Tuesday Poster Session
Category: GI Bleeding
P5252 - Esophageal Stent as Salvage Therapy for Refractory Esophageal Ulcer Bleeding
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Adam Loeser, MD (he/him/his)
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Adam Loeser, MD1, Holly Greenwald, MD1, Nicholas Wilson, MD1, Nicholas McDonald, MD2
1Temple University Hospital, Philadelphia, PA; 2Temple University, Philadelphia, PA
Introduction: Esophageal stenting is an established salvage therapy for refractory esophageal variceal hemorrhage. Limited data exists for esophageal stenting in non-variceal upper gastrointestinal bleeding. Here we present a case of life-threatening hemorrhage from esophageal ulcer refractory to conventional endoscopic management successfully treated with an esophageal stent.
Case Description/
Methods: A 47-year-old male with AIDS was hospitalized for pneumonia. While admitted, he developed hematemesis complicated by hemorrhagic shock and a life-threatening bleed refractory to crystalloid and vasopressors. Hemoglobin at that time was 3.1 g/dL (14.0 – 17.5 g/dL), down from 9.0 g/dL two days prior. He then developed a cardiac arrest requiring advanced cardiovascular life support and massive transfusion protocol with 8 units of packed red blood cells, 4 units of fresh frozen plasma, and 1 unit of platelets. After stabilization, emergent upper endoscopy (EGD) revealed a large amount of red blood throughout the esophagus, stomach and duodenum preventing visualization. The procedure was aborted, erythromycin given, and repeat EGD hours later revealed a large esophageal ulcer 37 cm from the incisors with an actively bleeding vessel. Bipolar electrocoagulation and through-the-scope clips were attempted without hemostasis. Injected epinephrine slowed the bleeding without achieving hemostasis. Given poor surrounding tissue integrity, an over-the-scope clip was felt to not be a safe option. Hemostatic powder was applied with cessation of bleeding, however while observing the area bleeding recurred within minutes. The decision was then made to place a fully covered self-expandable metal stent across the area of bleeding which was secured using an endoscopic suturing system. No further bleeding was seen following stent deployment. The patient’s hemoglobin stabilized post-procedure. He was weaned from vasopressor support, extubated, and discharged. He underwent EGD for stent removal 41 days after discharge with no residual defect seen. At last follow-up, 72 days from index EGD, he was in his usual state of health.
Discussion: Esophageal stents are rarely utilized for upper gastrointestinal bleeding, typically in the setting of esophageal variceal hemorrhage. In this case, an esophageal stent was used as salvage therapy for refractory life-threatening hemorrhage when conventional methods had failed. While seldom required, endoscopists can consider this as an option in refractory cases of non-variceal esophageal hemorrhage.
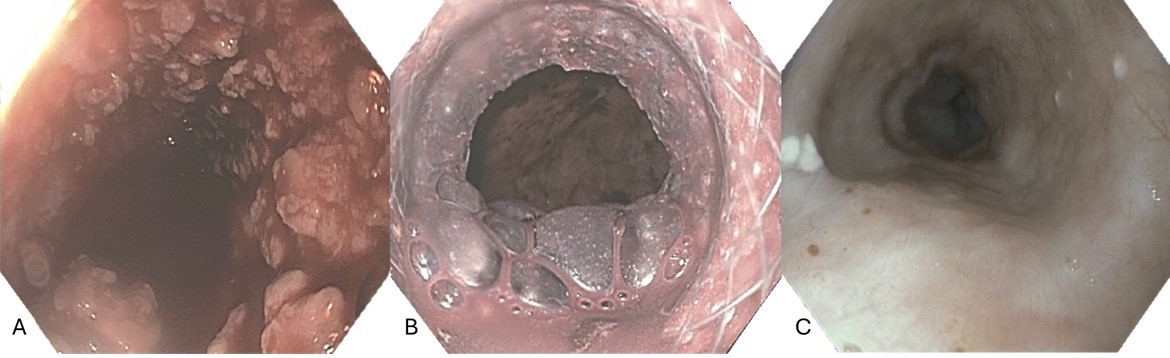
Figure: A) Initial endoscopic view of esophagus with active bleeding. B) Esophagus and gastroesophageal junction after stent deployment. C) Esophagus after stent removal.
