Tuesday Poster Session
Category: GI Bleeding
P5247 - A Rare and Fatal Complication of Atrial Fibrillation Ablation: Esophageal-Atrial Fistula – A Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DM
Daniel Mai, MD
University of California Irvine
Orange, CA
Presenting Author(s)
Daniel Mai, MD, Kuangda Shan, MD
University of California Irvine, Orange, CA
Introduction: Esophageal-atrial fistula (EAF) is a rare but fatal complication characterized by an abnormal connection between the left atrium and the esophagus. It most commonly arises following catheter ablation for atrial fibrillation1-2, due to the proximity of the esophagus to the posterior wall of the left atrium which predisposes it to thermal injury during ablation. Other less frequent causes include esophageal cancer, trauma, foreign body ingestion, and infections.
Case Description/
Methods: We report the case of a 57-year-old male with a history of congestive heart failure (LV EF 15%) and atrial fibrillation status post catheter ablation 4 weeks prior, who presented to an outside hospital with signs of sepsis and hypotension. He developed 3 liters of coffee ground emesis with a hemoglobin drop from 14.4 to 9.7 g/dL. He developed cardiac arrest, was resuscitated and intubated. A contrast-enhanced CT chest showed findings concerning for an EAF (Figure 1). Patient was transferred to our center for a higher level of care. Upon arrival, our team performed an emergent EGD which revealed a 2 to 3 cm full thickness defect located 35 cm from incisors around the anterior mid-esophagus with visualization of the pericardium (Figure 2). The cardiothoracic surgical team requested temporizing measure with an esophageal stent placement before definitive management and our team placed a 10-cm fully covered metal stent, from 32 cm to 42 cm from oral incisors covering the defect (Figure 2). Subsequently, the patient’s hospital course was complicated by multiorgan failure as he required transfusions of blood products, IV vasopressors, CRRT, and ECMO. Despite maximal supportive care, he deteriorated clinically and succumbed to the complication.
Discussion: EAF represents a diagnostic challenge. A prior systemic review found an average delay of 4.7 days from symptom onset to hospital presentation. Delayed hospitalization exceeding 14 days post-ablation is associated with an increase in mortality risk (OR 2.4; p = 0.5).3 This case underscores the importance of early diagnosis as catheter ablation becomes more widespread.4-6 Contrast-enhanced CT is a key diagnostic tool for identifying EAF with findings of esophageal wall thickening, mediastinal air, or contrast extravasation.7 Surgical report remains the most effective treatment, though esophageal stenting may serve as a bridge to surgery. Prompt diagnosis and heightened clinical suspicion are essential to improving outcomes in this often fatal condition.
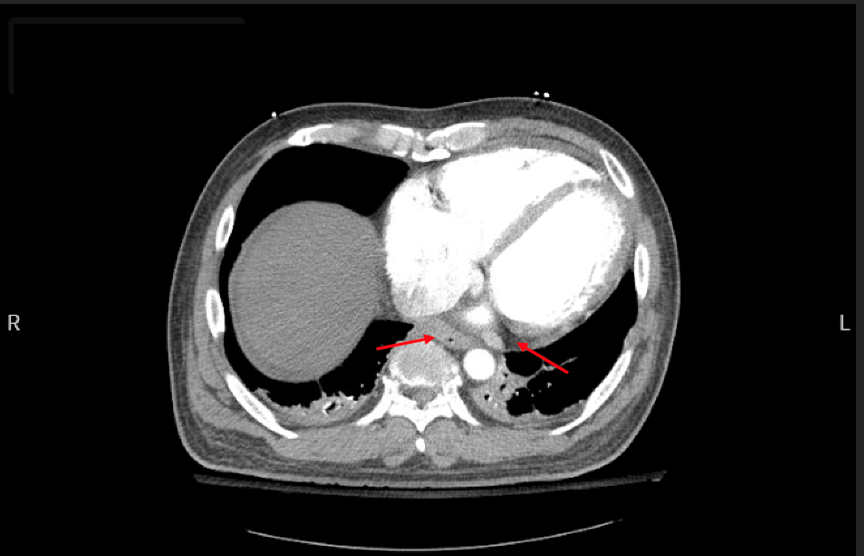
Figure: Figure 1. CT chest with IV contrast done at OSH. Red arrows note esophageal wall thickening (left arrow) juxtaposed to left atrium with epicardial fat stranding (right arrow).
