Tuesday Poster Session
Category: GI Bleeding
P5249 - Symptomatic Meckel’s Diverticulum: An Overlooked Cause of Terminal Ileal Bleeding in Octogenarians
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Sneh Sonaiya, MD, MPH, MBA
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Sneh Sonaiya, MD, MPH, MBA1, Preet Patel, MD2, Jose Aponte-Pieras, MD1
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV
Introduction: Meckel’s diverticulum (MD), a congenital diverticulum resulting from incomplete vitelline duct involution, affects approximately 2% of the population. While bleeding is a well-recognized presentation in children, symptomatic MD in adults is uncommon and often difficult to diagnose. In adults, bleeding occurs in only 11.8% of MD cases. Terminal ileal diverticula, including both acquired pseudodiverticula and congenital MD, are rare causes of lower GI bleeding in adults. Differentiating MD from other ileal diverticula is challenging without confirmatory imaging or histology. We present a case of terminal ileal bleeding, likely due to symptomatic MD, that was managed endoscopically, highlighting the importance of thorough ileal evaluation in cases of obscure GI bleeding.
Case Description/
Methods: An 84-year-old female with HIV and stage IV CKD presented with 1–2 days of painless bright red blood per rectum and presyncope. She was hemodynamically stable on arrival, with hemoglobin of 7.6 g/dL on arrival that improved to 8.6 g/dL post-transfusion. Non-contrast CT abdomen/pelvis showed sigmoid diverticulosis without diverticulitis. EGD revealed a Schatzki ring and mild gastropathy but no active bleeding. Colonoscopy showed diffuse colonic diverticulosis and an actively bleeding diverticulum in the terminal ileum. Hemostasis was achieved with APC, and a hemoclip was placed for site demarcation. Biopsies taken distal to the diverticulum revealed mild ileitis with superficial ulceration, without dysplasia or malignancy.
Discussion: Although MD is typically diagnosed in children, it can present later in life with bleeding, inflammation, or obstruction. In adults, bleeding occurs in a minority of cases and may result from ulceration due to ectopic gastric mucosa. In this case, the presence of active terminal ileal bleeding, ulceration, and inflammation was more suggestive of symptomatic MD than an acquired pseudodiverticulum, which rarely presents with all three features simultaneously. However, definitive diagnosis was limited by the absence of Meckel’s scan and lack of histologic confirmation via surgical resection or targeted biopsy within the diverticulum due to active bleeding. Histologic confirmation was not pursued due to her comorbidities and lack of rebleeding. This case highlights that lack of recognition of MD in older adults can contribute to missed diagnostic opportunities, and symptomatic MD as a potential cause of terminal ileal bleeding in adults with obscure lower GI hemorrhage.
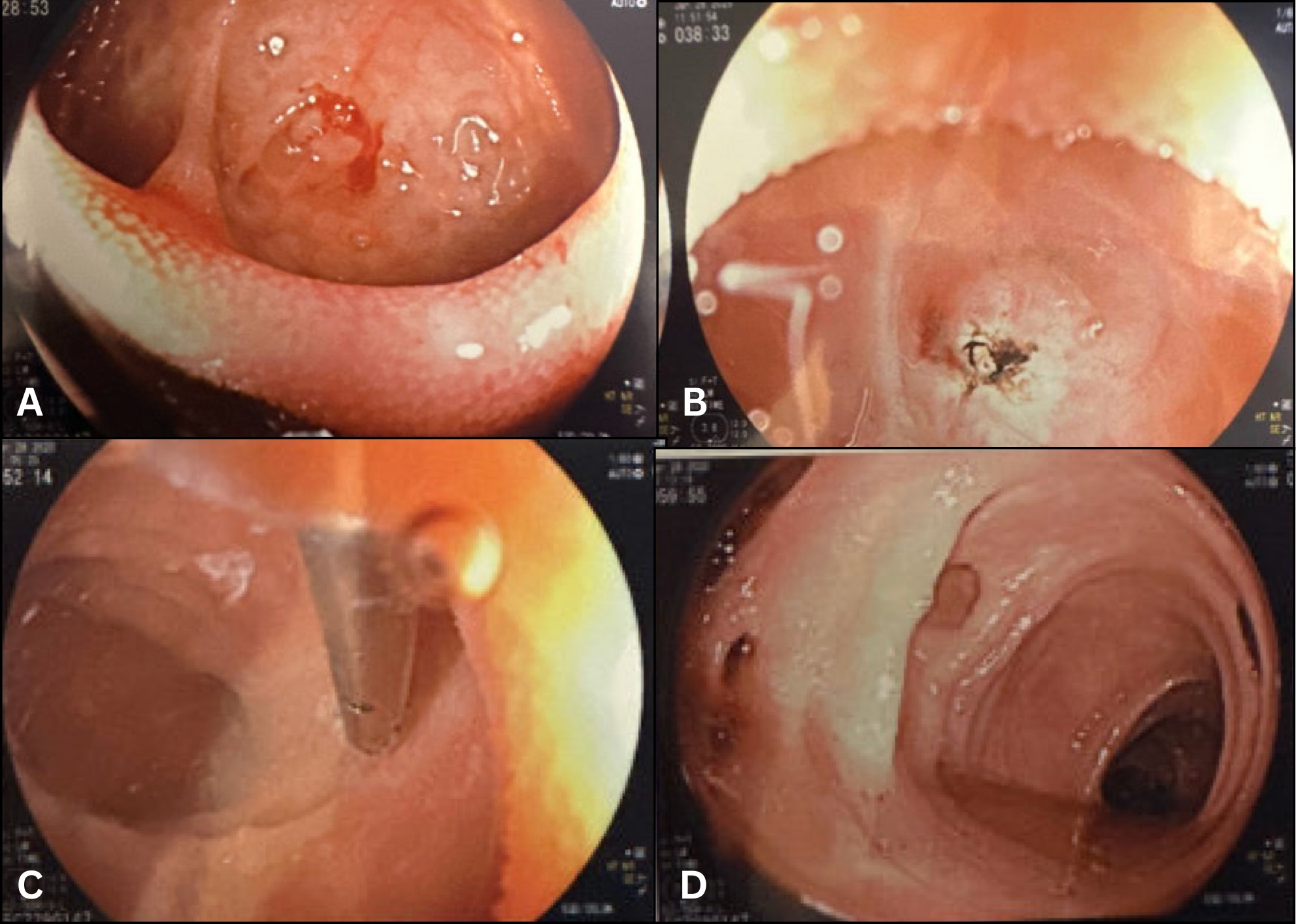