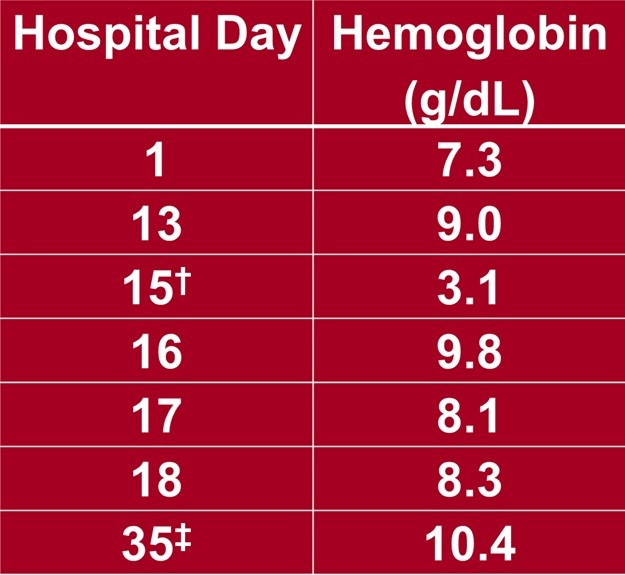
Figure: Hemoglobin trend for patient throughout hospitalization.
†Day of cardiac arrest and EGD with stent placed
‡ Day of discharge from hospital
Disclosures:
Adam Loeser indicated no relevant financial relationships.
Holly Greenwald indicated no relevant financial relationships.
Nicholas Wilson indicated no relevant financial relationships.
Nicholas McDonald indicated no relevant financial relationships.
Adam Loeser, MD1, Holly Greenwald, MD1, Nicholas Wilson, MD1, Nicholas McDonald, MD2. P5252 - Esophageal Stent as Salvage Therapy for Refractory Esophageal Ulcer Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Temple University Hospital, Philadelphia, PA; 2Temple University, Philadelphia, PA
Introduction: Esophageal stenting is an established salvage therapy for refractory esophageal variceal hemorrhage. Limited data exists for esophageal stenting in non-variceal upper gastrointestinal bleeding. Here we present a case of life-threatening hemorrhage from esophageal ulcer refractory to conventional endoscopic management successfully treated with an esophageal stent.
Case Description/
Methods: A 47-year-old male with AIDS was hospitalized for pneumonia. While admitted, he developed hematemesis complicated by hemorrhagic shock and a life-threatening bleed refractory to crystalloid and vasopressors. Hemoglobin at that time was 3.1 g/dL (14.0 – 17.5 g/dL), down from 9.0 g/dL two days prior. He then developed a cardiac arrest requiring advanced cardiovascular life support and massive transfusion protocol with 8 units of packed red blood cells, 4 units of fresh frozen plasma, and 1 unit of platelets. After stabilization, emergent upper endoscopy (EGD) revealed a large amount of red blood throughout the esophagus, stomach and duodenum preventing visualization. The procedure was aborted, erythromycin given, and repeat EGD hours later revealed a large esophageal ulcer 37 cm from the incisors with an actively bleeding vessel. Bipolar electrocoagulation and through-the-scope clips were attempted without hemostasis. Injected epinephrine slowed the bleeding without achieving hemostasis. Given poor surrounding tissue integrity, an over-the-scope clip was felt to not be a safe option. Hemostatic powder was applied with cessation of bleeding, however while observing the area bleeding recurred within minutes. The decision was then made to place a fully covered self-expandable metal stent across the area of bleeding which was secured using an endoscopic suturing system. No further bleeding was seen following stent deployment. The patient’s hemoglobin stabilized post-procedure. He was weaned from vasopressor support, extubated, and discharged. He underwent EGD for stent removal 41 days after discharge with no residual defect seen. At last follow-up, 72 days from index EGD, he was in his usual state of health.
