Tuesday Poster Session
Category: GI Bleeding
P5210 - Impact of Cirrhosis Etiology on Clinical Outcomes in Hospitalized Patients With Upper Gastrointestinal Bleeding: A Nationwide Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RV
Renuka Verma, MD (she/her/hers)
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Renuka Verma, MD1, Kamleshun Ramphul, MD2, Yassin Naga, MD1, Banreet Dhindsa, MD3, Nikki Duong, MD4
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Independent researcher, Las Vegas, NV; 3Brown University / Rhode Island Hospital, East Providence, RI; 4Stanford University, Stanford, CA
Introduction: Upper gastrointestinal bleeding(UGIB) is a significant complication observed in cirrhosis patients, contributing to around a quarter of all deaths observed among them. The impact of cirrhosis etiology on outcomes in patients hospitalized with UGIB remains poorly understood.
Methods: Patients with cirrhosis hospitalized with UGIB were queried via the National Inpatient Sample(2016-2022). We excluded COVID-19 positive patients, cases discharged the same day, or transferred in/out, and those younger than 18 years. The use of esophagogastroduodenoscopy (EGD) (and early vs late) and the presence of adverse effects such as acute kidney injury(AKI), blood transfusion, vasopressors, septicemia, major adverse cardiac and cerebrovascular events(MACCE), and all-cause death were compared between patients who had underlying chronic hepatitis B(CHB), chronic hepatitis C(CHC), alcohol abuse(AA), metabolic dysfunction-associated steatohepatitis (MASH), primary sclerosing cholangitis (PSC), and primary biliary cholangitis (PBC), and expressed as adjusted odds ratio(aOR), 95% confidence interval(95%CI), and p-values. A two-way p-value of < 0.05 was considered significant.
Results: A total of 196,250 admissions with UGIB and cirrhosis were included. The most common etiology was AA (61.1%), followed by CHC (8.8%), MASH (8.7%), PBC (1.1%), CHB (0.9%), and PSC (0.2%). Patients with MASH were the oldest in our cohort, while those with PSC were the youngest (Figure 1).
