Tuesday Poster Session
Category: GI Bleeding
P5224 - A Rare Case of Life-threatening Bleeding Related to Gastrointestinal Histoplasmosis in a Heart Transplant Recipient
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amey Joshi, MD (he/him/his)
University of Michigan Health - Sparrow
Lansing, MI
Presenting Author(s)
Award: ACG Presidential Poster Award
Amey Joshi, MD1, Hemangi Kale, MD2, Parag Kale, MD2, Seema Kudsia, MD2, Cesar Guerrero Miranda, MD2
1University of Michigan Health - Sparrow, Lansing, MI; 2Baylor Scott & White Medical Center, Dallas, TX
Introduction: Isolated small bowel involvement in gastrointestinal (GI) histoplasmosis presenting as overt bleeding is an exceedingly uncommon condition, even among immunosuppressed individuals, making its diagnosis and management challenging.
Case Description/
Methods: A 61-year-old male with a history of non-ischemic cardiomyopathy status post heart transplant four years ago on tacrolimus and sirolimus, chronic kidney disease stage IV, prior cytomegalovirus viremia, presented with symptoms of fatigue, melena, nausea, and early satiety ongoing for two days. On admission, he was afebrile and had mild hypotension and tachycardia. Initial labs revealed a hemoglobin (Hb) 6.1 g/dl, a normal WBC and platelet count, and serum creatinine 3.77 mg/dL (baseline 3.5). He received seven units of packed red blood cells due to blood loss. An EGD was performed, which revealed abnormal mucosal depositions with central vascular ectasia throughout the duodenum and the jejunum. Active bleeding was noted in one of the larger jejunal lesions and was controlled by argon plasma coagulation and PuraStat application. Biopsies were obtained. Despite this, melena and drop in Hb recurred, needing further transfusions. Scintigraphy scan confirmed active jejunal bleeding, which was then treated by IR guided embolization. Duodenal biopsies revealed histoplasmosis, and the patient was started on itraconazole. Tacrolimus was held temporarily based on trough levels that were affected by drug-drug interactions with itraconazole. The patient did not have any further bleeding or blood transfusions. Due to itraconazole intolerance, IV amphotericin B was given for five days, then switched to voriconazole. The patient continued to improve with his symptoms through the remaining hospital course.
Discussion: GI bleeding occurs in fewer than one-third of cases of histoplasmosis and involves the duodenum in less than 4% of patients without AIDS. Presentations can vary from ulcerations, mucosal inflammation, or strictures, but mucosal depositions with vascular ectasias have not been reported in heart transplant recipients. Anti-fungal therapy was key in treating the infection and associated bleeding. This case underscores the importance of lesional biopsies in transplant recipients with unexplained GI bleeding and highlights the need for careful immunosuppressive management during treatment.
