analysis, stricturing (B2) (p=0.018) and penetrating (B3) (p=0.036) phenotypes, colonic involvement (L2) (p=0.006), presence of continuous PAF activity with drainage during the first year or PAF diagnosis (p=0.002), and ≥2 ED visits in the first year of PAF diagnosis (p< 0.001) were associated with increased odds of fecal diversion.
On multivariable analysis, B2 (OR 10.61, p=0.003) and B3 (OR 8.54, p=0.003) phenotypes, colonic involvement (L2) involvement (OR 21.68, p=0.002), continuous PAF activity with drainage during the first year of PAF diagnosis (OR 10.92, p=0.024), and ≥2 ED visits within 1 year of PAF diagnosis (OR 33.32, p< 0.001) were independently associated with fecal diversion. Conversely, undergoing an exam under anesthesia (EUA) within 3 months of PAF diagnosis was associated with decreased odds of fecal diversion (OR 0.30, p=0.040).
Discussion: In this single-center study, stricturing and penetrating disease phenotypes, colonic involvement, continuous PAF activity, and frequent ED visits were independently associated with fecal diversion in patients with PFCD. Conversely, early EUAs were independently associated with reduced risk of fecal diversion. These data could help to identify at-risk patients who may benefit from early aggressive treatment strategies for PFCD.
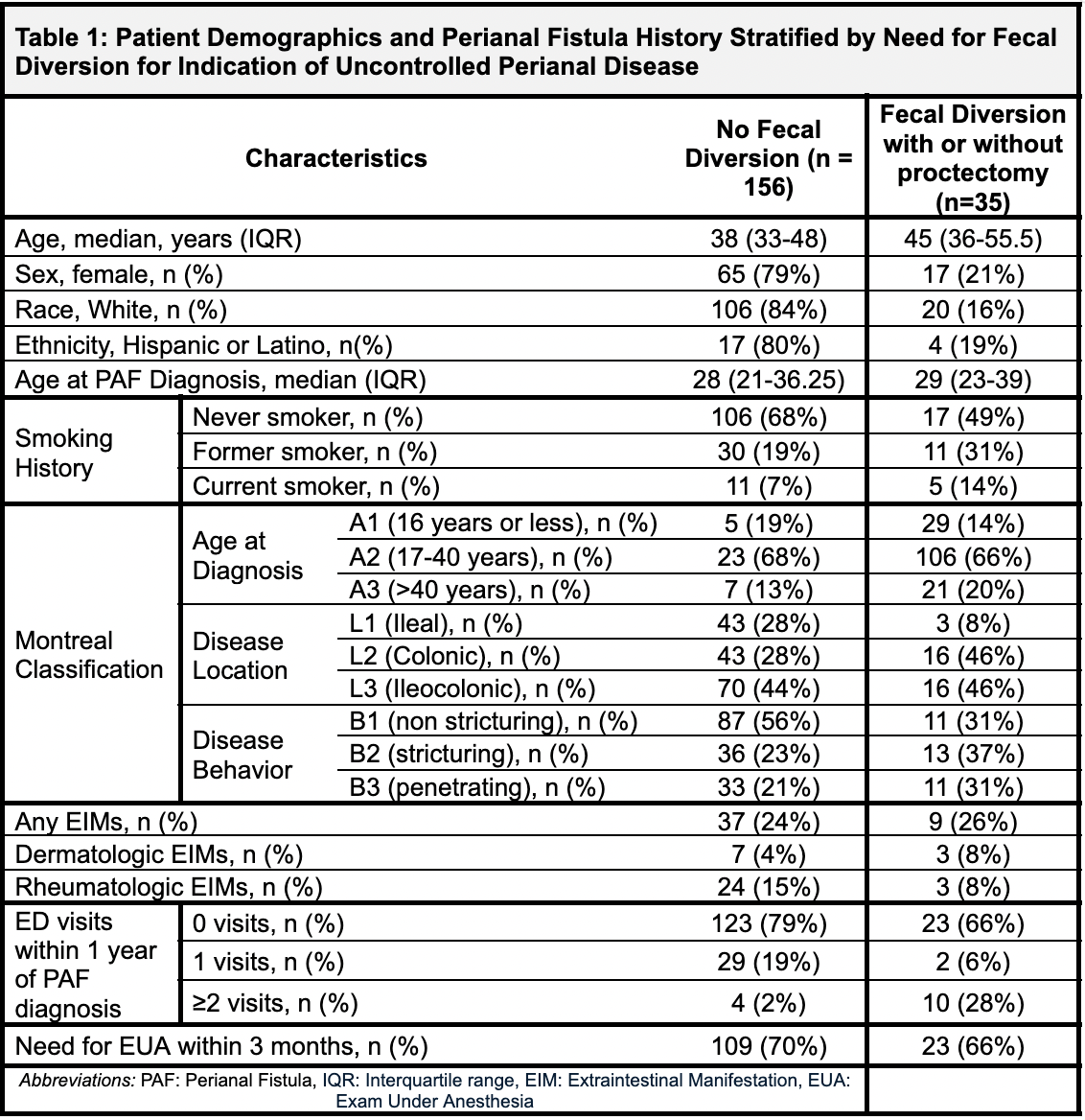
Figure: This table compares patients who required fecal diversion (with or without proctectomy) to those who did not, based on demographic data, smoking history, Montreal classification, extraintestinal manifestations (EIMs), emergency department (ED) visits, and need for exam under anesthesia (EUA).