Patients with CHB, MASH and PBC were less likely to undergo EGD, while patients with AA had significantly higher odds of undergoing EGD. AKI was more prevalent in those with AA, MASH, and PSC, and less likely in those with CHC and PBC. Blood transfusion was commonly used for those with PBC, and less frequently used in CHB, CHC, and MASH. Vasopressors were also more common in PSC, PBC, and AA cases, with fewer cases among those with MASH.
Discussion: Our findings underscore the critical impact that the underlying etiologies of cirrhosis have on the management, complications, and clinical outcomes following admission for upper gastrointestinal bleeding (UGIB). Although outcomes varied by etiology, cases related to alcohol-associated (AA) cirrhosis demonstrated the highest mortality risk. This may be attributable to delayed healthcare engagement and more advanced liver disease at the time of presentation. These results highlight the need for etiology-specific strategies to enhance patient care and optimize resource utilization.
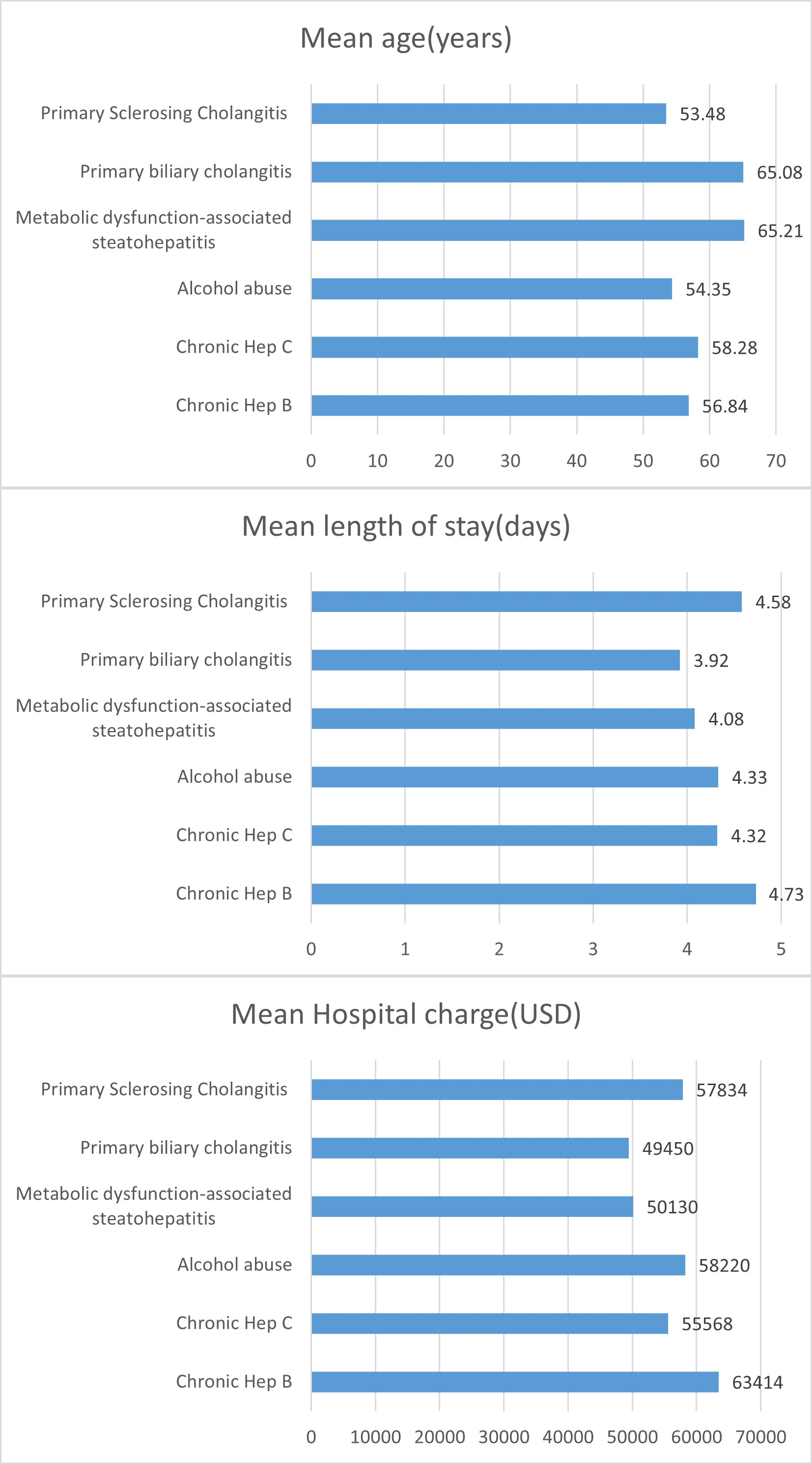
Figure: Figure 1- Mean hospital charge, length of stay, and age in Upper GI bleed patients
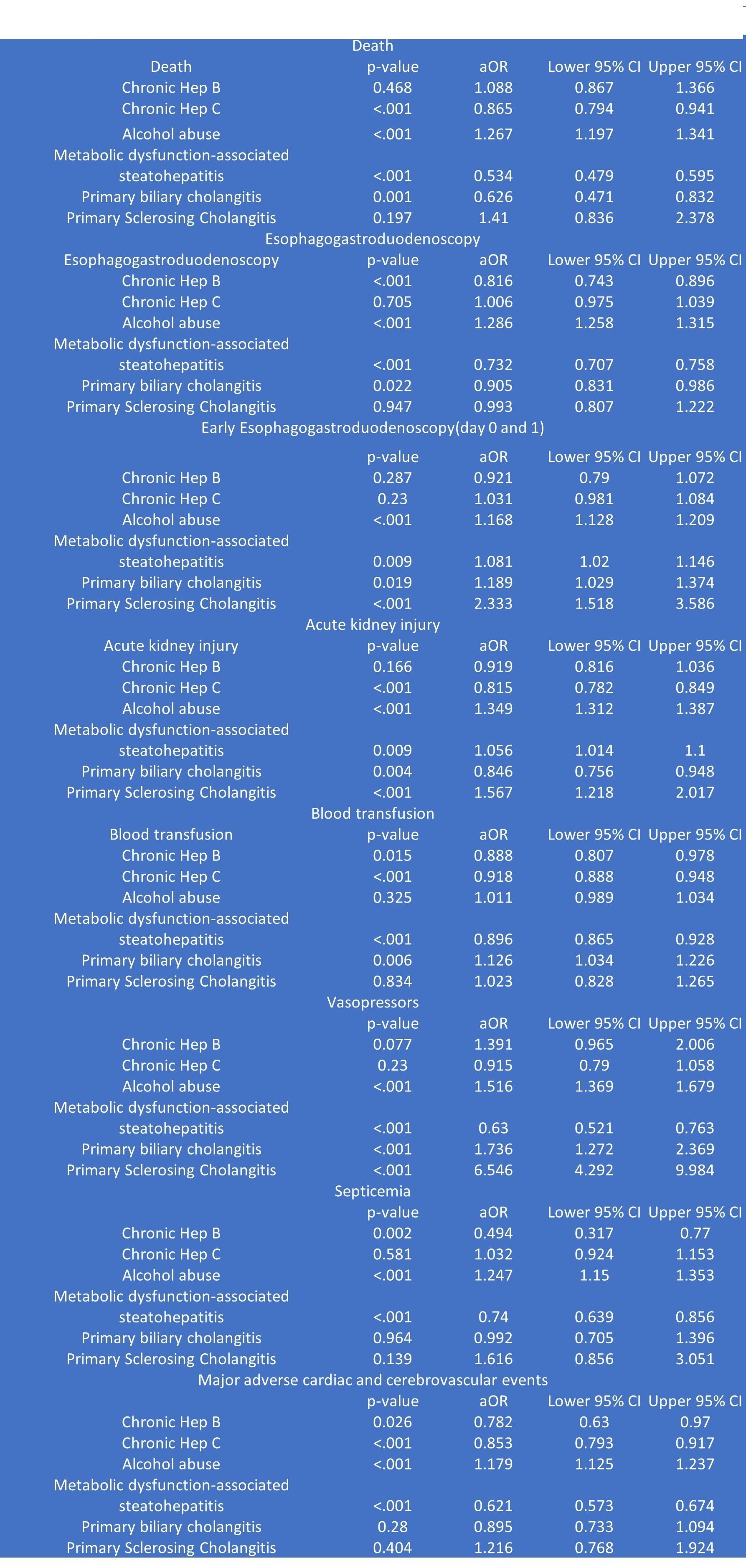
Figure: Table 1 - Management and complications in Upper GI bleed patients with different etiologies
Disclosures:
Renuka Verma indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Yassin Naga indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Renuka Verma, MD1, Kamleshun Ramphul, MD2, Yassin Naga, MD1, Banreet Dhindsa, MD3, Nikki Duong, MD4. P5210 - Impact of Cirrhosis Etiology on Clinical Outcomes in Hospitalized Patients With Upper Gastrointestinal Bleeding: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Independent researcher, Las Vegas, NV; 3Brown University / Rhode Island Hospital, East Providence, RI; 4Stanford University, Stanford, CA