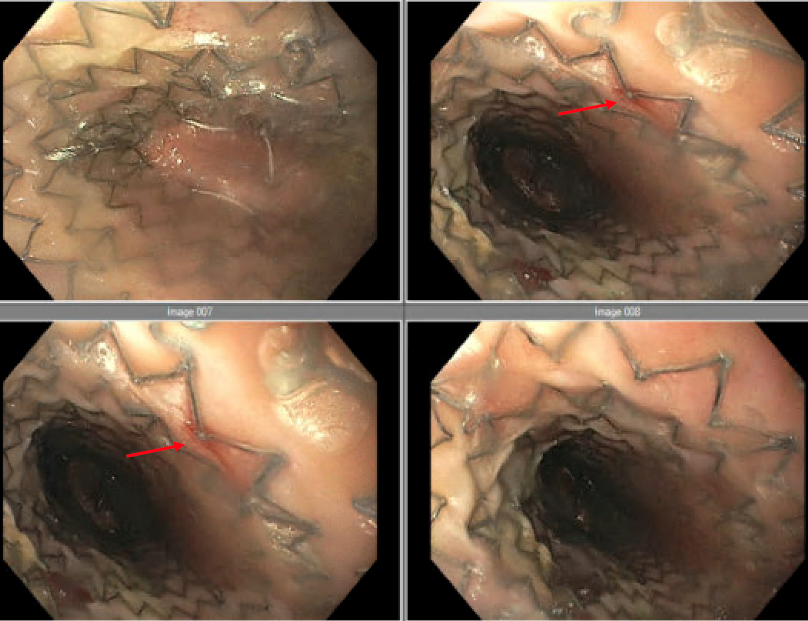
Figure: Figure 2: Endoscopic view of esophageal-atrial fistula (red arrows) located 35 cm from incisors with esophageal stent successfully placed from 32 cm to 42 cm from incisors.
Disclosures:
Daniel Mai indicated no relevant financial relationships.
Kuangda Shan indicated no relevant financial relationships.
Daniel Mai, MD, Kuangda Shan, MD. P5247 - A Rare and Fatal Complication of Atrial Fibrillation Ablation: Esophageal-Atrial Fistula – A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of California Irvine, Orange, CA
Introduction: Esophageal-atrial fistula (EAF) is a rare but fatal complication characterized by an abnormal connection between the left atrium and the esophagus. It most commonly arises following catheter ablation for atrial fibrillation1-2, due to the proximity of the esophagus to the posterior wall of the left atrium which predisposes it to thermal injury during ablation. Other less frequent causes include esophageal cancer, trauma, foreign body ingestion, and infections.
Case Description/
Methods: We report the case of a 57-year-old male with a history of congestive heart failure (LV EF 15%) and atrial fibrillation status post catheter ablation 4 weeks prior, who presented to an outside hospital with signs of sepsis and hypotension. He developed 3 liters of coffee ground emesis with a hemoglobin drop from 14.4 to 9.7 g/dL. He developed cardiac arrest, was resuscitated and intubated. A contrast-enhanced CT chest showed findings concerning for an EAF (Figure 1). Patient was transferred to our center for a higher level of care. Upon arrival, our team performed an emergent EGD which revealed a 2 to 3 cm full thickness defect located 35 cm from incisors around the anterior mid-esophagus with visualization of the pericardium (Figure 2). The cardiothoracic surgical team requested temporizing measure with an esophageal stent placement before definitive management and our team placed a 10-cm fully covered metal stent, from 32 cm to 42 cm from oral incisors covering the defect (Figure 2). Subsequently, the patient’s hospital course was complicated by multiorgan failure as he required transfusions of blood products, IV vasopressors, CRRT, and ECMO. Despite maximal supportive care, he deteriorated clinically and succumbed to the complication.
Discussion: EAF represents a diagnostic challenge. A prior systemic review found an average delay of 4.7 days from symptom onset to hospital presentation. Delayed hospitalization exceeding 14 days post-ablation is associated with an increase in mortality risk (OR 2.4; p = 0.5).3 This case underscores the importance of early diagnosis as catheter ablation becomes more widespread.4-6 Contrast-enhanced CT is a key diagnostic tool for identifying EAF with findings of esophageal wall thickening, mediastinal air, or contrast extravasation.7 Surgical report remains the most effective treatment, though esophageal stenting may serve as a bridge to surgery. Prompt diagnosis and heightened clinical suspicion are essential to improving outcomes in this often fatal condition.
