Tuesday Poster Session
Category: GI Bleeding
P5234 - Isolated Bleeding From a Duodenal Varix: A Rare and Unusual Presentation in Newly Diagnosed Cirrhosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AC
Aneesa Chowdhury, MD (she/her/hers)
UC Irvine Digestive Health Institute
Orange, CA
Presenting Author(s)
Aneesa Chowdhury, MD1, Christopher Paiji, MD2
1UC Irvine Digestive Health Institute, Orange, CA; 2University of California Irvine Digestive Health Institute, Orange, CA
Introduction: Duodenal varices are an uncommon cause of gastrointestinal bleeding, accounting for ≤5% of all variceal bleeding, and are most often seen in the context of prior abdominal surgery or prehepatic portal hypertension. In cirrhosis, varices most commonly develop in the esophagus and proximal stomach due to the typical patterns of portosystemic collateral formation. Isolated duodenal varices without the presence of esophagogastric varices are exceedingly rare and may delay prompt recognition of a bleeding source.
Case Description/
Methods: A 83-year-old female without a known history of liver disease presented to the hospital for multiple episodes of coffee-ground emesis. She had no history of alcohol use, prior surgery, or anticoagulation use. She was hypotensive with hemoglobin of 6.6 on arrival. Bedside rectal exam demonstrated melena.
CT angiography abdomen and pelvis with liver cirrhosis with sequela of portal hypertension and diffuse hyperenhancement of a segment of anterior abdominal small bowel with differentials including nonspecific enteritis or small bowel vascular lesion. Upper endoscopy revealed a normal esophagus without esophageal varices. Stomach had copious amounts of dark red blood. After irrigating and suctioning there was no obvious source of bleed identified in the stomach. No gastric varices were seen. Duodenal exam with red blood and a large duodenal varix was seen in the duodenal sweep, which was near the ampulla but did not involve it (Figure 1a). There was noted active spurting from the varix. A hemoclip was placed with hemostasis achieved (Figure 1b).
Patient was then sent to Interventional Radiology for coil-assisted retrograde transvenous obliteration of the varix (Figure 2). Hemoglobin remained stable the remainder of the hospital stay without additional signs of bleed.
Discussion: This case demonstrates a unique presentation of a newly diagnosed cirrhotic patient with isolated duodenal varices without the more common esophageal or gastric varices seen in portal hypertension. This atypical presentation underscores the diagnostic challenge posed by ectopic varices and the need for prompt and thorough endoscopic evaluation. The management of duodenal varices is not standardized but may include endoscopic, radiologic, or surgical interventions, requiring a multidisciplinary approach.
