Tuesday Poster Session
Category: GI Bleeding
P5281 - Gastrointestinal AA Amyloidosis Uncovered in a Trauma Patient With ESRD
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JL
Julie Lee, DO
HonorHealth
Scottsdale, AZ
Presenting Author(s)
Julie Lee, DO1, Shradha Gupta, MD2, Navroop Nagra, MD1, Deepa Shah, MD, FACG1, Cory Fraser, MD1
1HonorHealth, Scottsdale, AZ; 2HonorHealth, Phoenix, AZ
Introduction: AA amyloidosis is a systemic condition characterized by extracellular deposition of serum amyloid A (SAA) protein, an acute-phase reactant elevated during chronic inflammation. It commonly affects the kidneys, but gastrointestinal (GI) involvement can occur in up to 60% of cases, often going unrecognized due to nonspecific symptoms such as weight loss, early satiety, diarrhea, or occult bleeding. GI amyloid deposition may lead to mucosal friability, ulceration, and iron-deficiency anemia, with the stomach being a less common site. Patients with end-stage renal disease (ESRD) are at risk due to persistent inflammation and impaired SAA clearance. Early detection through endoscopic biopsy and Congo red staining is essential for diagnosis and management.
Case Description/
Methods: We present a 79-year-old man with ESRD on hemodialysis, hypertension, hyperlipidemia, and an extensive vascular history, including TAVR and multiple aortic aneurysm repairs, who was transferred to our emergency department after a fall resulting in facial trauma and left-sided rib fractures. He was found to have a hemoglobin of 6.6 g/dL on admission and was transfused. He denied hematemesis, melena, or hematochezia. He did report 1-2 loose stools daily and tested positive for fecal occult blood. CT abdomen was unremarkable. The patient was on chronic iron therapy and aspirin 81 mg daily. EGD and colonoscopy were performed, showing erosive gastritis, friable colonic mucosa with