Tuesday Poster Session
Category: GI Bleeding
P5237 - Beyond the Typical GI Bleed: Superior Mesenteric Artery Pseudoaneurysm Causing Hemosuccus Pancreaticus
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alan Gabriel Ortega Macias, MD (he/him/his)
University of New Mexico
Albuquerque, NM
Presenting Author(s)
Alan Gabriel. Ortega Macias, MD1, Udita Gupta, MD2, Pooja Viswanath, DO1, Prithvi Reddy Akepati, MD3, Euriko Torrazza Perez, MD, MSPH1
1University of New Mexico, Albuquerque, NM; 2University of New Mexico Health Sciences Center, Albuquerque, NM; 3University of New Mexico Hospital, Albuquerque, NM
Introduction: Hemosuccus pancreaticus (HP) is a rare but life-threatening cause of upper gastrointestinal bleeding, characterized by hemorrhage into the pancreatic duct and egress of blood through the ampulla of Vater often arising from a visceral artery pseudoaneurysm (VAPAs) of the peripancreatic arteries in the setting of acute or chronic pancreatitis, trauma, or surgery. Splenic artery pseudoaneurysm is the leading cause of this condition, superior mesenteric artery (SMA) is the rarest subtype, with an estimated incidence of 0.01%. We present a challenging case of gastrointestinal bleeding due to an SMA pseudoaneurysm in a patient with necrotizing pancreatitis and multiple vascular complications.
Case Description/
Methods: A 59-year-old woman with a recent episode of alcohol-associated pancreatitis complicated by pseudocyst formation was admitted for stroke due to M1 occlusion, status post thrombectomy. Her hospitalization was further complicated by acute limb ischemia requiring embolectomy and initiation of therapeutic anticoagulation. She then developed melena, hematemesis, and acute anemia (Hgb 11.3 → 6.9 g/dL). EGD revealed a large clot in the second portion of the duodenum and blood oozing from the ampulla, consistent with HP (Fig .1). CT angiography demonstrated necrotizing pancreatitis with expanding peripancreatic collections and a possible SMA pseudoaneurysm. Mesenteric angiography with IR revealed active extravasation from a 1.7 cm pseudoaneurysm