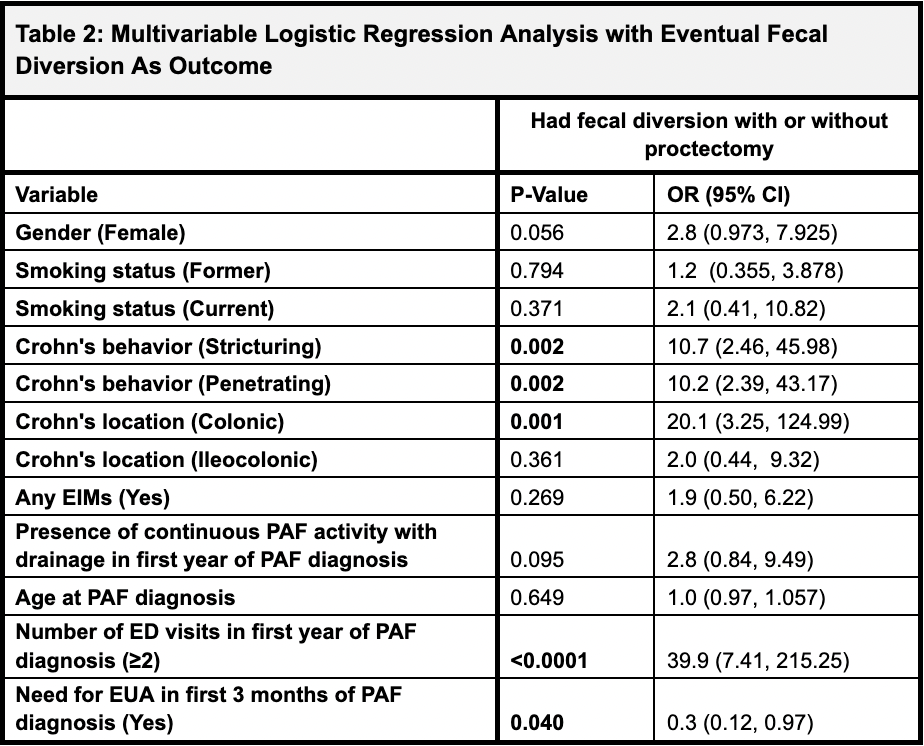
Figure: This table identifies predictors of fecal diversion (with or without proctectomy). Statistically significant predictors include stricturing behavior (OR 10.7, p=0.002), penetrating behavior (OR 10.2, p=0.002), colonic disease location (OR 20.1, p=0.001), ≥2 ED visits within the first year of perianal fistula (PAF) diagnosis (OR 39.9, p<0.0001), and need for EUA within 3 months (OR 0.3, p=0.040, indicating a protective association). Female gender showed a trend toward significance (p=0.056), while smoking status, EIMs, presence of continuous perianal fistula (PAF) activity, and age at diagnosis were not significant predictors.
Disclosures:
Lisa Pinero indicated no relevant financial relationships.
Seth Bergenholtz indicated no relevant financial relationships.
Kim Le indicated no relevant financial relationships.
Jeffrey McCurdy: Abbvie – Consultant. Amgen – Consultant. Celltrion – Consultant. Eli – Consultant. Fresenius – Consultant. Jannsen – Consultant. Kabi – Consultant. Lilly – Consultant. MERK – Consultant. Pfizer – Consultant. Takeda – Consultant.
Serre-Yu Wong: BMS – Advisory Committee/Board Member. Eli Lilly and Company – Grant/Research Support. Takeda/Trinetx – Grant/Research Support.
Lisa Pinero, MD1, Seth Bergenholtz, MD2, Kim P. Le, MD1, Jeffrey McCurdy, MD, PhD3, Serre-Yu Wong, MD, PhD2. P5298 - Predictors of Fecal Diversion in Perianal Crohn’s Disease: A Retrospective Review, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
