Tuesday Poster Session
Category: GI Bleeding
P5294 - A Rare Case of Hemosuccus Pancreaticus Caused by Pancreatic Pseudoaneurysm
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AH
Anam Herekar, MD
Medical College of Georgia at Augusta University
Augusta, GA
Presenting Author(s)
Anam Herekar, MD1, John N. McNally, DO1, Karan Sharma, MS2, Rishik Marneni, 3, Davis Hardell, 4, Angela Barnes, MD1, Stephen Schaffner, DO4, Amol Sharma, MD, MSc, FACG5
1Medical College of Georgia at Augusta University, Augusta, GA; 2Medical College of Georgia at Augusta University, Suwanee, GA; 3University of Missouri - Kansas City School of Medicine, Kansas City, MO; 4Augusta University Medical Center, Augusta, GA; 5Medical University of South Carolina, Charleston, SC
Introduction: Hemosuccus pancreaticus causes 1/1,500 gastrointestinal (GI) bleeding cases and has a male predilection. It involves bleeding from the Ampulla of Vater into the duodenum.1 There are multiple potential causes of this condition, though the most common cause involves rupture of a splenic artery aneurysm associated with acute or chronic pancreatitis.2The resultant inflammation from pancreatitis leads to vascular wall weakening leading to rupture. Pseudoaneurysm of hepatic, gastroduodenal, and hepatoduodenal arteries have also been implicated in literature.2 Since the bleeding can be intermittent, it is very challenging to confirm it endoscopically.
Case Description/
Methods: A 63-year-old male presented from surgery clinic with a two-week history of epigastric pain, vomiting, and rectal bleeding. Labs on admission were notable for hemoglobin 6.1 g/dl and lipase 3129 U/l. CT of abdomen/pelvis revealed acute interstitial edematous pancreatitis. Of note, the patient had a history of alcohol abuse, portal vein thrombosis, and necrotizing pancreatitis due to mass effect caused by pseudoaneurysm with high flow arterio-portal fistula formation supplied from a pancreaticoduodenal arterial arcade located at the pancreatic head for which he had history of cystgastrostomy. (Fig1) He had history of coil embolization followed by surgical ligation of the feeding vessels. EGD performed during admission revealed fresh blood at the Ampulla of Vater suggestive of hemosuccus pancreaticus. (Fig 2) Bleeding subsequently stopped. By the time, arteriogram was performed five days later, it was normal. When patient presented with bleeding again two months later, new hemorrhage was noted within the partially thrombosed pseudoaneurysm sac arising within the distribution of the head of the pancreas for which he underwent gastroduodenal artery pseudoaneurysm embolization.
Discussion: Hemosuccus pancreaticus is a rare cause of upper GI bleeding that should be considered in patients with pancreatitis. Early imaging and endoscopic evaluation is imperative to ensure timely intervention. Awareness of this condition, along with timely multidisciplinary collaboration, are essential components in both an accurate diagnosis and favorable outcome.
References
1. Yu, P, Gong, J. Hemosuccus pancreaticus: A mini-review. Ann Med Surg (Lond). 2018 Mar 9;28:45–48.
2. Toyoki, Y, Hakamada, K, Narumi, S, et al. Hemosuccus pancreaticus: problems and pitfalls in diagnosis and treatment. World J Gastroenterology. 2008 May 7;14(17): 2776–9.
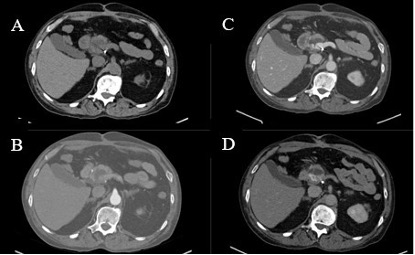
Figure: Figure 1. Pseudoaneurysm seen in non-contrast (A), arterial (B), portal-venous (C), and delayed phase (D).

Figure: Figure 2. Bleeding in second part of duodenum.
Disclosures:
Anam Herekar indicated no relevant financial relationships.
John McNally indicated no relevant financial relationships.
Karan Sharma indicated no relevant financial relationships.
Rishik Marneni indicated no relevant financial relationships.
Davis Hardell indicated no relevant financial relationships.
Angela Barnes indicated no relevant financial relationships.
Stephen Schaffner indicated no relevant financial relationships.
Amol Sharma indicated no relevant financial relationships.
