Tuesday Poster Session
Category: GI Bleeding
P5256 - Refractory Anemia Secondary to Acquired Blue Rubber Bleb Nevus Syndrome
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Juan C. Santiago-Gonzalez, MD, MSc (he/him/his)
Howard University Hospital
Washington, DC
Presenting Author(s)
Juan C. Santiago-Gonzalez, MD, MSc1, Pinky Bai, MD1, Mesay Asfaw, MD2, Amro Abdellatief, MD1, Kristen Miller, MD3, Adeyinka Laiyemo, MD, MPH4
1Howard University Hospital, Washington, DC; 2Howard University, Washington, DC; 3Howard University Hospital | 2041 GEORGIA AVE NW | WASHINGTON, DC, Washington, DC; 4Howard University Hospital | 2041 GEORGIA AVE NW | WASHINGTON, DC, Washington DC, DC
Introduction: Blue Rubber Bleb Nevus Syndrome (BRBNS) is a rare vascular anomaly syndrome characterized by multifocal venous malformations (VMs) predominantly involving the skin and gastrointestinal (GI) tract but can also affect other organs. The prevalence of BRBNS is unknown, with fewer than 200 cases reported globally. Most cases are sporadic, although an autosomal dominant form linked to chromosome 9p has been described. Chronic GI bleeding from VMs leads to anemia, requiring lifelong treatment with iron supplementation or blood transfusions.
Case Description/
Methods: Case of a 88-year-old female with coronary artery disease post-PCI and metastatic duodenal ampullary adenocarcinoma status post-gastrojejunostomy and hepaticojejunostomy. She presented to the emergency department with melena, tachycardia, and hemoglobin of 3.8 g/dL. Despite previous hospitalizations for anemia, the bleeding source remained unidentified. Resuscitation with intravenous fluids and blood transfusions was initiated. Contrast-enhanced abdominal CT revealed intraluminal contrast in a small bowel loop at the right pelvis, indicating active GI bleeding. Subsequent esophagogastroduodenoscopy identified multiple arteriovenous malformations in the jejunal afferent and efferent limbs, consistent with