Tuesday Poster Session
Category: GI Bleeding
P5291 - Iron Tablet Gastropathy: When Iron Supplementation for GI Bleeding Leads to More GI Bleeding
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yannis S. Lafazanos, DO (he/him/his)
Advocate Lutheran General
Long Grove, IL
Presenting Author(s)
Yannis S. Lafazanos, DO1, Robin David, MD2, Jennifer Kang, MD2, Nahren Asado, MD2, Eli Ehrenpreis, MD, FACG3
1Advocate Lutheran General, Long Grove, IL; 2Advocate Lutheran General Hospital, Park Ridge, IL; 3Advocate Lutheran General, Park Ridge, IL
Introduction: Iron deficiency anemia is the most common cause of anemia, and its supplementation is typically done via oral tablets. Exposure of iron to the GI tract can produce many side effects, including stomach upset, pyrosis, and constipation, along with darker stools. Pill-induced gastropathy is another adverse symptom of iron exposure, but not well described at therapeutic iron levels. Medication-associated inflammatory changes occur in about 0.7% of patients and are due to the oxidative stress of iron. Even less described is severe iron tablet gastropathy leading to bleeding unable to be managed via endoscopic methods, eventually requiring partial gastrectomy.
Case Description/
Methods: A 67-year-old female with a history of CLL on darbepoetin alfa and iron deficiency anemia, presented to the ED for evaluation of hematemesis and melena. She reported multiple bouts of melenic stools over the previous 24 hours, beginning after an episode of hematemesis. She denied recent alcohol, NSAID, aspirin, or anticoagulant use. She reported the use of tirzepatide and daily iron tablets. She was hemodynamically stable and saturated well on room air. Examination was remarkable for conjunctival pallor and melena on digital rectal exam. Labwork was notable for chronic leukocytosis to 23.9 K/mcL, hemoglobin 6.8 g/dL (baseline 8.0), and acute kidney injury. She was transfused blood and given intravenous pantoprazole. Endoscopy noted a large gastric antral mass to which hemostatic spray was applied (Figure 1). Biopsy revealed foveolar hyperplasia, likely related to iron tablet use (Figure 2). Despite intervention, her hemoglobin continued to decline, requiring further transfusion. General surgery took the patient for anterior gastrotomy, resulting in partial gastrectomy with antral mass removal and surrounding serosal repair. Counts stabilized, and she was discharged on intravenous iron infusions.
Discussion: Iron tablet-induced gastropathy is a relatively underdiagnosed phenomenon that is the result of oxidative stress to the mucosal lining of the stomach. In our patient, chronic iron supplementation produced a milieu of inflammation that led to gastric mass formation. Her concurrent use of a dual GLP-1 and GIP agonist potentiated this, leading to slower gut transit and extended iron tablet exposure to the stomach, likely worsening the degree of inflammation. Given the prevalence of iron deficiency anemia and use of oral iron supplementation, the generalist and gastroenterologist should be familiar with this risk.
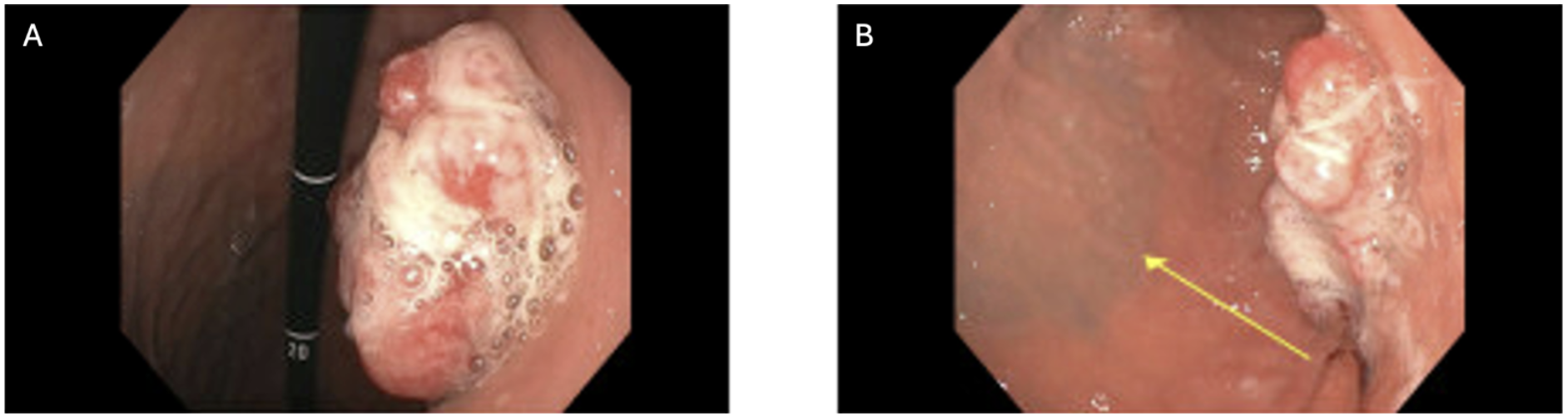
Figure: Figure 1. Endoscopy. Mass in the gastric antrum. Tattoo from previous endoscopy, completed three years prior, across from the gastric mass (yellow arrow).