contact bleeding, and colon polyps. Biopsies taken from the stomach and random colon biopsies were notable for amyloid deposition in the lamina propria, and subtype analysis confirmed AA amyloid. His acute anemia was attributed to chronic GI blood loss from gastrointestinal amyloid infiltration, superimposed on his complex comorbid state with ESRD. The patient has not had a kidney biopsy confirmed, but we suspect that amyloid is likely at least a contributor to the ESRD.
Discussion: This case underscores the importance of considering GI amyloidosis in dialysis patients presenting with anemia and occult GI bleeding, especially when imaging is unrevealing and symptoms are vague. Gastric involvement by AA amyloid is uncommon but clinically significant, as it may contribute to chronic blood loss and transfusion dependence. Prompt histological diagnosis can guide appropriate supportive care and long-term monitoring. In patients with ESRD, AA amyloidosis should remain on the differential.
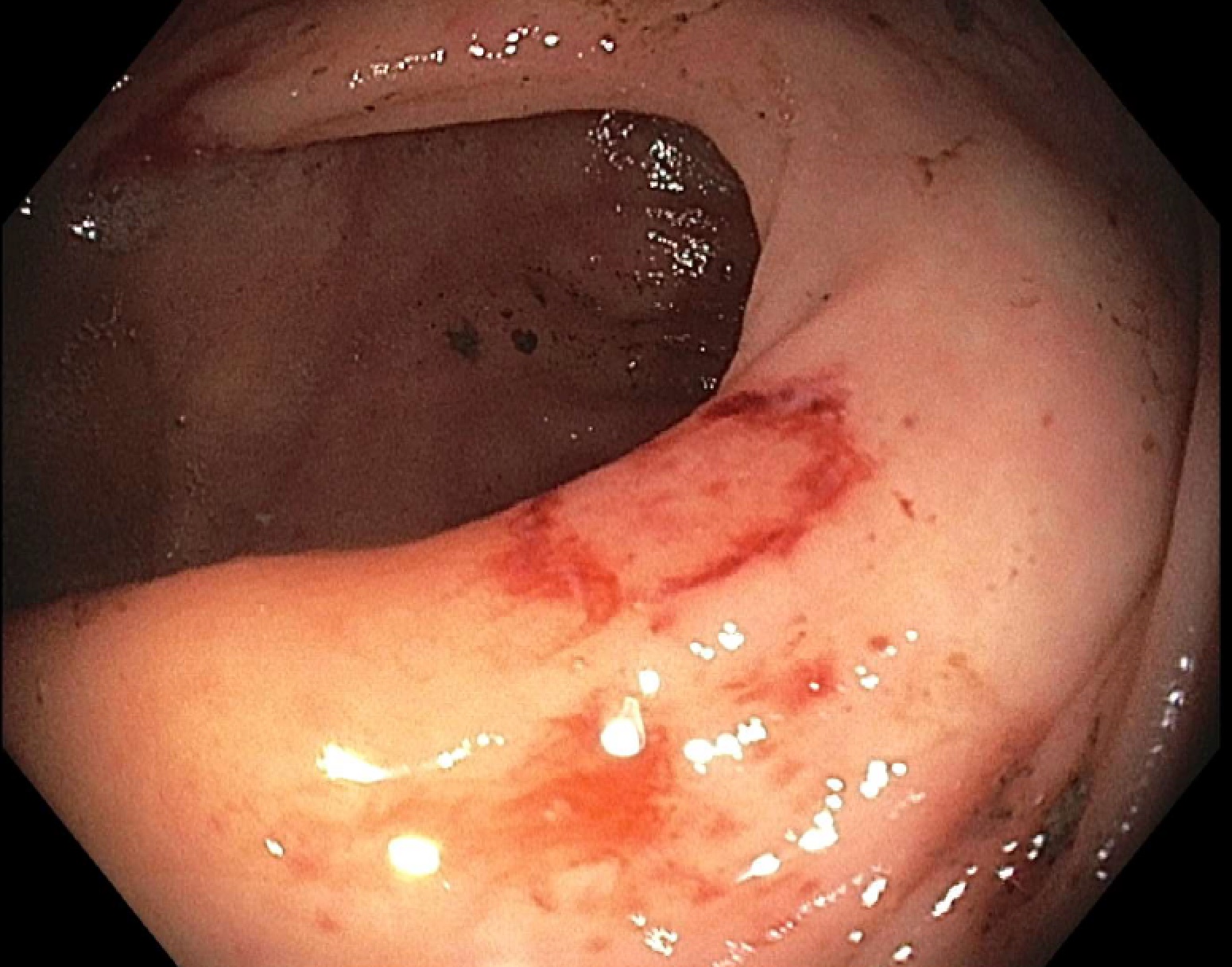
Figure: Congo red stain - hallmark of amyloid deposition.
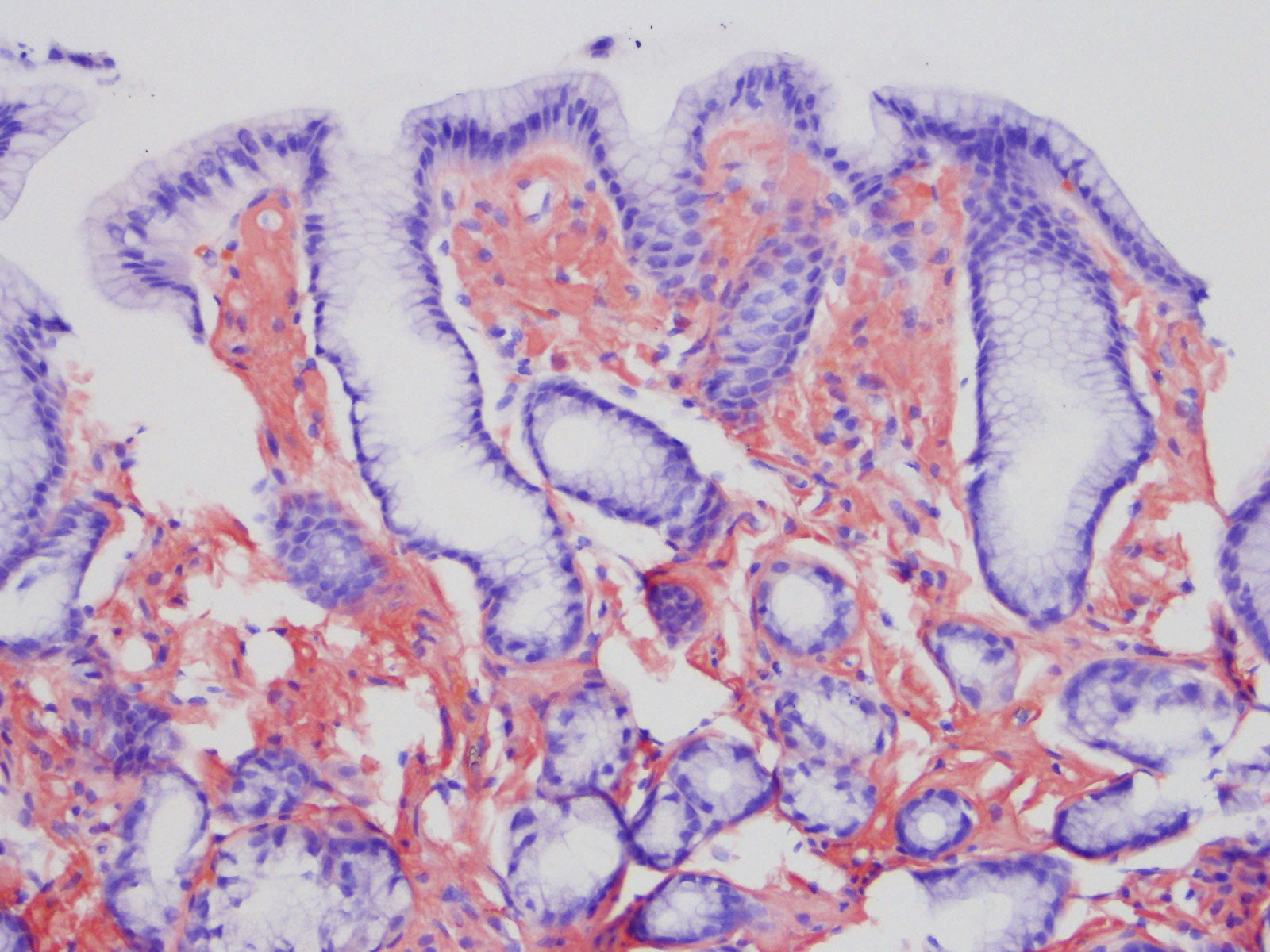
Figure: Friable (with contact bleeding) mucosa in the entire examined colon.
Disclosures:
Julie Lee indicated no relevant financial relationships.
Shradha Gupta indicated no relevant financial relationships.
Navroop Nagra indicated no relevant financial relationships.
Deepa Shah indicated no relevant financial relationships.
Cory Fraser indicated no relevant financial relationships.
Julie Lee, DO1, Shradha Gupta, MD2, Navroop Nagra, MD1, Deepa Shah, MD, FACG1, Cory Fraser, MD1. P5281 - Gastrointestinal AA Amyloidosis Uncovered in a Trauma Patient With ESRD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HonorHealth, Scottsdale, AZ; 2HonorHealth, Phoenix, AZ