BRBNS. In the following days, the patient underwent enteroscopy, which revealed multiple eroded VMs. Endoscopic therapies, including APC and endoclip placement, were performed. However, due to recurrent bleeding and the limited success of these interventions, the patient was scheduled for surgery to resect the affected VMs.
Discussion: Management of BRBNS-related GI bleeding remains a challenge due to the recurrence of lesions and associated complications, including localized intravascular coagulopathy. Endoscopic interventions and systemic therapies, such as sirolimus, have emerged as preferred options, especially for diffuse or recurrent lesions. A systematic review demonstrated clinical success in 86.7% of cases treated with endoscopic resection, banding, or looping. However, adverse events were more frequently associated with systemic therapy. While there is no evidence of malignant transformation of VMs, complications like intestinal infarction, volvulus, or massive GI hemorrhage can be life-threatening, with mortality reported in 2.3% of cases. This case underscores the importance of timely diagnosis and individualized multimodal treatment to mitigate chronic anemia and avoid transfusion dependency.
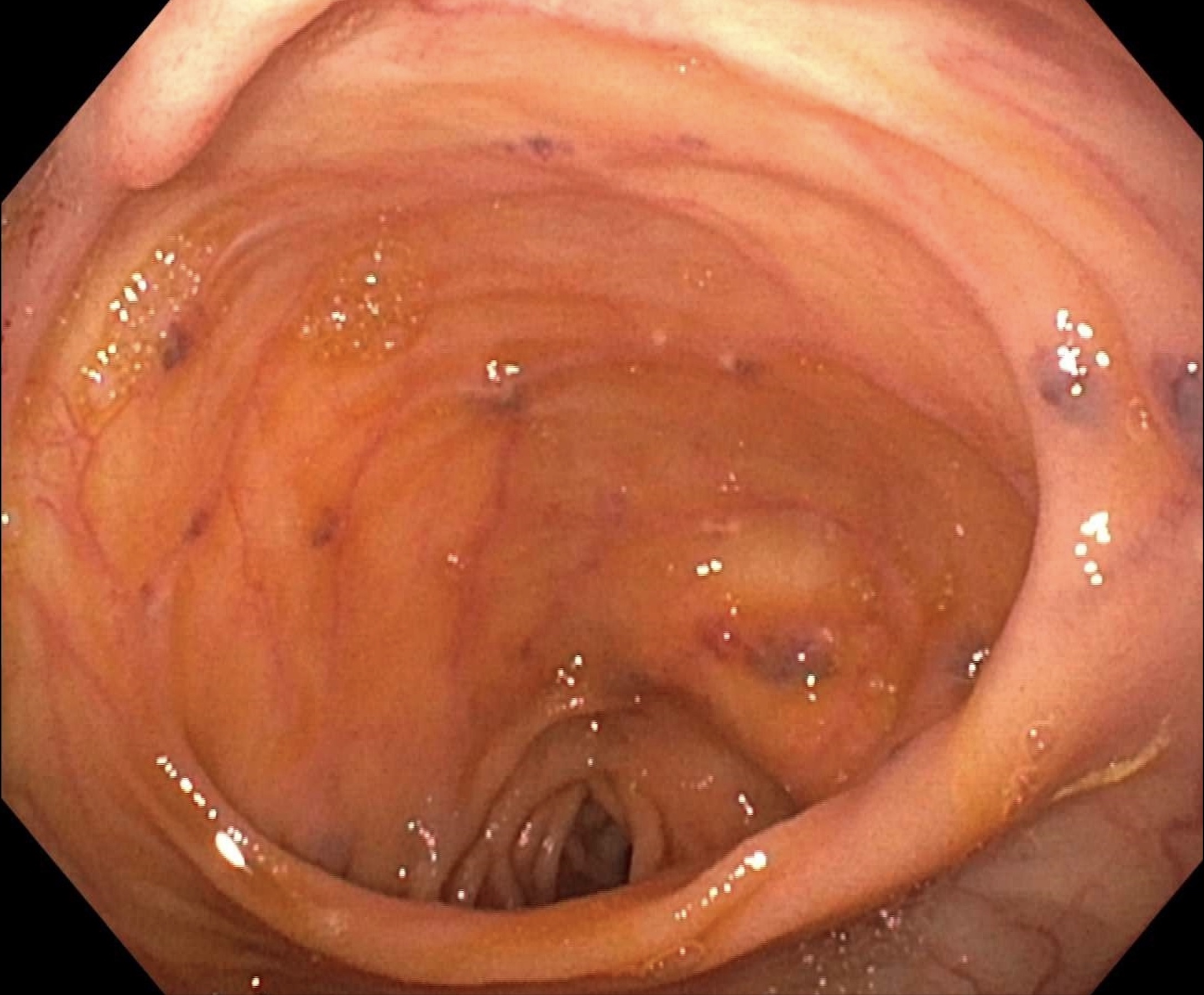
Figure: Endoscopic findings in the small bowel of venous malformations, Blue Rubber Bleb Nevus.
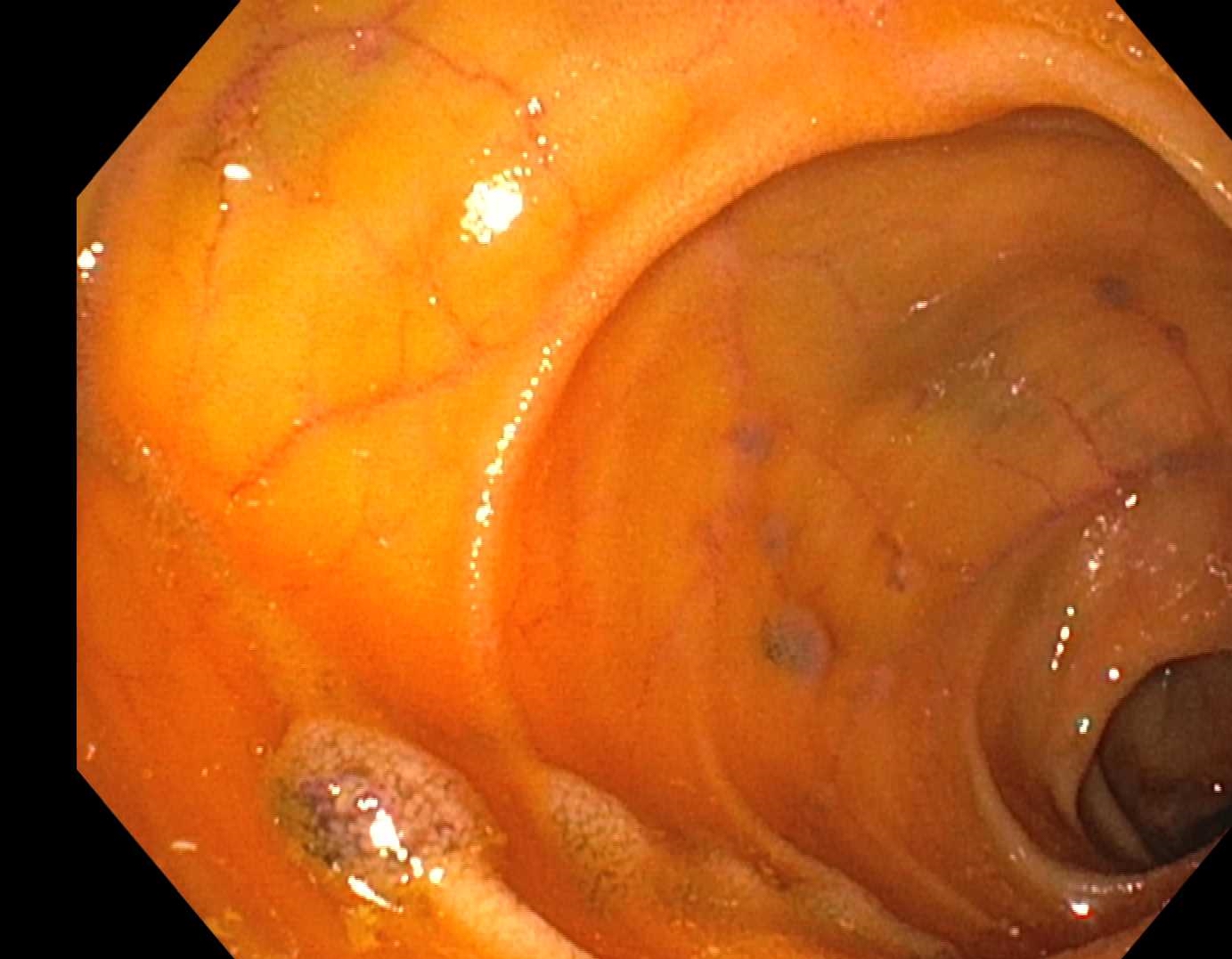
Figure: Endoscopic findings of multiple eroded VMs.
Disclosures:
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Pinky Bai indicated no relevant financial relationships.
Mesay Asfaw indicated no relevant financial relationships.
Amro Abdellatief indicated no relevant financial relationships.
Kristen Miller indicated no relevant financial relationships.
Adeyinka Laiyemo indicated no relevant financial relationships.