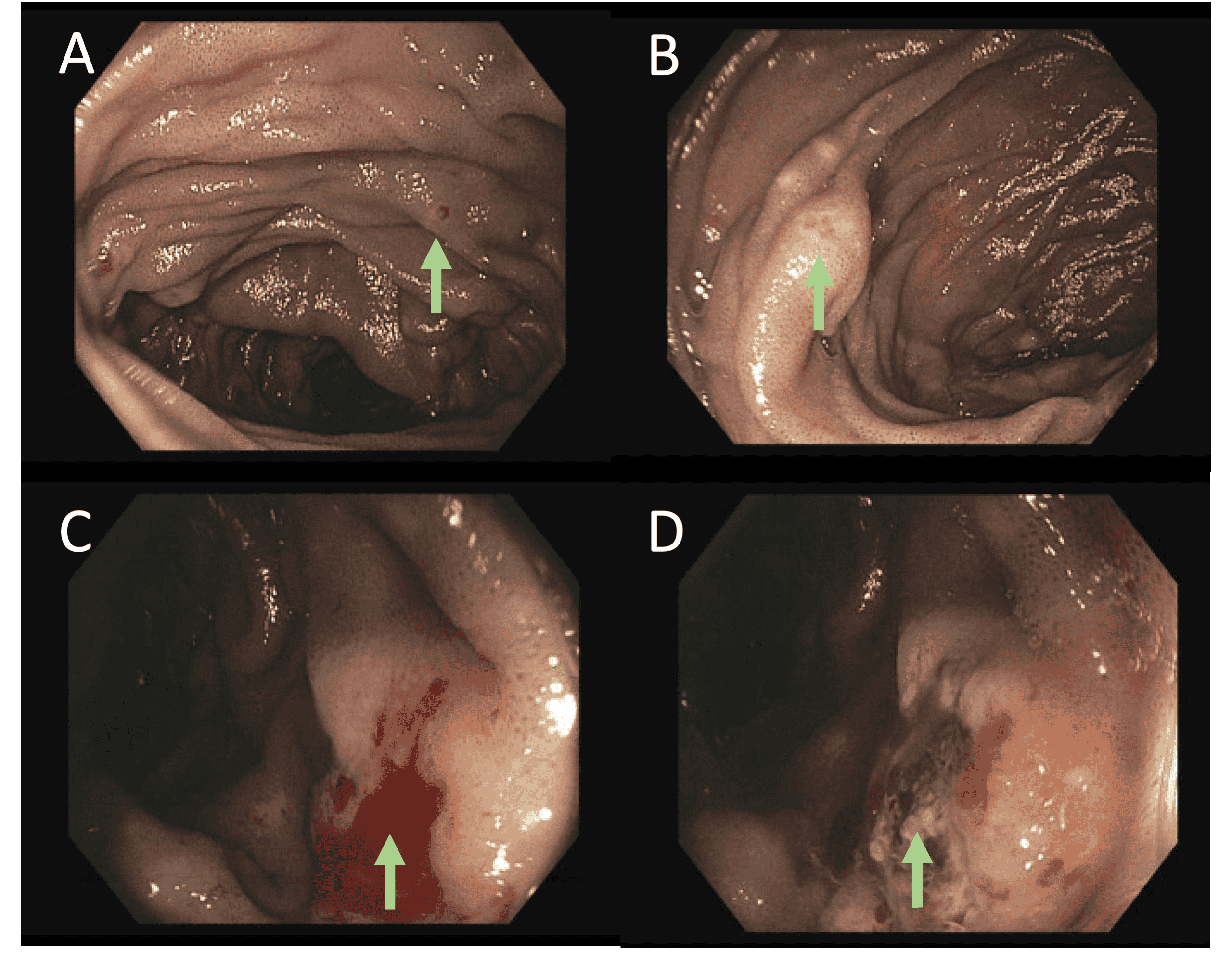
Figure: Esophagogastroduodenoscopy showing A) central vascular lesions on polypoidal lesions in second portion of duodenum (green arrow) B) polypoidal lesion in second portion of duodenum (green arrow) C) bleeding lesion in jejunum (green arrow) D) bleeding lesion after argon plasma coagulation and Purastat application in the jejunum (green arrow)
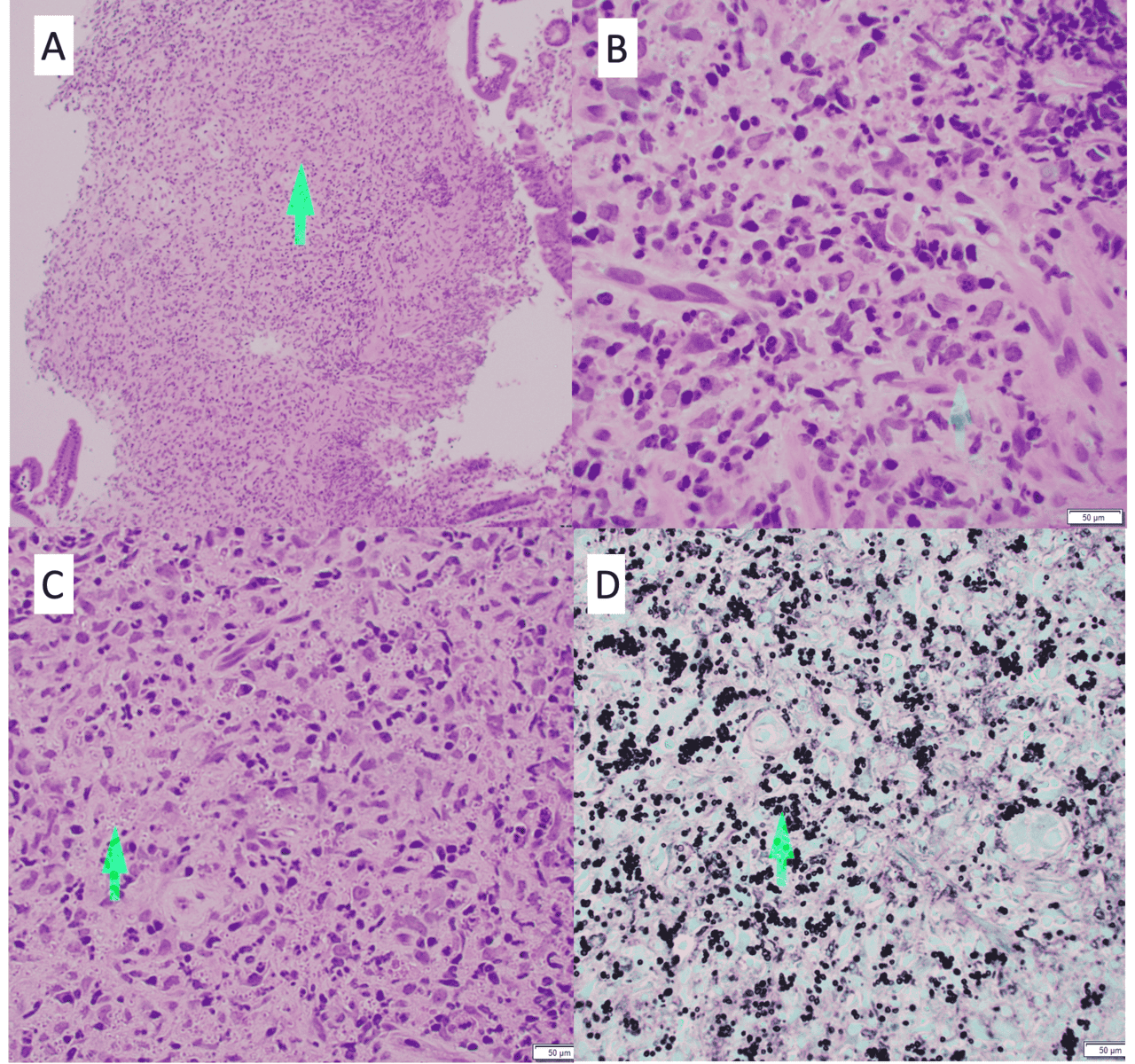
Figure: A) H&E stain of duodenal biopsy showing thickening submucosa and mucosa with granulomatous inflammation (green arrow) at 10 x microscopy, B) H&E stain showing red blood cell (green arrow) for comparison to cluster of yeasts at 40 x microscopy, C) H&E stain showing cluster of yeasts at 40 x microscopy (green arrow) and, D) GMS stain showing cluster of yeasts (green arrow)
Disclosures:
Amey Joshi indicated no relevant financial relationships.
Hemangi Kale indicated no relevant financial relationships.
Parag Kale indicated no relevant financial relationships.
Seema Kudsia indicated no relevant financial relationships.
Cesar Guerrero Miranda indicated no relevant financial relationships.