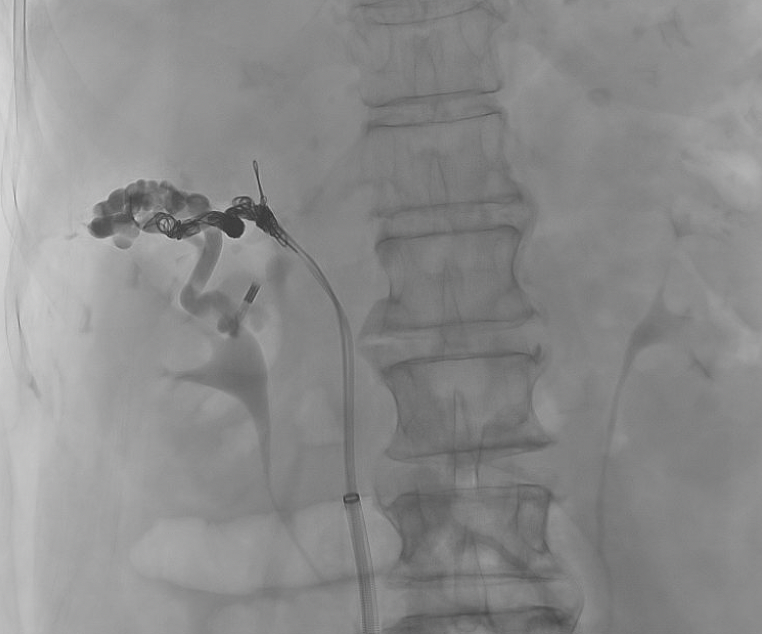
Figure: Figure 1. Endoscopic findings of duodenal varix a) active spurting b) hemostasis following hemoclip placement
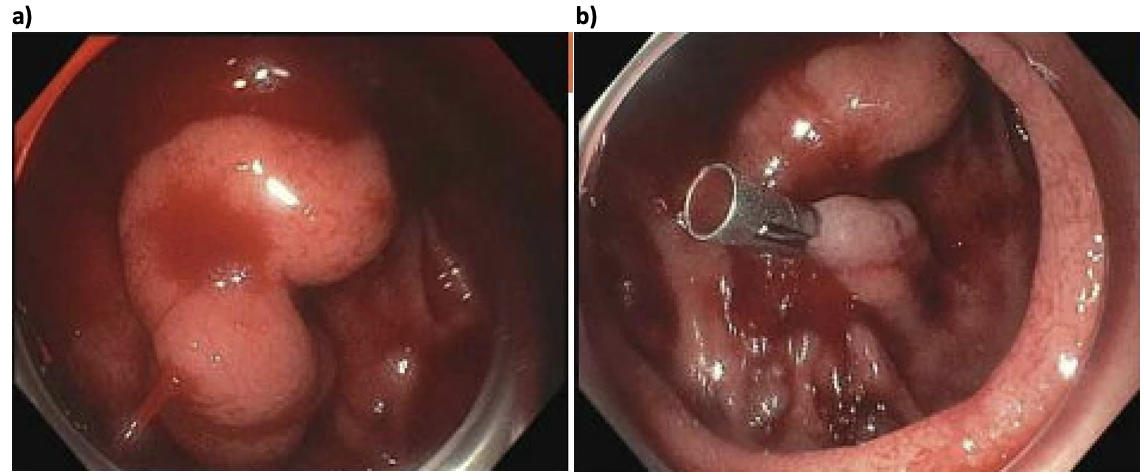
Figure: Figure 2. Coil-assisted retrograde transvenous obliteration of the duodenal varix
Disclosures:
Aneesa Chowdhury indicated no relevant financial relationships.
Christopher Paiji indicated no relevant financial relationships.
Aneesa Chowdhury, MD1, Christopher Paiji, MD2. P5234 - Isolated Bleeding From a Duodenal Varix: A Rare and Unusual Presentation in Newly Diagnosed Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1UC Irvine Digestive Health Institute, Orange, CA; 2University of California Irvine Digestive Health Institute, Orange, CA
Introduction: Duodenal varices are an uncommon cause of gastrointestinal bleeding, accounting for ≤5% of all variceal bleeding, and are most often seen in the context of prior abdominal surgery or prehepatic portal hypertension. In cirrhosis, varices most commonly develop in the esophagus and proximal stomach due to the typical patterns of portosystemic collateral formation. Isolated duodenal varices without the presence of esophagogastric varices are exceedingly rare and may delay prompt recognition of a bleeding source.
Case Description/
Methods: A 83-year-old female without a known history of liver disease presented to the hospital for multiple episodes of coffee-ground emesis. She had no history of alcohol use, prior surgery, or anticoagulation use. She was hypotensive with hemoglobin of 6.6 on arrival. Bedside rectal exam demonstrated melena.
CT angiography abdomen and pelvis with liver cirrhosis with sequela of portal hypertension and diffuse hyperenhancement of a segment of anterior abdominal small bowel with differentials including nonspecific enteritis or small bowel vascular lesion. Upper endoscopy revealed a normal esophagus without esophageal varices. Stomach had copious amounts of dark red blood. After irrigating and suctioning there was no obvious source of bleed identified in the stomach. No gastric varices were seen. Duodenal exam with red blood and a large duodenal varix was seen in the duodenal sweep, which was near the ampulla but did not involve it (Figure 1a). There was noted active spurting from the varix. A hemoclip was placed with hemostasis achieved (Figure 1b).
Patient was then sent to Interventional Radiology for coil-assisted retrograde transvenous obliteration of the varix (Figure 2). Hemoglobin remained stable the remainder of the hospital stay without additional signs of bleed.