Juan C. Santiago-Gonzalez, MD, MSc1, Pinky Bai, MD1, Mesay Asfaw, MD2, Amro Abdellatief, MD1, Kristen Miller, MD3, Adeyinka Laiyemo, MD, MPH4. P5256 - Refractory Anemia Secondary to Acquired Blue Rubber Bleb Nevus Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Howard University Hospital, Washington, DC; 2Howard University, Washington, DC; 3Howard University Hospital | 2041 GEORGIA AVE NW | WASHINGTON, DC, Washington, DC; 4Howard University Hospital | 2041 GEORGIA AVE NW | WASHINGTON, DC, Washington DC, DC
Introduction: Blue Rubber Bleb Nevus Syndrome (BRBNS) is a rare vascular anomaly syndrome characterized by multifocal venous malformations (VMs) predominantly involving the skin and gastrointestinal (GI) tract but can also affect other organs. The prevalence of BRBNS is unknown, with fewer than 200 cases reported globally. Most cases are sporadic, although an autosomal dominant form linked to chromosome 9p has been described. Chronic GI bleeding from VMs leads to anemia, requiring lifelong treatment with iron supplementation or blood transfusions.
Case Description/
Methods: Case of a 88-year-old female with coronary artery disease post-PCI and metastatic duodenal ampullary adenocarcinoma status post-gastrojejunostomy and hepaticojejunostomy. She presented to the emergency department with melena, tachycardia, and hemoglobin of 3.8 g/dL. Despite previous hospitalizations for anemia, the bleeding source remained unidentified. Resuscitation with intravenous fluids and blood transfusions was initiated. Contrast-enhanced abdominal CT revealed intraluminal contrast in a small bowel loop at the right pelvis, indicating active GI bleeding. Subsequent esophagogastroduodenoscopy identified multiple arteriovenous malformations in the jejunal afferent and efferent limbs, consistent with BRBNS. In the following days, the patient underwent enteroscopy, which revealed multiple eroded VMs. Endoscopic therapies, including APC and endoclip placement, were performed. However, due to recurrent bleeding and the limited success of these interventions, the patient was scheduled for surgery to resect the affected VMs.