Amey Joshi, MD1, Hemangi Kale, MD2, Parag Kale, MD2, Seema Kudsia, MD2, Cesar Guerrero Miranda, MD2. P5224 - A Rare Case of Life-threatening Bleeding Related to Gastrointestinal Histoplasmosis in a Heart Transplant Recipient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Amey Joshi, MD1, Hemangi Kale, MD2, Parag Kale, MD2, Seema Kudsia, MD2, Cesar Guerrero Miranda, MD2
1University of Michigan Health - Sparrow, Lansing, MI; 2Baylor Scott & White Medical Center, Dallas, TX
Introduction: Isolated small bowel involvement in gastrointestinal (GI) histoplasmosis presenting as overt bleeding is an exceedingly uncommon condition, even among immunosuppressed individuals, making its diagnosis and management challenging.
Case Description/
Methods: A 61-year-old male with a history of non-ischemic cardiomyopathy status post heart transplant four years ago on tacrolimus and sirolimus, chronic kidney disease stage IV, prior cytomegalovirus viremia, presented with symptoms of fatigue, melena, nausea, and early satiety ongoing for two days. On admission, he was afebrile and had mild hypotension and tachycardia. Initial labs revealed a hemoglobin (Hb) 6.1 g/dl, a normal WBC and platelet count, and serum creatinine 3.77 mg/dL (baseline 3.5). He received seven units of packed red blood cells due to blood loss. An EGD was performed, which revealed abnormal mucosal depositions with central vascular ectasia throughout the