Tuesday Poster Session
Category: GI Bleeding
P5232 - Behind Bars, Out of Sight: Catastrophic NSAID-Induced Duodenal Perforation in an Incarcerated Patient
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Muhammad Hassan, MD
Nuvance Health
Poughkeepsie, NY
Presenting Author(s)
Cameron Mitchell, MD1, Muhammad Hassan, MD1, Zana Nikolla, MD2, Elizabeth Williams, DO2
1Nuvance Health, Poughkeepsie, NY; 2Premier Medical Group, Poughkeepsie, NY
Introduction: Nonsteroidal anti-inflammatory drugs (NSAIDs) are widely used for musculoskeletal pain due to their anti-inflammatory and analgesic effects. However, by inhibiting prostaglandin synthesis, NSAIDs compromise the gastrointestinal (GI) mucosal barrier, increasing the risk of mucosal injury, ulceration, bleeding, and perforation. Chronic NSAID use is a well-established risk factor for peptic ulcer disease (PUD), though complications have become increasingly rare due to the accessibility of gastroprotective agents such as proton pump inhibitors (PPIs) and H2 blockers.
Case Description/
Methods: A 28-year-old incarcerated male with no known medical history presented with sudden-onset hematemesis and left upper quadrant abdominal pain. He had been taking naproxen 500 mg twice daily for six months following a metatarsal fracture. On EMS arrival, he was hypotensive (BP 80/40 mmHg), tachycardic (HR 140), and briefly unresponsive. Labs revealed leukocytosis (20.0 × 10⁹/L), hemoglobin 10.1 g/dL, elevated BUN/Cr ratio (35.7), and lactate 2.7 mmol/L. His Glasgow-Blatchford Bleeding Score was 11.
CT angiography showed a 5.4 × 4.6 cm hyperdense gastric body lesion and a suspected contained perforation at the gastroduodenal junction. He received IV fluids, pantoprazole, antibiotics, and four units of packed red blood cells in 24 hours of admission. After 60 hours in the ICU, he was transferred to step-down but developed recurrent massive hematemesis. Emergent endoscopy revealed a large, circumferential, cratered duodenal bulb ulcer with active bleeding. Given the ulcer’s size and associated perforation, empiric gastroduodenal artery embolization was performed despite no contrast extravasation.
Discussion: This case illustrates rare but life-threatening complications of NSAID use - duodenal perforation and massive upper GI bleeding. Despite initial hemodynamic stabilization, delayed EGD—due to concern for converting a contained perforation—may have contributed to recurrent hemorrhage. While caution with insufflation is warranted, early EGD evaluation should still be strongly considered in patients with high-risk features, to promptly identify and manage bleeding sources.
This case also underscores broader systemic issues, including the risks of unmonitored NSAID use and the healthcare disparities faced by incarcerated individuals. Limited access to medical oversight, gastroprotective strategies, and preventive education likely contributed to the severity of this patient’s presentation.
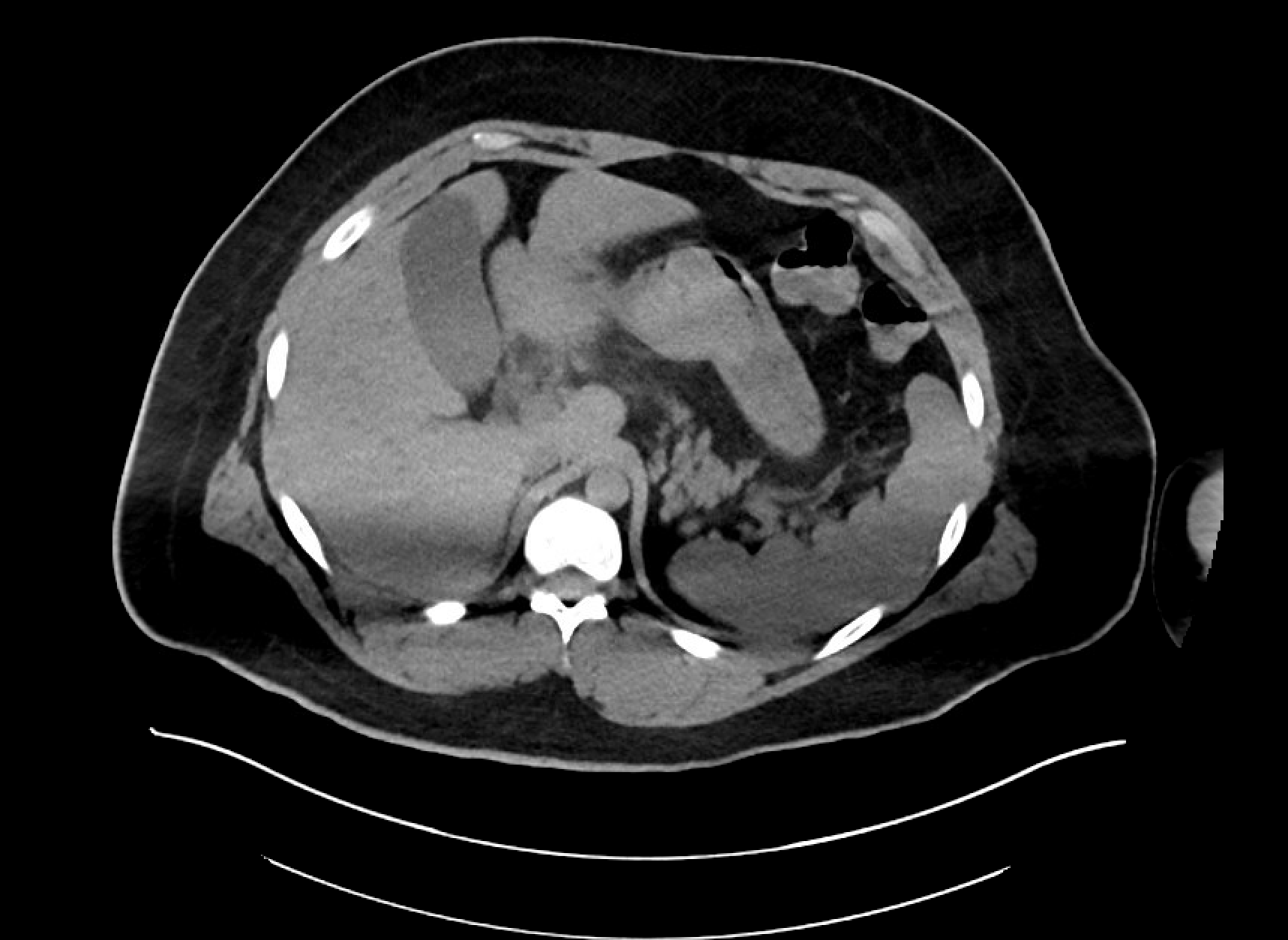
Figure: CTA Abdomen Pelvis on Admission in Emergency Department:
No focal acute arterial contrast extravasation in the GI lumen.