in the pancreatic head arising from the distal SMA but it could not be cannulated or embolized (Fig. 2). Stent graft placement was deferred due to anatomical limitations and risk of bowel ischemia. Given prohibitive surgical risk due to her comorbidities, a multidisciplinary team including IR, vascular, and hepatobiliary surgery recommended non-operative management. Anticoagulation was held due to ongoing GI bleeding despite prior embolectomy. Due to multiple ongoing issues with limited therapeutic options and poor prognosis, her family elected to transition to hospice care.
Discussion: HP, when seen in pancreatitis, happens due to enzymatic injury of the arterial system which may lead to formation and rupture of arterial pseudoaneurysm into the pancreatic duct and subsequent hemorrhage. Endoscopic diagnosis is challenging, with bleeding visible in only 30% of cases; CTA offers superior sensitivity (96%). This case underscores the diagnostic challenge of HP from the relatively rare SMA aneurysm and the complexity of managing life-threatening GI bleeding.
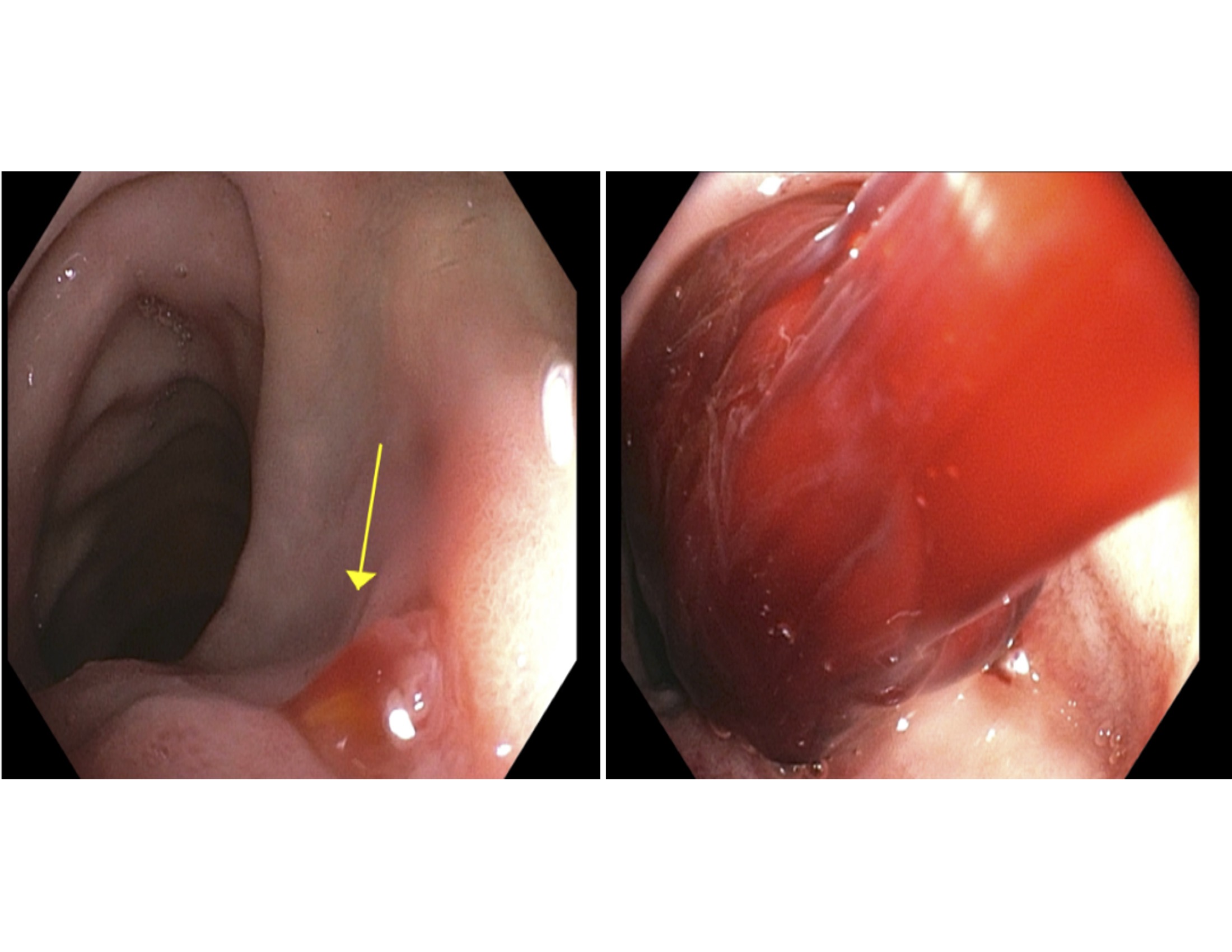
Figure: Fig 1. EGD showing blood oozing from major ampulla.
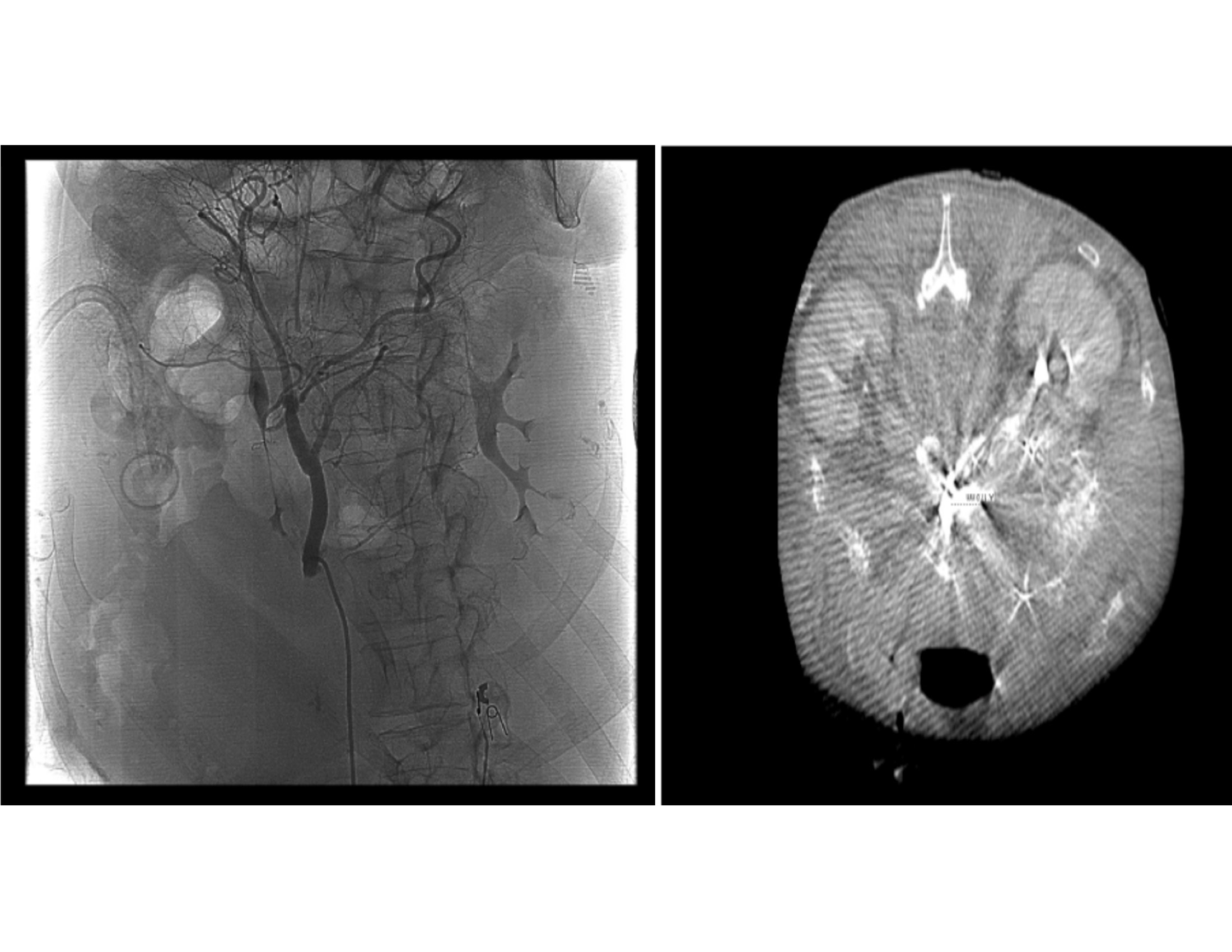
Figure: Fig 2. CT angiography and fluoroscopy with evidence of a 17 mm superior mesenteric artery pseudoaneurysm.
Disclosures:
Alan Ortega Macias indicated no relevant financial relationships.
Udita Gupta indicated no relevant financial relationships.
Pooja Viswanath indicated no relevant financial relationships.
Prithvi Reddy Akepati indicated no relevant financial relationships.
Euriko Torrazza Perez indicated no relevant financial relationships.
Alan Gabriel. Ortega Macias, MD1, Udita Gupta, MD2, Pooja Viswanath, DO1, Prithvi Reddy Akepati, MD3, Euriko Torrazza Perez, MD, MSPH1. P5237 - Beyond the Typical GI Bleed: Superior Mesenteric Artery Pseudoaneurysm Causing Hemosuccus Pancreaticus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of New Mexico, Albuquerque, NM; 2University of New Mexico Health Sciences Center, Albuquerque, NM; 3University of New Mexico Hospital, Albuquerque, NM