Introduction: AA amyloidosis is a systemic condition characterized by extracellular deposition of serum amyloid A (SAA) protein, an acute-phase reactant elevated during chronic inflammation. It commonly affects the kidneys, but gastrointestinal (GI) involvement can occur in up to 60% of cases, often going unrecognized due to nonspecific symptoms such as weight loss, early satiety, diarrhea, or occult bleeding. GI amyloid deposition may lead to mucosal friability, ulceration, and iron-deficiency anemia, with the stomach being a less common site. Patients with end-stage renal disease (ESRD) are at risk due to persistent inflammation and impaired SAA clearance. Early detection through endoscopic biopsy and Congo red staining is essential for diagnosis and management.
Case Description/
Methods: We present a 79-year-old man with ESRD on hemodialysis, hypertension, hyperlipidemia, and an extensive vascular history, including TAVR and multiple aortic aneurysm repairs, who was transferred to our emergency department after a fall resulting in facial trauma and left-sided rib fractures. He was found to have a hemoglobin of 6.6 g/dL on admission and was transfused. He denied hematemesis, melena, or hematochezia. He did report 1-2 loose stools daily and tested positive for fecal occult blood. CT abdomen was unremarkable. The patient was on chronic iron therapy and aspirin 81 mg daily. EGD and colonoscopy were performed, showing erosive gastritis, friable colonic mucosa with contact bleeding, and colon polyps. Biopsies taken from the stomach and random colon biopsies were notable for amyloid deposition in the lamina propria, and subtype analysis confirmed AA amyloid. His acute anemia was attributed to chronic GI blood loss from gastrointestinal amyloid infiltration, superimposed on his complex comorbid state with ESRD. The patient has not had a kidney biopsy confirmed, but we suspect that amyloid is likely at least a contributor to the ESRD.