The stomach is noted to be contracted. with a 54 x 46 mm high attenuation bland appearing masslike filling defect in the gastric body measuring 53 HU on noncontrast phase suggesting gross hematoma.
Acute stranding surrounding the gastroduodenal junction with suspected walled-off perforation of the medial wall of the junction.
Disclosures:
Cameron Mitchell indicated no relevant financial relationships.
Muhammad Hassan indicated no relevant financial relationships.
Zana Nikolla indicated no relevant financial relationships.
Elizabeth Williams indicated no relevant financial relationships.
Cameron Mitchell, MD1, Muhammad Hassan, MD1, Zana Nikolla, MD2, Elizabeth Williams, DO2. P5232 - Behind Bars, Out of Sight: Catastrophic NSAID-Induced Duodenal Perforation in an Incarcerated Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Nuvance Health, Poughkeepsie, NY; 2Premier Medical Group, Poughkeepsie, NY
Introduction: Nonsteroidal anti-inflammatory drugs (NSAIDs) are widely used for musculoskeletal pain due to their anti-inflammatory and analgesic effects. However, by inhibiting prostaglandin synthesis, NSAIDs compromise the gastrointestinal (GI) mucosal barrier, increasing the risk of mucosal injury, ulceration, bleeding, and perforation. Chronic NSAID use is a well-established risk factor for peptic ulcer disease (PUD), though complications have become increasingly rare due to the accessibility of gastroprotective agents such as proton pump inhibitors (PPIs) and H2 blockers.
Case Description/
Methods: A 28-year-old incarcerated male with no known medical history presented with sudden-onset hematemesis and left upper quadrant abdominal pain. He had been taking naproxen 500 mg twice daily for six months following a metatarsal fracture. On EMS arrival, he was hypotensive (BP 80/40 mmHg), tachycardic (HR 140), and briefly unresponsive. Labs revealed leukocytosis (20.0 × 10⁹/L), hemoglobin 10.1 g/dL, elevated BUN/Cr ratio (35.7), and lactate 2.7 mmol/L. His Glasgow-Blatchford Bleeding Score was 11.
CT angiography showed a 5.4 × 4.6 cm hyperdense gastric body lesion and a suspected contained perforation at the gastroduodenal junction. He received IV fluids, pantoprazole, antibiotics, and four units of packed red blood cells in 24 hours of admission. After 60 hours in the ICU, he was transferred to step-down but developed recurrent massive hematemesis. Emergent endoscopy revealed a large, circumferential, cratered duodenal bulb ulcer with active bleeding. Given the ulcer’s size and associated perforation, empiric gastroduodenal artery embolization was performed despite no contrast extravasation.
Discussion: This case illustrates rare but life-threatening complications of NSAID use - duodenal perforation and massive upper GI bleeding. Despite initial hemodynamic stabilization, delayed EGD—due to concern for converting a contained perforation—may have contributed to recurrent hemorrhage. While caution with insufflation is warranted, early EGD evaluation should still be strongly considered in patients with high-risk features, to promptly identify and manage bleeding sources.