Discussion: This case demonstrates a unique presentation of a newly diagnosed cirrhotic patient with isolated duodenal varices without the more common esophageal or gastric varices seen in portal hypertension. This atypical presentation underscores the diagnostic challenge posed by ectopic varices and the need for prompt and thorough endoscopic evaluation. The management of duodenal varices is not standardized but may include endoscopic, radiologic, or surgical interventions, requiring a multidisciplinary approach.
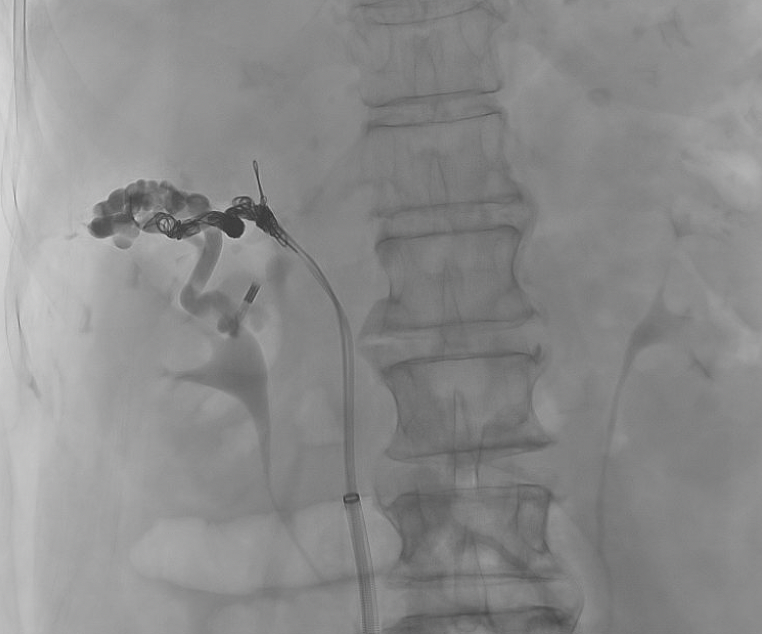
Figure: Figure 1. Endoscopic findings of duodenal varix a) active spurting b) hemostasis following hemoclip placement
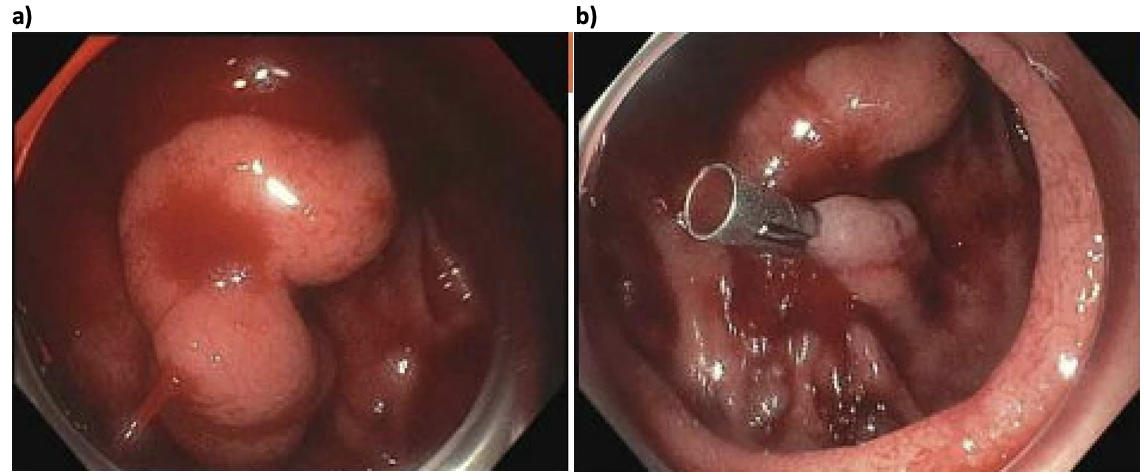
Figure: Figure 2. Coil-assisted retrograde transvenous obliteration of the duodenal varix
Disclosures:
Aneesa Chowdhury indicated no relevant financial relationships.
Christopher Paiji indicated no relevant financial relationships.
Aneesa Chowdhury, MD1, Christopher Paiji, MD2. P5234 - Isolated Bleeding From a Duodenal Varix: A Rare and Unusual Presentation in Newly Diagnosed Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