Discussion: This case underscores the importance of considering GI amyloidosis in dialysis patients presenting with anemia and occult GI bleeding, especially when imaging is unrevealing and symptoms are vague. Gastric involvement by AA amyloid is uncommon but clinically significant, as it may contribute to chronic blood loss and transfusion dependence. Prompt histological diagnosis can guide appropriate supportive care and long-term monitoring. In patients with ESRD, AA amyloidosis should remain on the differential.
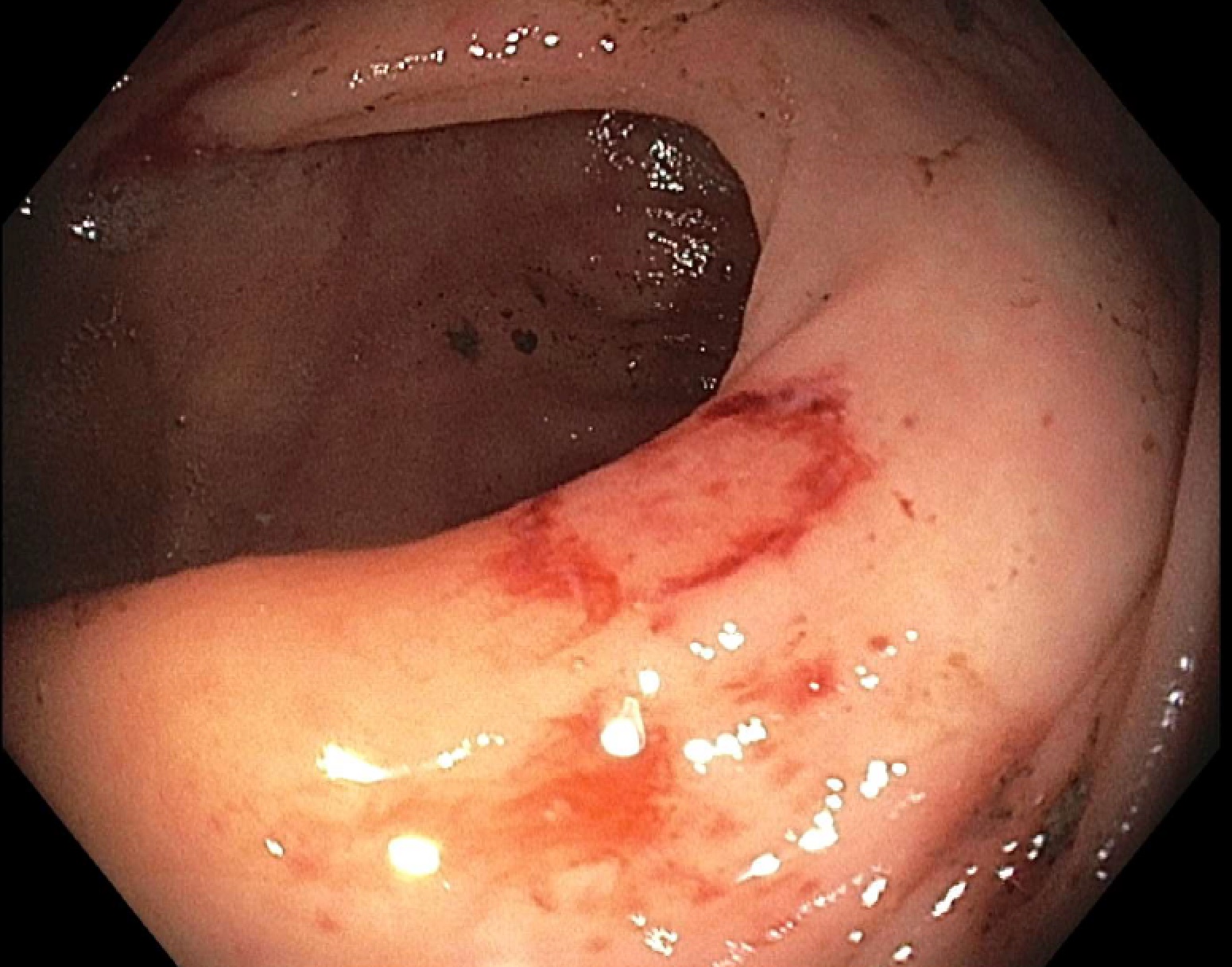
Figure: Congo red stain - hallmark of amyloid deposition.