Figure: Figure 1: Endoscopic images demonstrating terminal ileal diverticular hemorrhage: (A) Actively bleeding diverticulum identified in the terminal ileum during colonoscopy. (B) Post-hemostasis appearance following application of argon plasma coagulation (APC). (C) Deployment of a hemoclip adjacent to the treated site for future localization. (D) Diffuse pan-colonic diverticulosis.
Disclosures:
Sneh Sonaiya indicated no relevant financial relationships.
Preet Patel indicated no relevant financial relationships.
Jose Aponte-Pieras indicated no relevant financial relationships.
Sneh Sonaiya, MD, MPH, MBA1, Preet Patel, MD2, Jose Aponte-Pieras, MD1. P5249 - Symptomatic Meckel’s Diverticulum: An Overlooked Cause of Terminal Ileal Bleeding in Octogenarians, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV
Introduction: Meckel’s diverticulum (MD), a congenital diverticulum resulting from incomplete vitelline duct involution, affects approximately 2% of the population. While bleeding is a well-recognized presentation in children, symptomatic MD in adults is uncommon and often difficult to diagnose. In adults, bleeding occurs in only 11.8% of MD cases. Terminal ileal diverticula, including both acquired pseudodiverticula and congenital MD, are rare causes of lower GI bleeding in adults. Differentiating MD from other ileal diverticula is challenging without confirmatory imaging or histology. We present a case of terminal ileal bleeding, likely due to symptomatic MD, that was managed endoscopically, highlighting the importance of thorough ileal evaluation in cases of obscure GI bleeding.
Case Description/
Methods: An 84-year-old female with HIV and stage IV CKD presented with 1–2 days of painless bright red blood per rectum and presyncope. She was hemodynamically stable on arrival, with hemoglobin of 7.6 g/dL on arrival that improved to 8.6 g/dL post-transfusion. Non-contrast CT abdomen/pelvis showed sigmoid diverticulosis without diverticulitis. EGD revealed a Schatzki ring and mild gastropathy but no active bleeding. Colonoscopy showed diffuse colonic diverticulosis and an actively bleeding diverticulum in the terminal ileum. Hemostasis was achieved with APC, and a hemoclip was placed for site demarcation. Biopsies taken distal to the diverticulum revealed mild ileitis with superficial ulceration, without dysplasia or malignancy.
Discussion: Although MD is typically diagnosed in children, it can present later in life with bleeding, inflammation, or obstruction. In adults, bleeding occurs in a minority of cases and may result from ulceration due to ectopic gastric mucosa. In this case, the presence of active terminal ileal bleeding, ulceration, and inflammation was more suggestive of symptomatic MD than an acquired pseudodiverticulum, which rarely presents with all three features simultaneously. However, definitive diagnosis was limited by the absence of Meckel’s scan and lack of histologic confirmation via surgical resection or targeted biopsy within the diverticulum due to active bleeding. Histologic confirmation was not pursued due to her comorbidities and lack of rebleeding. This case highlights that lack of recognition of MD in older adults can contribute to missed diagnostic opportunities, and symptomatic MD as a potential cause of terminal ileal bleeding in adults with obscure lower GI hemorrhage.