Discussion: Management of BRBNS-related GI bleeding remains a challenge due to the recurrence of lesions and associated complications, including localized intravascular coagulopathy. Endoscopic interventions and systemic therapies, such as sirolimus, have emerged as preferred options, especially for diffuse or recurrent lesions. A systematic review demonstrated clinical success in 86.7% of cases treated with endoscopic resection, banding, or looping. However, adverse events were more frequently associated with systemic therapy. While there is no evidence of malignant transformation of VMs, complications like intestinal infarction, volvulus, or massive GI hemorrhage can be life-threatening, with mortality reported in 2.3% of cases. This case underscores the importance of timely diagnosis and individualized multimodal treatment to mitigate chronic anemia and avoid transfusion dependency.
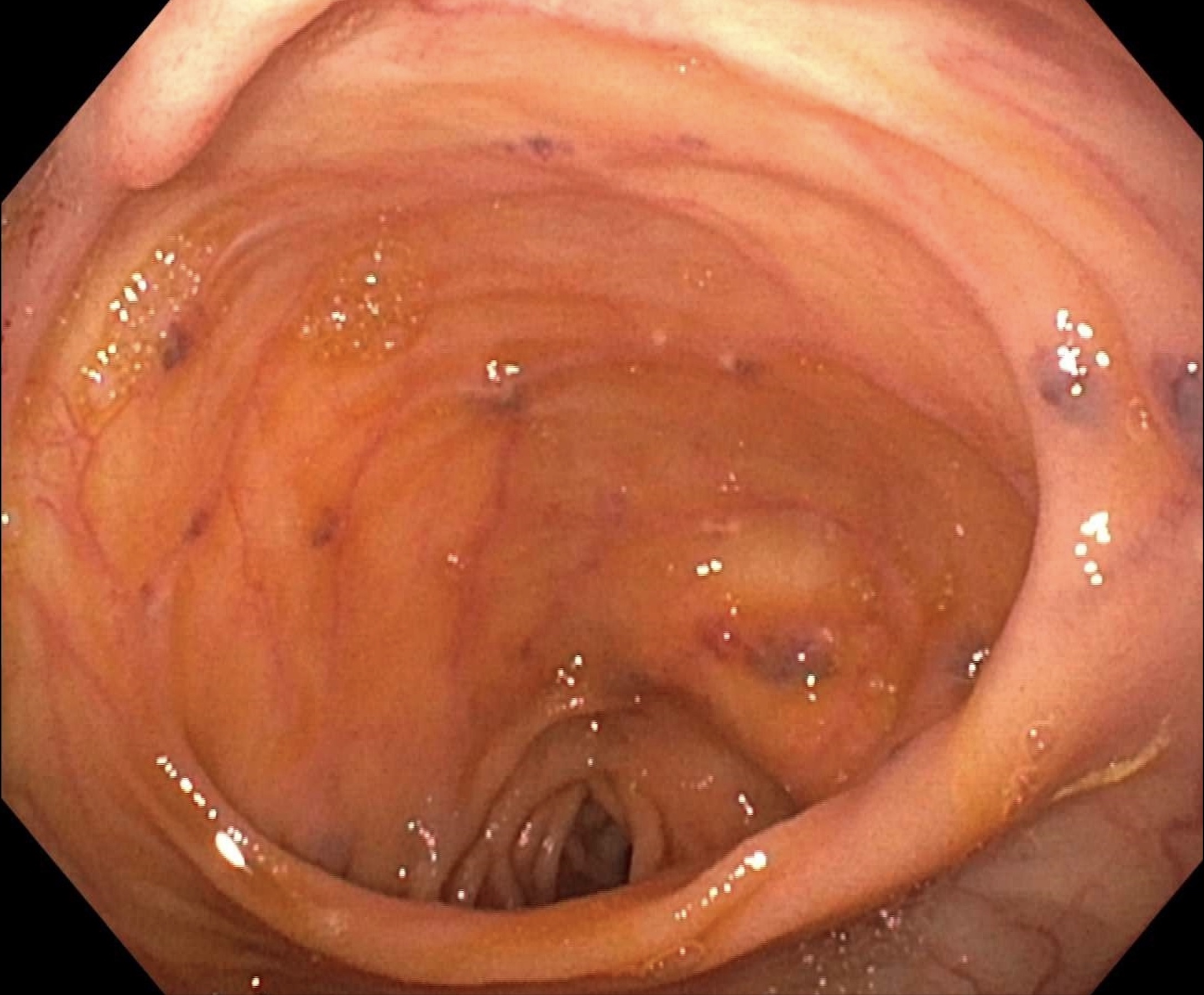
Figure: Endoscopic findings in the small bowel of venous malformations, Blue Rubber Bleb Nevus.