Introduction: Hemosuccus pancreaticus (HP) is a rare but life-threatening cause of upper gastrointestinal bleeding, characterized by hemorrhage into the pancreatic duct and egress of blood through the ampulla of Vater often arising from a visceral artery pseudoaneurysm (VAPAs) of the peripancreatic arteries in the setting of acute or chronic pancreatitis, trauma, or surgery. Splenic artery pseudoaneurysm is the leading cause of this condition, superior mesenteric artery (SMA) is the rarest subtype, with an estimated incidence of 0.01%. We present a challenging case of gastrointestinal bleeding due to an SMA pseudoaneurysm in a patient with necrotizing pancreatitis and multiple vascular complications.
Case Description/
Methods: A 59-year-old woman with a recent episode of alcohol-associated pancreatitis complicated by pseudocyst formation was admitted for stroke due to M1 occlusion, status post thrombectomy. Her hospitalization was further complicated by acute limb ischemia requiring embolectomy and initiation of therapeutic anticoagulation. She then developed melena, hematemesis, and acute anemia (Hgb 11.3 → 6.9 g/dL). EGD revealed a large clot in the second portion of the duodenum and blood oozing from the ampulla, consistent with HP (Fig .1). CT angiography demonstrated necrotizing pancreatitis with expanding peripancreatic collections and a possible SMA pseudoaneurysm. Mesenteric angiography with IR revealed active extravasation from a 1.7 cm pseudoaneurysm in the pancreatic head arising from the distal SMA but it could not be cannulated or embolized (Fig. 2). Stent graft placement was deferred due to anatomical limitations and risk of bowel ischemia. Given prohibitive surgical risk due to her comorbidities, a multidisciplinary team including IR, vascular, and hepatobiliary surgery recommended non-operative management. Anticoagulation was held due to ongoing GI bleeding despite prior embolectomy. Due to multiple ongoing issues with limited therapeutic options and poor prognosis, her family elected to transition to hospice care.