Introduction: Upper gastrointestinal bleeding(UGIB) is a significant complication observed in cirrhosis patients, contributing to around a quarter of all deaths observed among them. The impact of cirrhosis etiology on outcomes in patients hospitalized with UGIB remains poorly understood.
Methods: Patients with cirrhosis hospitalized with UGIB were queried via the National Inpatient Sample(2016-2022). We excluded COVID-19 positive patients, cases discharged the same day, or transferred in/out, and those younger than 18 years. The use of esophagogastroduodenoscopy (EGD) (and early vs late) and the presence of adverse effects such as acute kidney injury(AKI), blood transfusion, vasopressors, septicemia, major adverse cardiac and cerebrovascular events(MACCE), and all-cause death were compared between patients who had underlying chronic hepatitis B(CHB), chronic hepatitis C(CHC), alcohol abuse(AA), metabolic dysfunction-associated steatohepatitis (MASH), primary sclerosing cholangitis (PSC), and primary biliary cholangitis (PBC), and expressed as adjusted odds ratio(aOR), 95% confidence interval(95%CI), and p-values. A two-way p-value of < 0.05 was considered significant.
Results: A total of 196,250 admissions with UGIB and cirrhosis were included. The most common etiology was AA (61.1%), followed by CHC (8.8%), MASH (8.7%), PBC (1.1%), CHB (0.9%), and PSC (0.2%). Patients with MASH were the oldest in our cohort, while those with PSC were the youngest (Figure 1).
Patients with CHB, MASH and PBC were less likely to undergo EGD, while patients with AA had significantly higher odds of undergoing EGD. AKI was more prevalent in those with AA, MASH, and PSC, and less likely in those with CHC and PBC. Blood transfusion was commonly used for those with PBC, and less frequently used in CHB, CHC, and MASH. Vasopressors were also more common in PSC, PBC, and AA cases, with fewer cases among those with MASH.