Discussion: Esophageal stents are rarely utilized for upper gastrointestinal bleeding, typically in the setting of esophageal variceal hemorrhage. In this case, an esophageal stent was used as salvage therapy for refractory life-threatening hemorrhage when conventional methods had failed. While seldom required, endoscopists can consider this as an option in refractory cases of non-variceal esophageal hemorrhage.
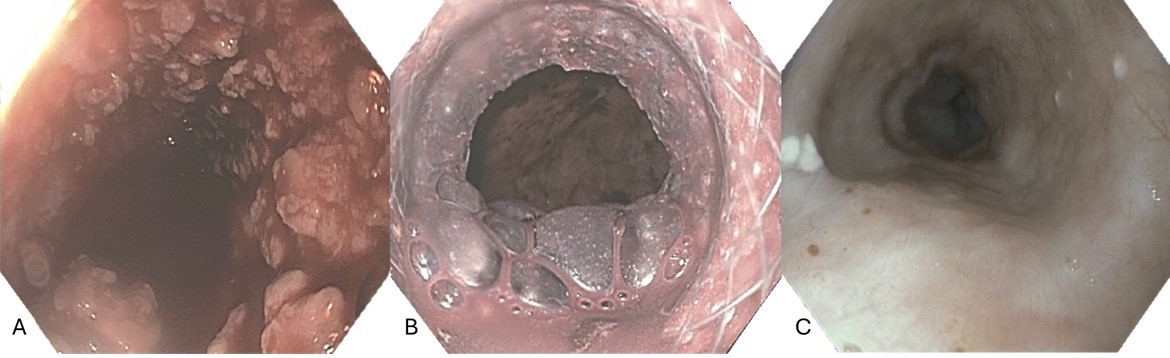
Figure: A) Initial endoscopic view of esophagus with active bleeding. B) Esophagus and gastroesophageal junction after stent deployment. C) Esophagus after stent removal.
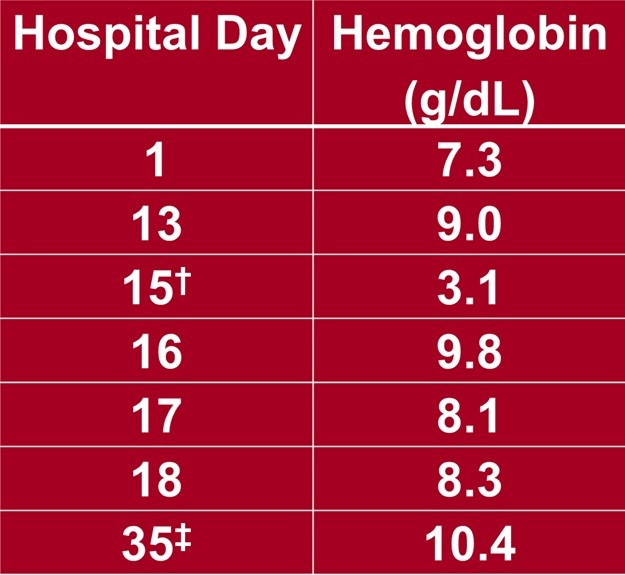
Figure: Hemoglobin trend for patient throughout hospitalization.
†Day of cardiac arrest and EGD with stent placed
‡ Day of discharge from hospital
Disclosures:
Adam Loeser indicated no relevant financial relationships.
Holly Greenwald indicated no relevant financial relationships.
Nicholas Wilson indicated no relevant financial relationships.
Nicholas McDonald indicated no relevant financial relationships.
Adam Loeser, MD1, Holly Greenwald, MD1, Nicholas Wilson, MD1, Nicholas McDonald, MD2. P5252 - Esophageal Stent as Salvage Therapy for Refractory Esophageal Ulcer Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