Discussion: HP, when seen in pancreatitis, happens due to enzymatic injury of the arterial system which may lead to formation and rupture of arterial pseudoaneurysm into the pancreatic duct and subsequent hemorrhage. Endoscopic diagnosis is challenging, with bleeding visible in only 30% of cases; CTA offers superior sensitivity (96%). This case underscores the diagnostic challenge of HP from the relatively rare SMA aneurysm and the complexity of managing life-threatening GI bleeding.
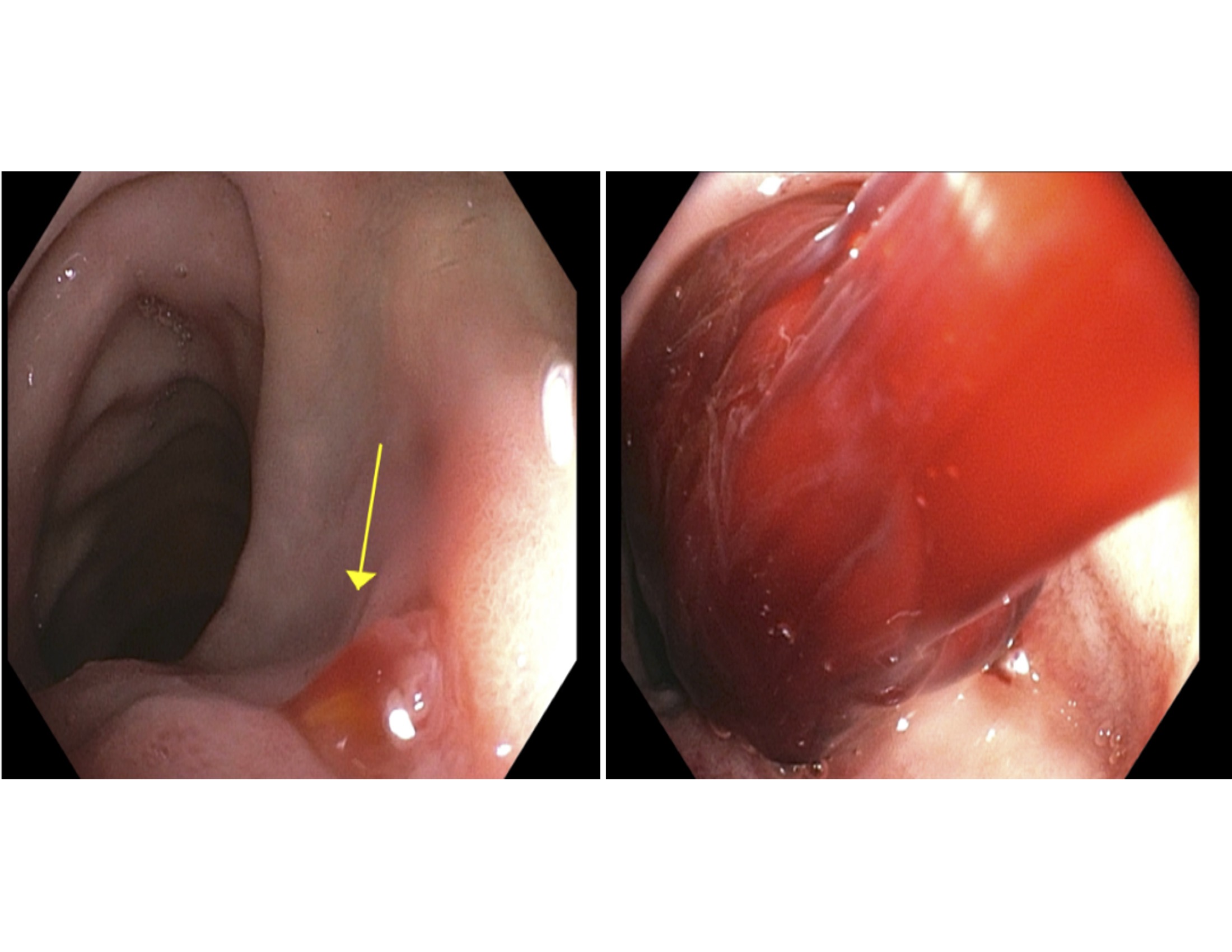
Figure: Fig 1. EGD showing blood oozing from major ampulla.