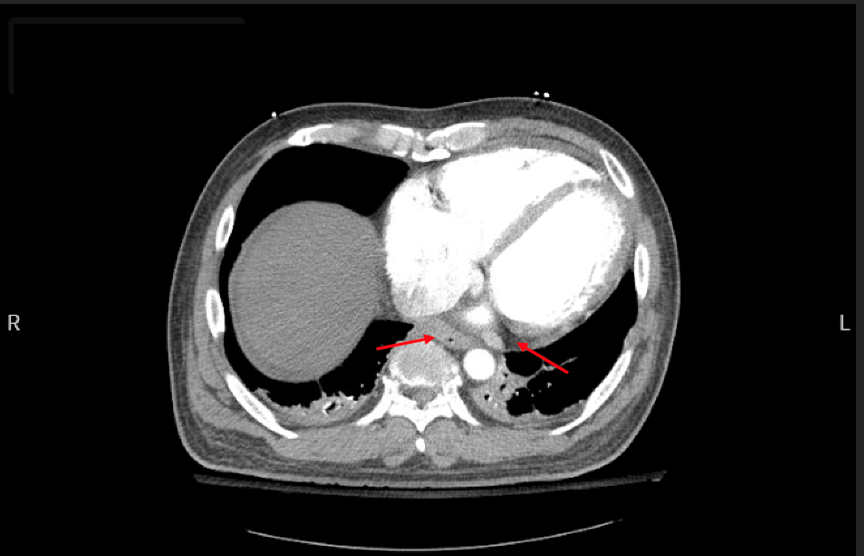
Figure: Figure 1. CT chest with IV contrast done at OSH. Red arrows note esophageal wall thickening (left arrow) juxtaposed to left atrium with epicardial fat stranding (right arrow).
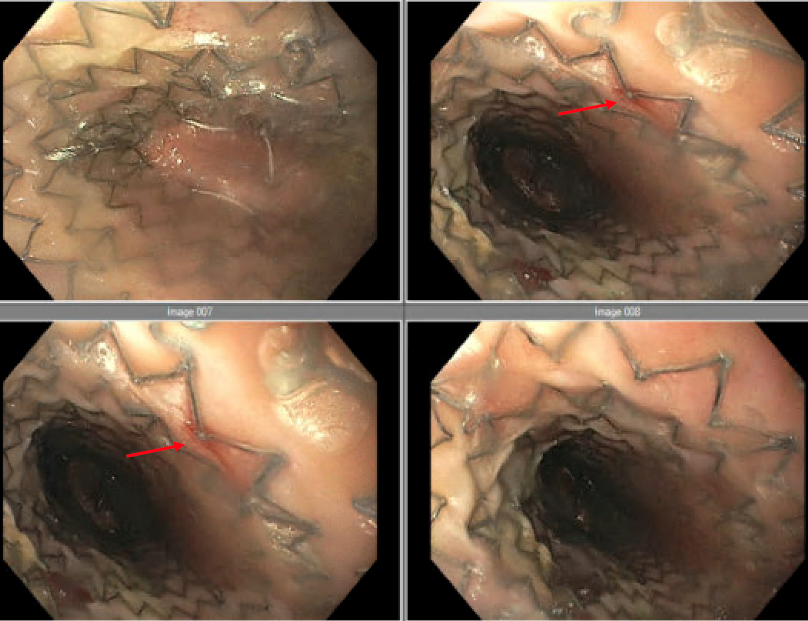
Figure: Figure 2: Endoscopic view of esophageal-atrial fistula (red arrows) located 35 cm from incisors with esophageal stent successfully placed from 32 cm to 42 cm from incisors.
Disclosures:
Daniel Mai indicated no relevant financial relationships.
Kuangda Shan indicated no relevant financial relationships.
Daniel Mai, MD, Kuangda Shan, MD. P5247 - A Rare and Fatal Complication of Atrial Fibrillation Ablation: Esophageal-Atrial Fistula – A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