Figure: Figure 2. Pathology. (A) Photomicrograph of submucosal resection of the gastric mass, showing polypoid lesion with elongated, tortuous and hyperplastic foveolar epithelium. (50x; H&E). (B) Higher power view of hyperplastic gastric mucosa with brown crystalline deposits (200x; H&E). (C) Brown crystalline deposits are positive with iron histochemical staining (200x).
Disclosures:
Yannis Lafazanos indicated no relevant financial relationships.
Robin David indicated no relevant financial relationships.
Jennifer Kang indicated no relevant financial relationships.
Nahren Asado indicated no relevant financial relationships.
Eli Ehrenpreis: E2Bio Consultants – Intellectual Property/Patents, CEO, Owner/Ownership Interest. E2Bio Life Sciences – CEO, Owner/Ownership Interest.
Yannis S. Lafazanos, DO1, Robin David, MD2, Jennifer Kang, MD2, Nahren Asado, MD2, Eli Ehrenpreis, MD, FACG3. P5291 - Iron Tablet Gastropathy: When Iron Supplementation for GI Bleeding Leads to More GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Advocate Lutheran General, Long Grove, IL; 2Advocate Lutheran General Hospital, Park Ridge, IL; 3Advocate Lutheran General, Park Ridge, IL
Introduction: Iron deficiency anemia is the most common cause of anemia, and its supplementation is typically done via oral tablets. Exposure of iron to the GI tract can produce many side effects, including stomach upset, pyrosis, and constipation, along with darker stools. Pill-induced gastropathy is another adverse symptom of iron exposure, but not well described at therapeutic iron levels. Medication-associated inflammatory changes occur in about 0.7% of patients and are due to the oxidative stress of iron. Even less described is severe iron tablet gastropathy leading to bleeding unable to be managed via endoscopic methods, eventually requiring partial gastrectomy.
Case Description/
Methods: A 67-year-old female with a history of CLL on darbepoetin alfa and iron deficiency anemia, presented to the ED for evaluation of hematemesis and melena. She reported multiple bouts of melenic stools over the previous 24 hours, beginning after an episode of hematemesis. She denied recent alcohol, NSAID, aspirin, or anticoagulant use. She reported the use of tirzepatide and daily iron tablets. She was hemodynamically stable and saturated well on room air. Examination was remarkable for conjunctival pallor and melena on digital rectal exam. Labwork was notable for chronic leukocytosis to 23.9 K/mcL, hemoglobin 6.8 g/dL (baseline 8.0), and acute kidney injury. She was transfused blood and given intravenous pantoprazole. Endoscopy noted a large gastric antral mass to which hemostatic spray was applied (Figure 1). Biopsy revealed foveolar hyperplasia, likely related to iron tablet use (Figure 2). Despite intervention, her hemoglobin continued to decline, requiring further transfusion. General surgery took the patient for anterior gastrotomy, resulting in partial gastrectomy with antral mass removal and surrounding serosal repair. Counts stabilized, and she was discharged on intravenous iron infusions.
Discussion: Iron tablet-induced gastropathy is a relatively underdiagnosed phenomenon that is the result of oxidative stress to the mucosal lining of the stomach. In our patient, chronic iron supplementation produced a milieu of inflammation that led to gastric mass formation. Her concurrent use of a dual GLP-1 and GIP agonist potentiated this, leading to slower gut transit and extended iron tablet exposure to the stomach, likely worsening the degree of inflammation. Given the prevalence of iron deficiency anemia and use of oral iron supplementation, the generalist and gastroenterologist should be familiar with this risk.
Figure: Figure 1. Endoscopy. Mass in the gastric antrum. Tattoo from previous endoscopy, completed three years prior, across from the gastric mass (yellow arrow).

Figure: Figure 2. Pathology. (A) Photomicrograph of submucosal resection of the gastric mass, showing polypoid lesion with elongated, tortuous and hyperplastic foveolar epithelium. (50x; H&E). (B) Higher power view of hyperplastic gastric mucosa with brown crystalline deposits (200x; H&E). (C) Brown crystalline deposits are positive with iron histochemical staining (200x).
Disclosures:
Yannis Lafazanos indicated no relevant financial relationships.
Robin David indicated no relevant financial relationships.
Jennifer Kang indicated no relevant financial relationships.
Nahren Asado indicated no relevant financial relationships.
Eli Ehrenpreis: E2Bio Consultants – Intellectual Property/Patents, CEO, Owner/Ownership Interest. E2Bio Life Sciences – CEO, Owner/Ownership Interest.
Yannis S. Lafazanos, DO1, Robin David, MD2, Jennifer Kang, MD2, Nahren Asado, MD2, Eli Ehrenpreis, MD, FACG3. P5291 - Iron Tablet Gastropathy: When Iron Supplementation for GI Bleeding Leads to More GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