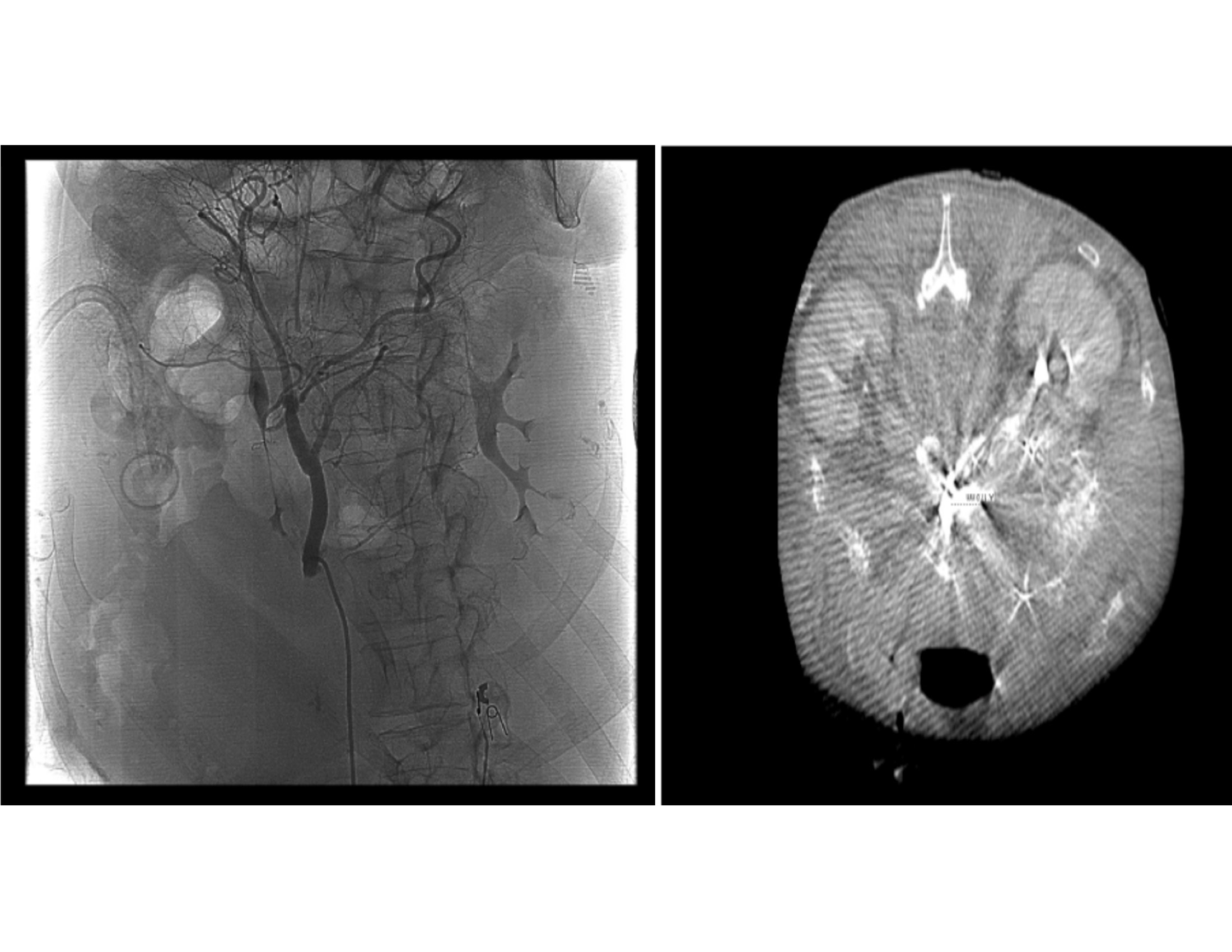
Figure: Fig 2. CT angiography and fluoroscopy with evidence of a 17 mm superior mesenteric artery pseudoaneurysm.
Disclosures:
Alan Ortega Macias indicated no relevant financial relationships.
Udita Gupta indicated no relevant financial relationships.
Pooja Viswanath indicated no relevant financial relationships.
Prithvi Reddy Akepati indicated no relevant financial relationships.
Euriko Torrazza Perez indicated no relevant financial relationships.
Alan Gabriel. Ortega Macias, MD1, Udita Gupta, MD2, Pooja Viswanath, DO1, Prithvi Reddy Akepati, MD3, Euriko Torrazza Perez, MD, MSPH1. P5237 - Beyond the Typical GI Bleed: Superior Mesenteric Artery Pseudoaneurysm Causing Hemosuccus Pancreaticus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