This case also underscores broader systemic issues, including the risks of unmonitored NSAID use and the healthcare disparities faced by incarcerated individuals. Limited access to medical oversight, gastroprotective strategies, and preventive education likely contributed to the severity of this patient’s presentation.
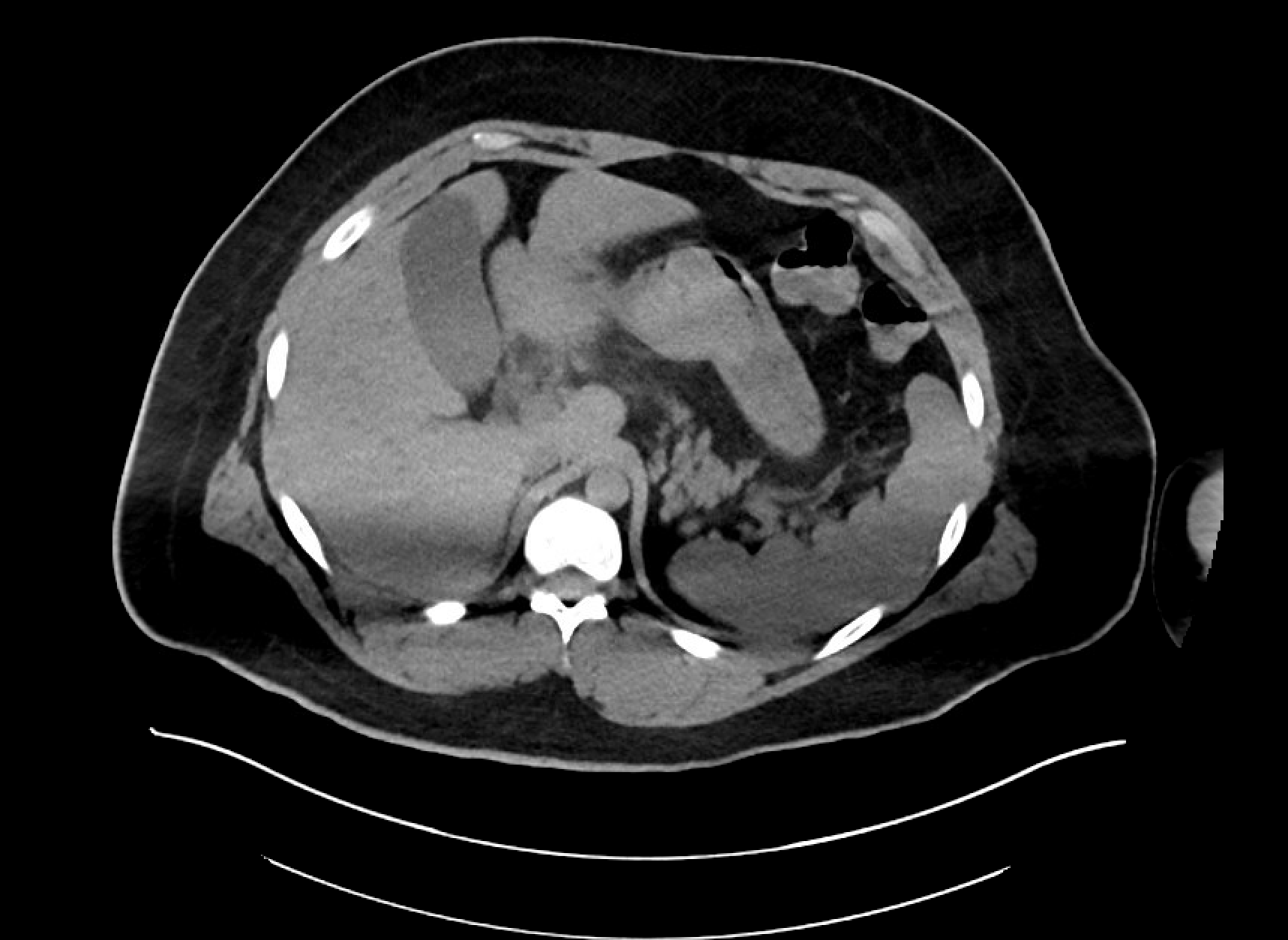
Figure: CTA Abdomen Pelvis on Admission in Emergency Department:
No focal acute arterial contrast extravasation in the GI lumen.
The stomach is noted to be contracted. with a 54 x 46 mm high attenuation bland appearing masslike filling defect in the gastric body measuring 53 HU on noncontrast phase suggesting gross hematoma.
Acute stranding surrounding the gastroduodenal junction with suspected walled-off perforation of the medial wall of the junction.
Disclosures:
Cameron Mitchell indicated no relevant financial relationships.
Muhammad Hassan indicated no relevant financial relationships.
Zana Nikolla indicated no relevant financial relationships.
Elizabeth Williams indicated no relevant financial relationships.
Cameron Mitchell, MD1, Muhammad Hassan, MD1, Zana Nikolla, MD2, Elizabeth Williams, DO2. P5232 - Behind Bars, Out of Sight: Catastrophic NSAID-Induced Duodenal Perforation in an Incarcerated Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
