Tuesday Poster Session
Category: GI Bleeding
P5216 - Exploring the Impact of NSTEMI on Outcomes of Lower GI Bleeding From Intestinal Vascular Disorders: Insights From a National Inpatient Sample
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HT
Hamza Tahir, MD (he/him/his)
Jefferson Einstein Hospital/Thomas Jefferson University
Philadelphia, PA
Presenting Author(s)
Hamza Tahir, MD, Bakhtawer Siraj, MD, Nandakumar Mohan, DO, Diaz-Caballero Luis, MD
Jefferson Einstein Hospital/Thomas Jefferson University, Philadelphia, PA
Introduction: NSTEMI complicating gastrointestinal bleeding can be challenging to manage and have negative consequences as a complex relationship exists between the two. Lower GI bleeding can worsen cardiac ischemia and be exacerbated by medications used to prevent or treat NSTEMI.
Using National Inpatient Sample data, we analyzed outcomes, interventions, and resource utilization in patients with lower GI bleeding from intestinal vascular disorders (e.g., ischemic colitis, mesenteric ischemia, mesenteric vein thrombosis), with and without subsequent NSTEMI.
Methods: The United States NIS (2018-2020) was queried to identify hospitalized patients with lower GI bleeding due to intestinal vascular disorders, with and without NSTEMI. Multivariable logistic regression adjusted for confounders. The primary outcome of our study was in-hospital mortality. The secondary outcomes were mean length of stay (LOS), mean total hospital charge (THC), blood transfusions, shock (hypovolemic, hemorrhagic, and septic shock), cardiac arrest, acute CVA, acute respiratory failure, sepsis, acute pulmonary embolism, deep venous thrombosis, colonoscopy performed, surgical intervention (exploratory laparotomy, Colectomy), mechanical ventilation and renal replacement therapy.
Results: Among 153,430 hospitalized patients with lower GI bleeding from vascular disorders, 1,380 (0.9%) had a diagnosis of NSTEMI. This group experienced a four-fold increase in inpatient mortality (P < 0.005) and an adjusted 2.62-day longer hospital stay (P < 0.05). NSTEMI patients had significantly higher rates of cardiac arrest, respiratory failure, deep venous thrombosis, mechanical ventilation, and renal replacement therapy (all P < 0.05). They also required more transfusions and had higher incidences of shock, acute kidney injury, and acute liver failure (P < 0.05), though these associations lost significance after adjusting for confounders. Notably, no significant differences were observed in total hospital costs, colonoscopies, or surgical interventions between the groups.
Discussion: Our study showed that NSTEMI, in conjunction with lower GI bleeding is associated with increased mortality, length of hospital stays, and increased risk of life-threatening complications in patients with lower GI bleeding predominantly from colonic ischemia compared to patients without NSTEMI. However, these findings should be further investigated in larger-scale trials.
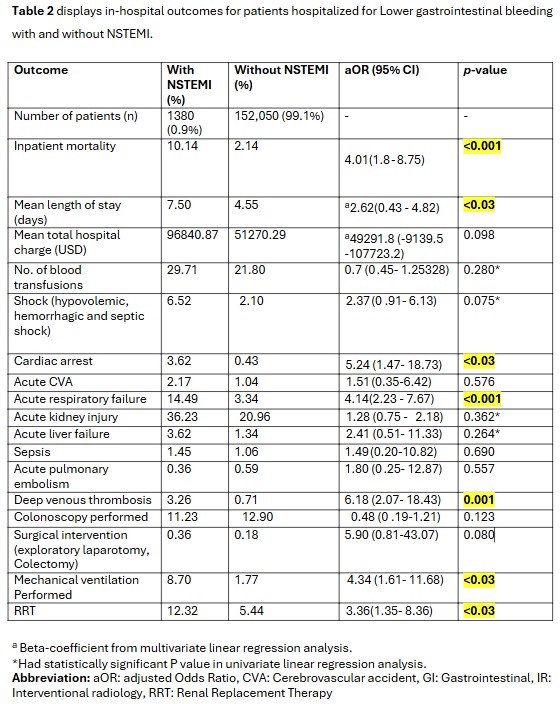
Figure: Table 2 displays in-hospital outcomes for patients hospitalized for Lower gastrointestinal bleeding with and without NSTEMI.
Disclosures:
Hamza Tahir indicated no relevant financial relationships.
Bakhtawer Siraj indicated no relevant financial relationships.
Nandakumar Mohan indicated no relevant financial relationships.
Diaz-Caballero Luis indicated no relevant financial relationships.