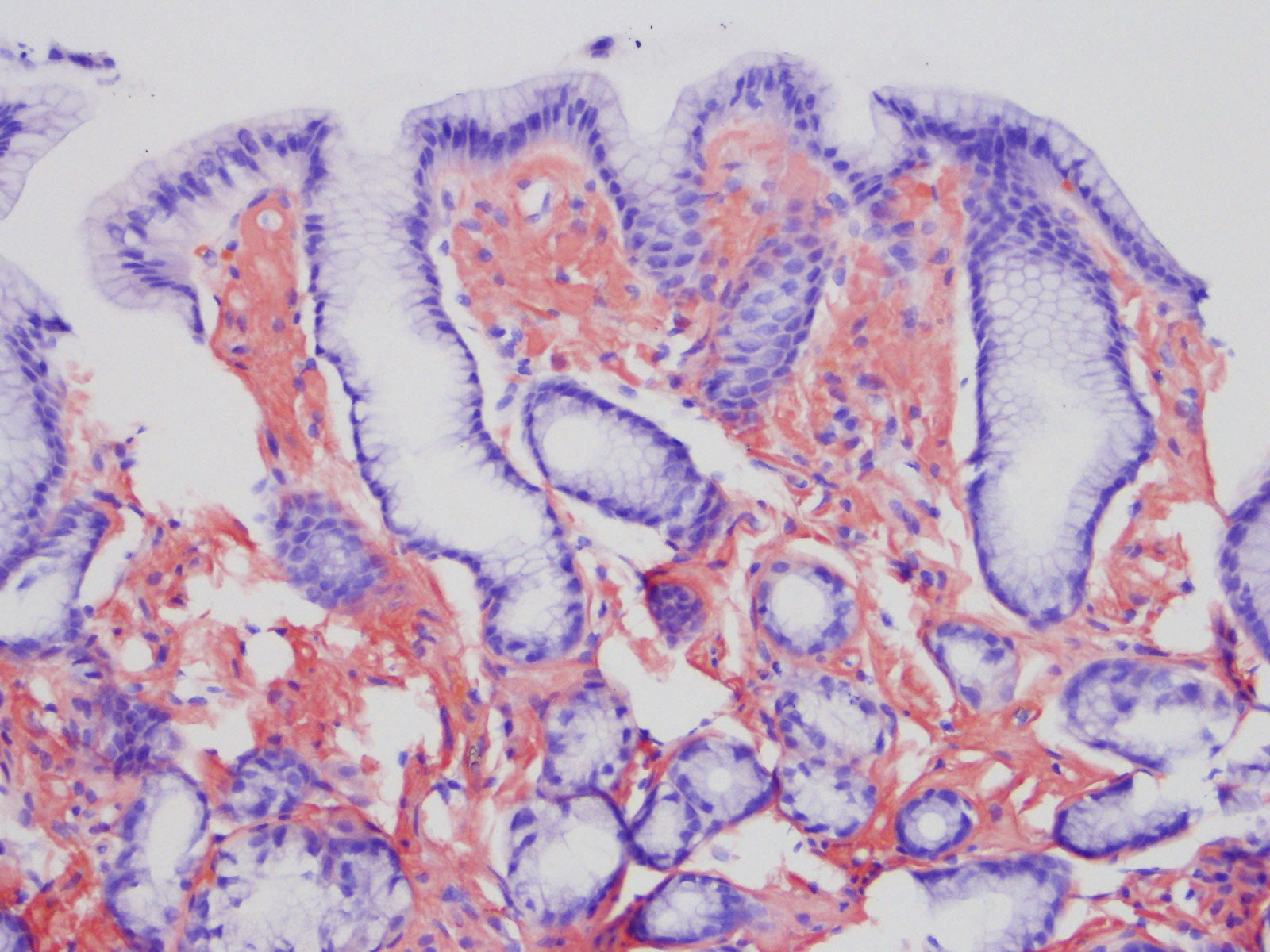
Figure: Friable (with contact bleeding) mucosa in the entire examined colon.
Disclosures:
Julie Lee indicated no relevant financial relationships.
Shradha Gupta indicated no relevant financial relationships.
Navroop Nagra indicated no relevant financial relationships.
Deepa Shah indicated no relevant financial relationships.
Cory Fraser indicated no relevant financial relationships.
Julie Lee, DO1, Shradha Gupta, MD2, Navroop Nagra, MD1, Deepa Shah, MD, FACG1, Cory Fraser, MD1. P5281 - Gastrointestinal AA Amyloidosis Uncovered in a Trauma Patient With ESRD, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