Anam Herekar, MD1, John N. McNally, DO1, Karan Sharma, MS2, Rishik Marneni, 3, Davis Hardell, 4, Angela Barnes, MD1, Stephen Schaffner, DO4, Amol Sharma, MD, MSc, FACG5. P5294 - A Rare Case of Hemosuccus Pancreaticus Caused by Pancreatic Pseudoaneurysm, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Medical College of Georgia at Augusta University, Augusta, GA; 2Medical College of Georgia at Augusta University, Suwanee, GA; 3University of Missouri - Kansas City School of Medicine, Kansas City, MO; 4Augusta University Medical Center, Augusta, GA; 5Medical University of South Carolina, Charleston, SC
Introduction: Hemosuccus pancreaticus causes 1/1,500 gastrointestinal (GI) bleeding cases and has a male predilection. It involves bleeding from the Ampulla of Vater into the duodenum.1 There are multiple potential causes of this condition, though the most common cause involves rupture of a splenic artery aneurysm associated with acute or chronic pancreatitis.2The resultant inflammation from pancreatitis leads to vascular wall weakening leading to rupture. Pseudoaneurysm of hepatic, gastroduodenal, and hepatoduodenal arteries have also been implicated in literature.2 Since the bleeding can be intermittent, it is very challenging to confirm it endoscopically.
Case Description/
Methods: A 63-year-old male presented from surgery clinic with a two-week history of epigastric pain, vomiting, and rectal bleeding. Labs on admission were notable for hemoglobin 6.1 g/dl and lipase 3129 U/l. CT of abdomen/pelvis revealed acute interstitial edematous pancreatitis. Of note, the patient had a history of alcohol abuse, portal vein thrombosis, and necrotizing pancreatitis due to mass effect caused by pseudoaneurysm with high flow arterio-portal fistula formation supplied from a pancreaticoduodenal arterial arcade located at the pancreatic head for which he had history of cystgastrostomy. (Fig1) He had history of coil embolization followed by surgical ligation of the feeding vessels. EGD performed during admission revealed fresh blood at the Ampulla of Vater suggestive of hemosuccus pancreaticus. (Fig 2) Bleeding subsequently stopped. By the time, arteriogram was performed five days later, it was normal. When patient presented with bleeding again two months later, new hemorrhage was noted within the partially thrombosed pseudoaneurysm sac arising within the distribution of the head of the pancreas for which he underwent gastroduodenal artery pseudoaneurysm embolization.
Discussion: Hemosuccus pancreaticus is a rare cause of upper GI bleeding that should be considered in patients with pancreatitis. Early imaging and endoscopic evaluation is imperative to ensure timely intervention. Awareness of this condition, along with timely multidisciplinary collaboration, are essential components in both an accurate diagnosis and favorable outcome.
References
1. Yu, P, Gong, J. Hemosuccus pancreaticus: A mini-review. Ann Med Surg (Lond). 2018 Mar 9;28:45–48.
2. Toyoki, Y, Hakamada, K, Narumi, S, et al. Hemosuccus pancreaticus: problems and pitfalls in diagnosis and treatment. World J Gastroenterology. 2008 May 7;14(17): 2776–9.
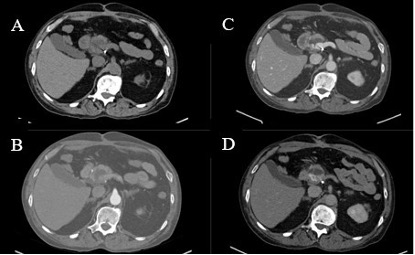
Figure: Figure 1. Pseudoaneurysm seen in non-contrast (A), arterial (B), portal-venous (C), and delayed phase (D).

Figure: Figure 2. Bleeding in second part of duodenum.
Disclosures:
Anam Herekar indicated no relevant financial relationships.
John McNally indicated no relevant financial relationships.
Karan Sharma indicated no relevant financial relationships.
Rishik Marneni indicated no relevant financial relationships.
Davis Hardell indicated no relevant financial relationships.
Angela Barnes indicated no relevant financial relationships.
Stephen Schaffner indicated no relevant financial relationships.
Amol Sharma indicated no relevant financial relationships.
Anam Herekar, MD1, John N. McNally, DO1, Karan Sharma, MS2, Rishik Marneni, 3, Davis Hardell, 4, Angela Barnes, MD1, Stephen Schaffner, DO4, Amol Sharma, MD, MSc, FACG5. P5294 - A Rare Case of Hemosuccus Pancreaticus Caused by Pancreatic Pseudoaneurysm, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