Hamza Tahir, MD, Bakhtawer Siraj, MD, Nandakumar Mohan, DO, Diaz-Caballero Luis, MD. P5216 - Exploring the Impact of NSTEMI on Outcomes of Lower GI Bleeding From Intestinal Vascular Disorders: Insights From a National Inpatient Sample, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Jefferson Einstein Hospital/Thomas Jefferson University, Philadelphia, PA
Introduction: NSTEMI complicating gastrointestinal bleeding can be challenging to manage and have negative consequences as a complex relationship exists between the two. Lower GI bleeding can worsen cardiac ischemia and be exacerbated by medications used to prevent or treat NSTEMI.
Using National Inpatient Sample data, we analyzed outcomes, interventions, and resource utilization in patients with lower GI bleeding from intestinal vascular disorders (e.g., ischemic colitis, mesenteric ischemia, mesenteric vein thrombosis), with and without subsequent NSTEMI.
Methods: The United States NIS (2018-2020) was queried to identify hospitalized patients with lower GI bleeding due to intestinal vascular disorders, with and without NSTEMI. Multivariable logistic regression adjusted for confounders. The primary outcome of our study was in-hospital mortality. The secondary outcomes were mean length of stay (LOS), mean total hospital charge (THC), blood transfusions, shock (hypovolemic, hemorrhagic, and septic shock), cardiac arrest, acute CVA, acute respiratory failure, sepsis, acute pulmonary embolism, deep venous thrombosis, colonoscopy performed, surgical intervention (exploratory laparotomy, Colectomy), mechanical ventilation and renal replacement therapy.
Results: Among 153,430 hospitalized patients with lower GI bleeding from vascular disorders, 1,380 (0.9%) had a diagnosis of NSTEMI. This group experienced a four-fold increase in inpatient mortality (P < 0.005) and an adjusted 2.62-day longer hospital stay (P < 0.05). NSTEMI patients had significantly higher rates of cardiac arrest, respiratory failure, deep venous thrombosis, mechanical ventilation, and renal replacement therapy (all P < 0.05). They also required more transfusions and had higher incidences of shock, acute kidney injury, and acute liver failure (P < 0.05), though these associations lost significance after adjusting for confounders. Notably, no significant differences were observed in total hospital costs, colonoscopies, or surgical interventions between the groups.
Discussion: Our study showed that NSTEMI, in conjunction with lower GI bleeding is associated with increased mortality, length of hospital stays, and increased risk of life-threatening complications in patients with lower GI bleeding predominantly from colonic ischemia compared to patients without NSTEMI. However, these findings should be further investigated in larger-scale trials.
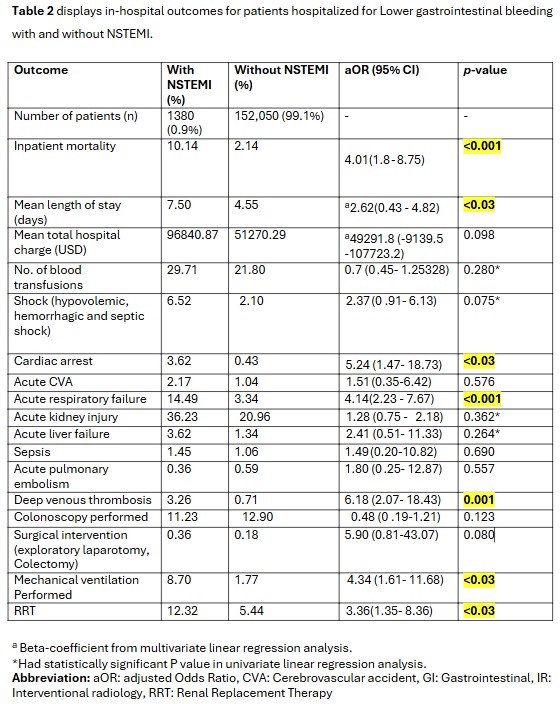
Figure: Table 2 displays in-hospital outcomes for patients hospitalized for Lower gastrointestinal bleeding with and without NSTEMI.
Disclosures:
Hamza Tahir indicated no relevant financial relationships.
Bakhtawer Siraj indicated no relevant financial relationships.
Nandakumar Mohan indicated no relevant financial relationships.
Diaz-Caballero Luis indicated no relevant financial relationships.
Hamza Tahir, MD, Bakhtawer Siraj, MD, Nandakumar Mohan, DO, Diaz-Caballero Luis, MD. P5216 - Exploring the Impact of NSTEMI on Outcomes of Lower GI Bleeding From Intestinal Vascular Disorders: Insights From a National Inpatient Sample, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