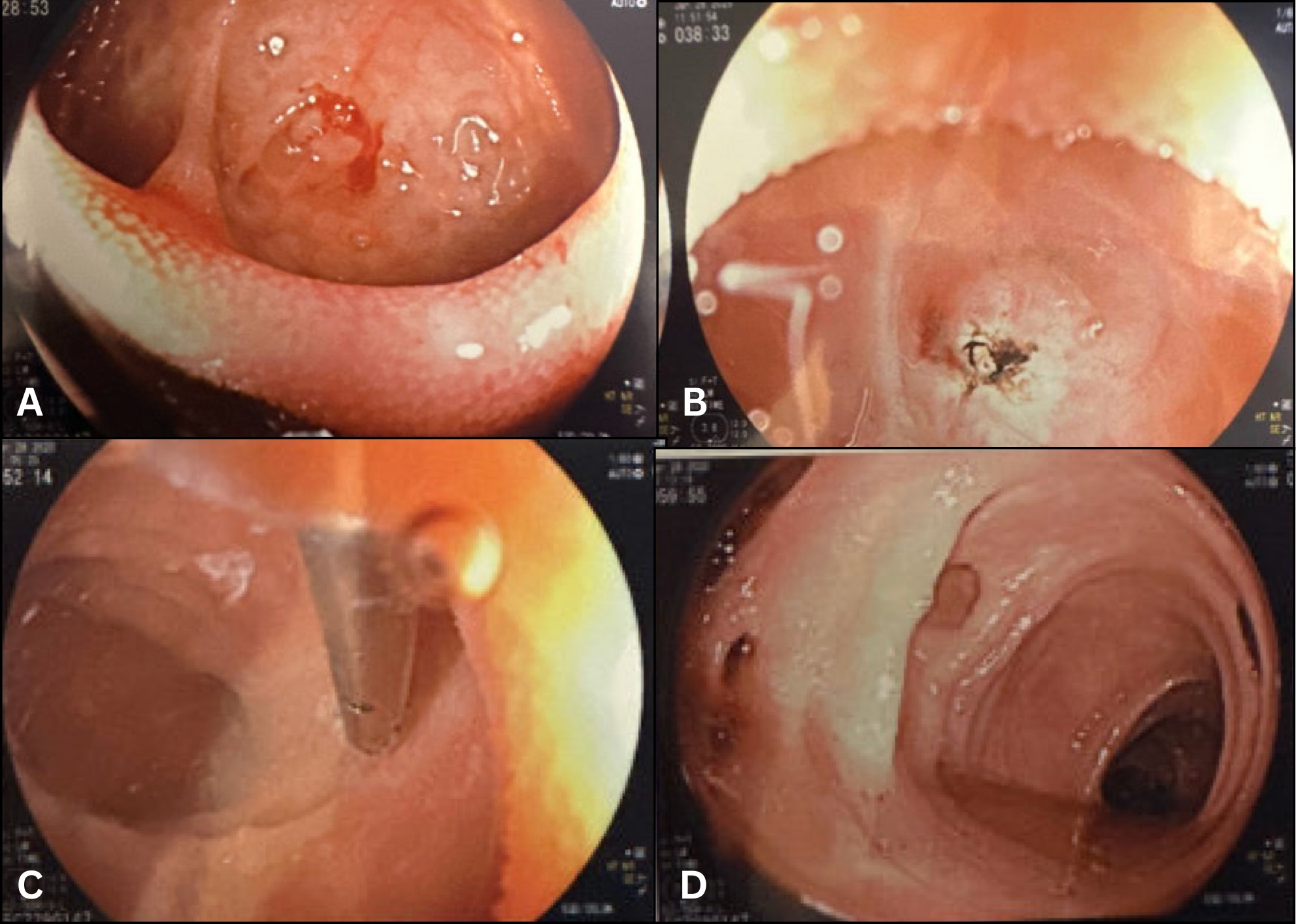
Figure: Figure 1: Endoscopic images demonstrating terminal ileal diverticular hemorrhage: (A) Actively bleeding diverticulum identified in the terminal ileum during colonoscopy. (B) Post-hemostasis appearance following application of argon plasma coagulation (APC). (C) Deployment of a hemoclip adjacent to the treated site for future localization. (D) Diffuse pan-colonic diverticulosis.
Disclosures:
Sneh Sonaiya indicated no relevant financial relationships.
Preet Patel indicated no relevant financial relationships.
Jose Aponte-Pieras indicated no relevant financial relationships.
Sneh Sonaiya, MD, MPH, MBA1, Preet Patel, MD2, Jose Aponte-Pieras, MD1. P5249 - Symptomatic Meckel’s Diverticulum: An Overlooked Cause of Terminal Ileal Bleeding in Octogenarians, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