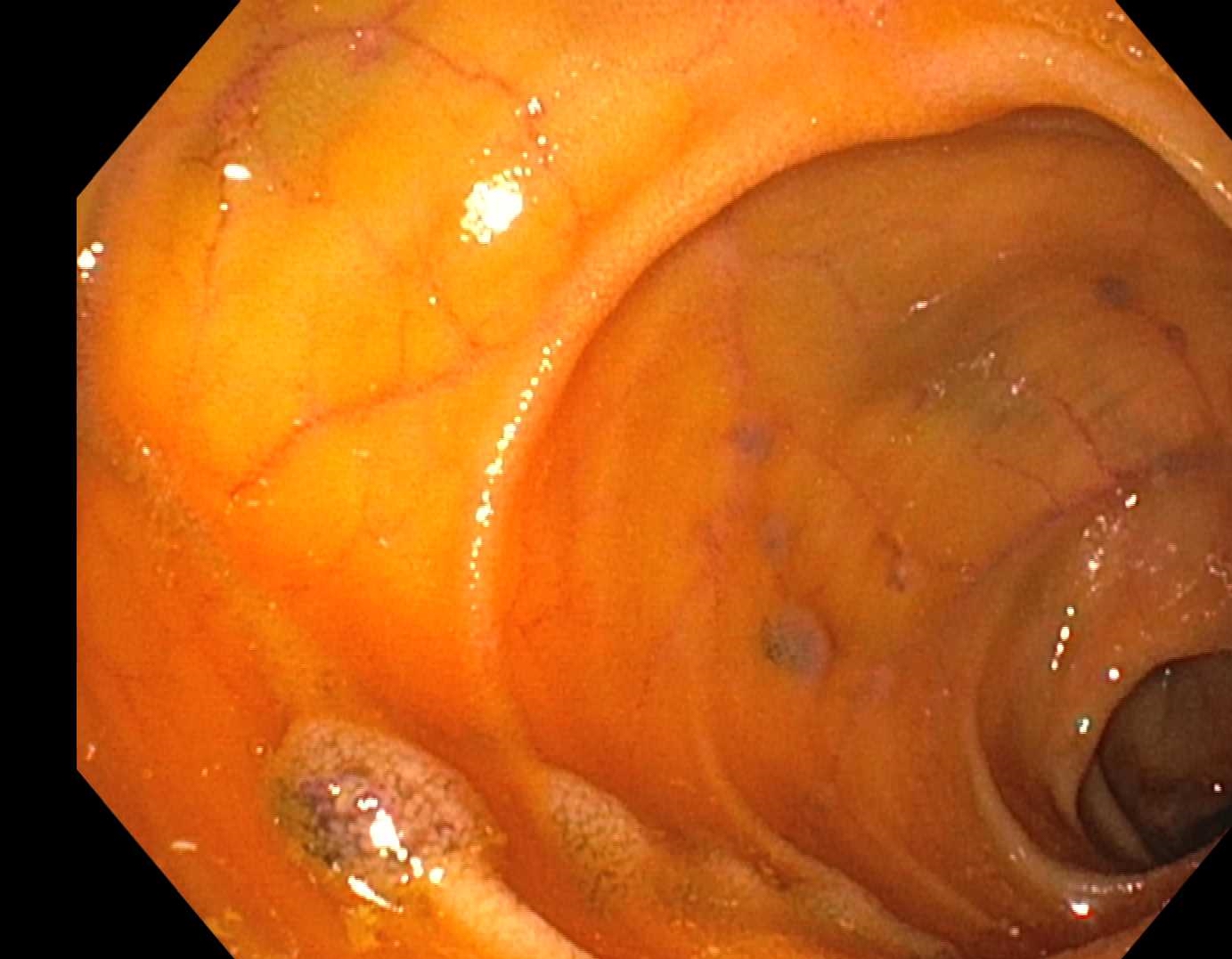
Figure: Endoscopic findings of multiple eroded VMs.
Disclosures:
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Pinky Bai indicated no relevant financial relationships.
Mesay Asfaw indicated no relevant financial relationships.
Amro Abdellatief indicated no relevant financial relationships.
Kristen Miller indicated no relevant financial relationships.
Adeyinka Laiyemo indicated no relevant financial relationships.
Juan C. Santiago-Gonzalez, MD, MSc1, Pinky Bai, MD1, Mesay Asfaw, MD2, Amro Abdellatief, MD1, Kristen Miller, MD3, Adeyinka Laiyemo, MD, MPH4. P5256 - Refractory Anemia Secondary to Acquired Blue Rubber Bleb Nevus Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