duodenum and the jejunum. Active bleeding was noted in one of the larger jejunal lesions and was controlled by argon plasma coagulation and PuraStat application. Biopsies were obtained. Despite this, melena and drop in Hb recurred, needing further transfusions. Scintigraphy scan confirmed active jejunal bleeding, which was then treated by IR guided embolization. Duodenal biopsies revealed histoplasmosis, and the patient was started on itraconazole. Tacrolimus was held temporarily based on trough levels that were affected by drug-drug interactions with itraconazole. The patient did not have any further bleeding or blood transfusions. Due to itraconazole intolerance, IV amphotericin B was given for five days, then switched to voriconazole. The patient continued to improve with his symptoms through the remaining hospital course.
Discussion: GI bleeding occurs in fewer than one-third of cases of histoplasmosis and involves the duodenum in less than 4% of patients without AIDS. Presentations can vary from ulcerations, mucosal inflammation, or strictures, but mucosal depositions with vascular ectasias have not been reported in heart transplant recipients. Anti-fungal therapy was key in treating the infection and associated bleeding. This case underscores the importance of lesional biopsies in transplant recipients with unexplained GI bleeding and highlights the need for careful immunosuppressive management during treatment.
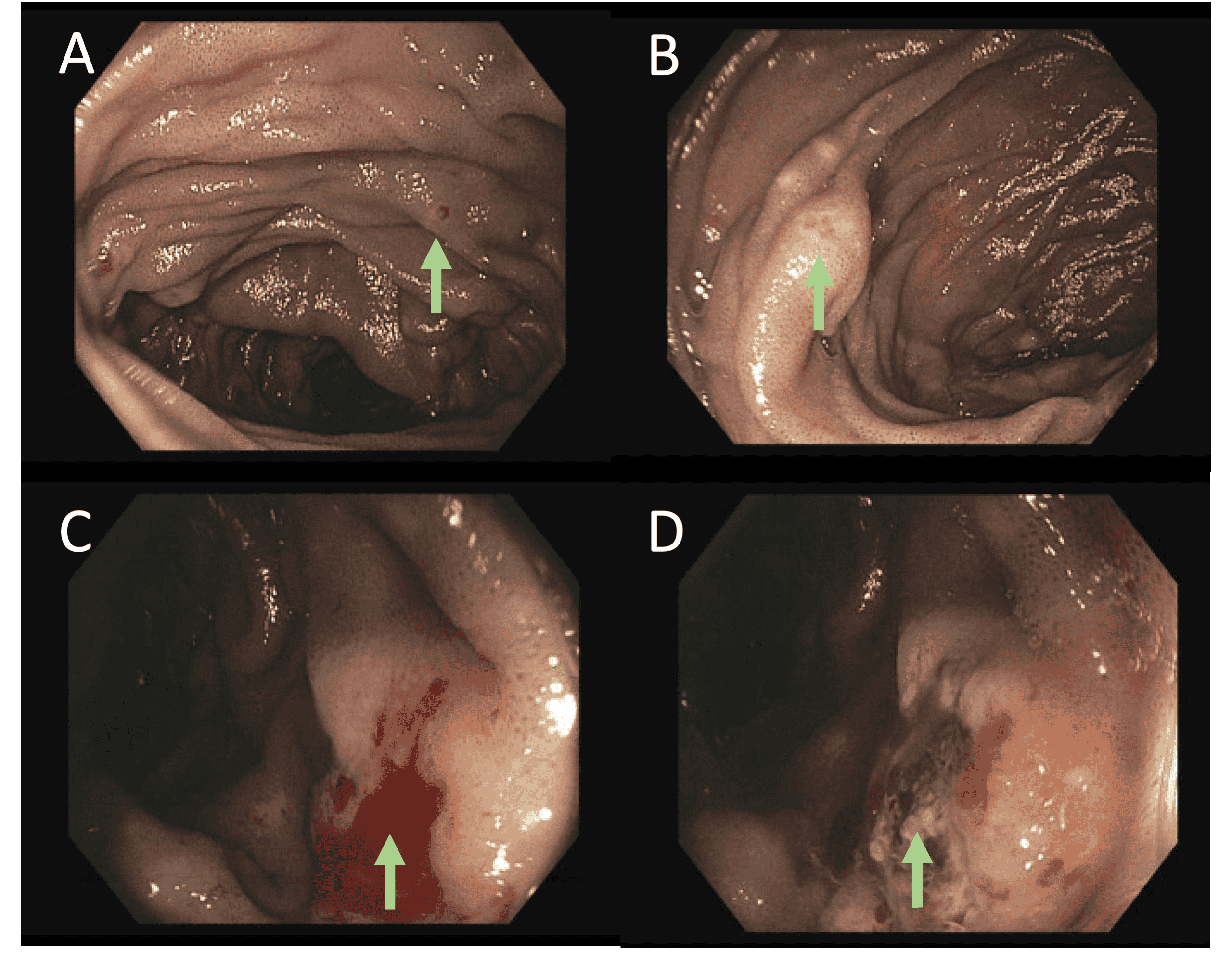
Figure: Esophagogastroduodenoscopy showing A) central vascular lesions on polypoidal lesions in second portion of duodenum (green arrow) B) polypoidal lesion in second portion of duodenum (green arrow) C) bleeding lesion in jejunum (green arrow) D) bleeding lesion after argon plasma coagulation and Purastat application in the jejunum (green arrow)
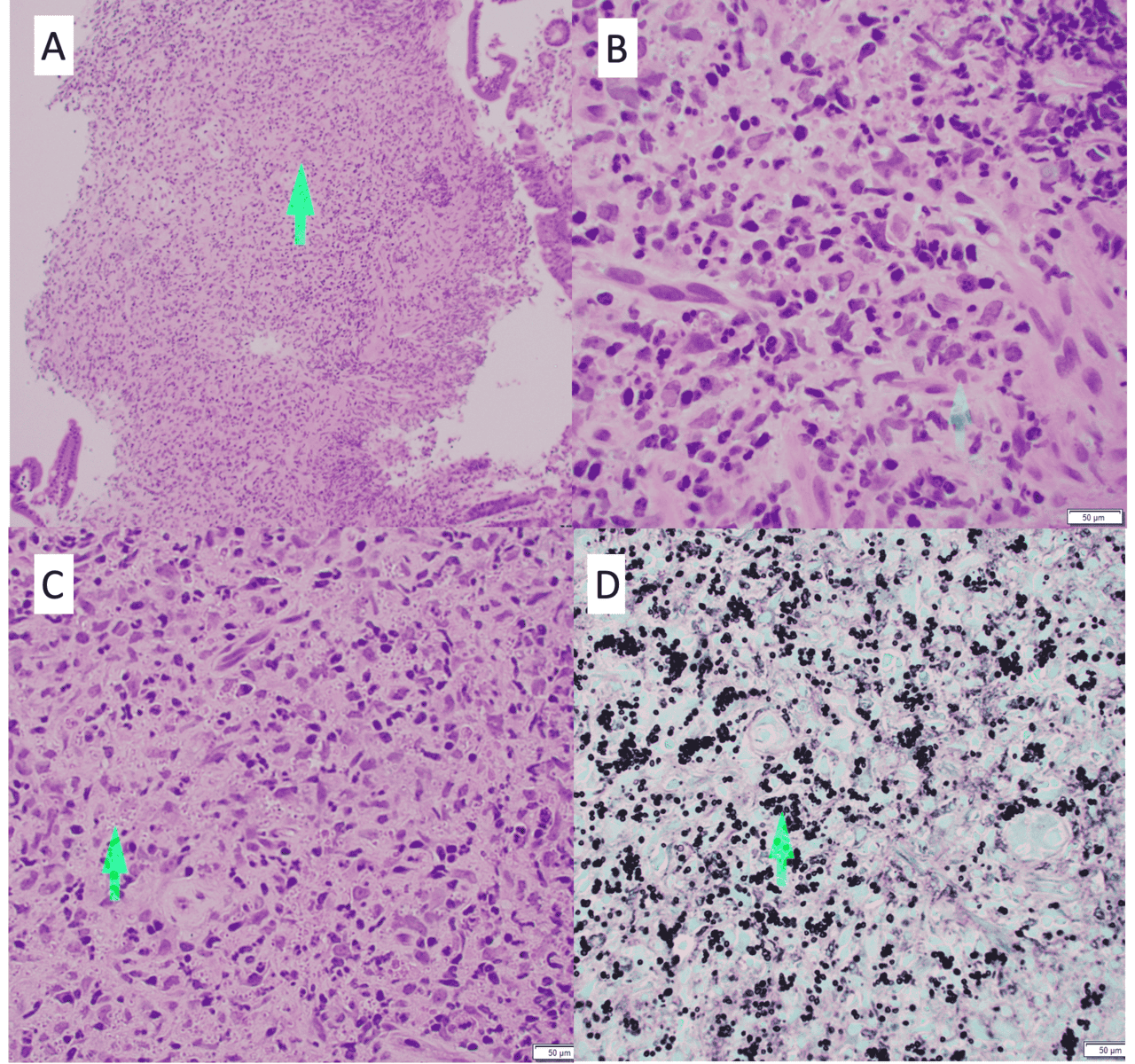
Figure: A) H&E stain of duodenal biopsy showing thickening submucosa and mucosa with granulomatous inflammation (green arrow) at 10 x microscopy, B) H&E stain showing red blood cell (green arrow) for comparison to cluster of yeasts at 40 x microscopy, C) H&E stain showing cluster of yeasts at 40 x microscopy (green arrow) and, D) GMS stain showing cluster of yeasts (green arrow)
Disclosures:
Amey Joshi indicated no relevant financial relationships.
Hemangi Kale indicated no relevant financial relationships.
Parag Kale indicated no relevant financial relationships.
Seema Kudsia indicated no relevant financial relationships.
Cesar Guerrero Miranda indicated no relevant financial relationships.
Amey Joshi, MD1, Hemangi Kale, MD2, Parag Kale, MD2, Seema Kudsia, MD2, Cesar Guerrero Miranda, MD2. P5224 - A Rare Case of Life-threatening Bleeding Related to Gastrointestinal Histoplasmosis in a Heart Transplant Recipient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