Discussion: Our findings underscore the critical impact that the underlying etiologies of cirrhosis have on the management, complications, and clinical outcomes following admission for upper gastrointestinal bleeding (UGIB). Although outcomes varied by etiology, cases related to alcohol-associated (AA) cirrhosis demonstrated the highest mortality risk. This may be attributable to delayed healthcare engagement and more advanced liver disease at the time of presentation. These results highlight the need for etiology-specific strategies to enhance patient care and optimize resource utilization.
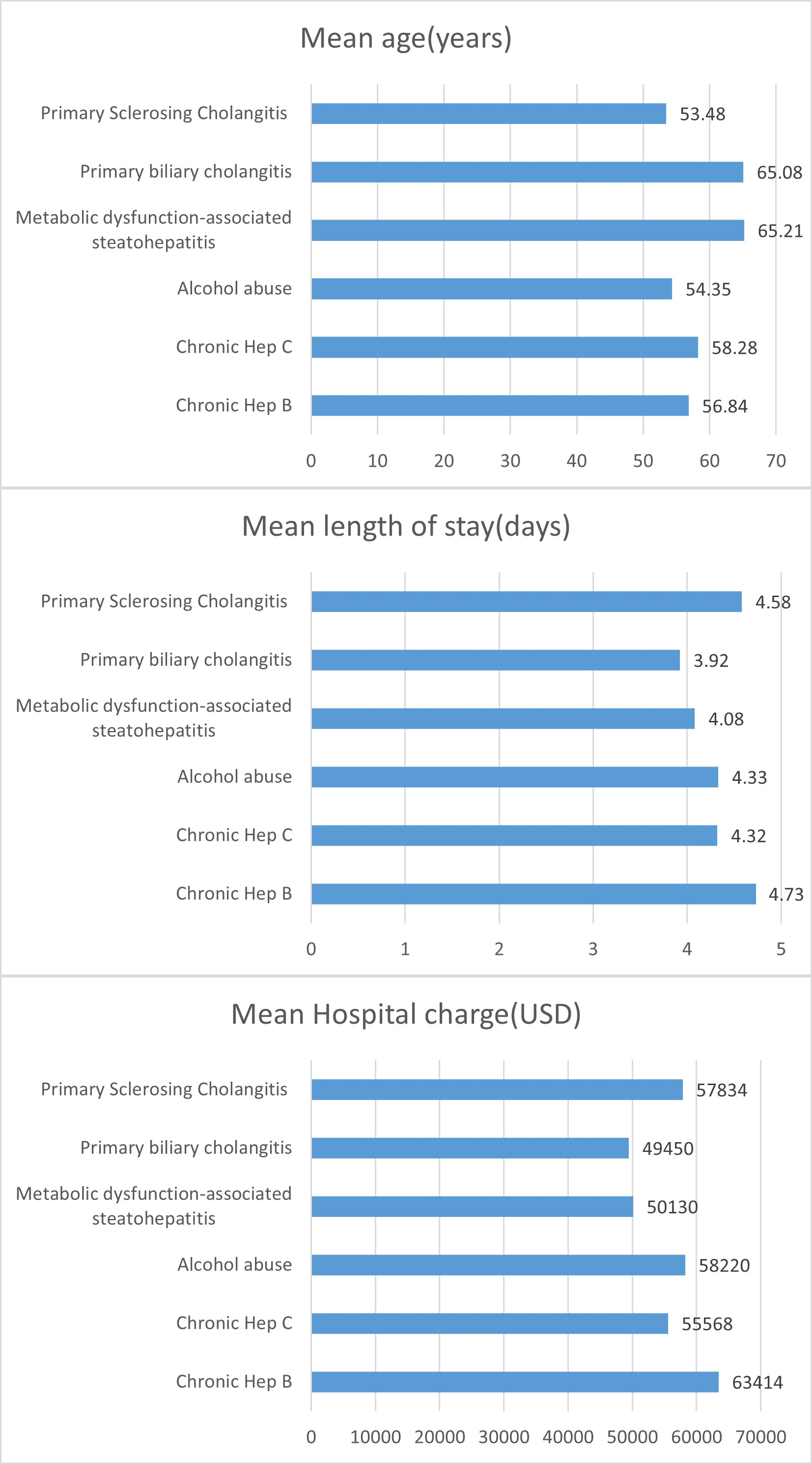
Figure: Figure 1- Mean hospital charge, length of stay, and age in Upper GI bleed patients
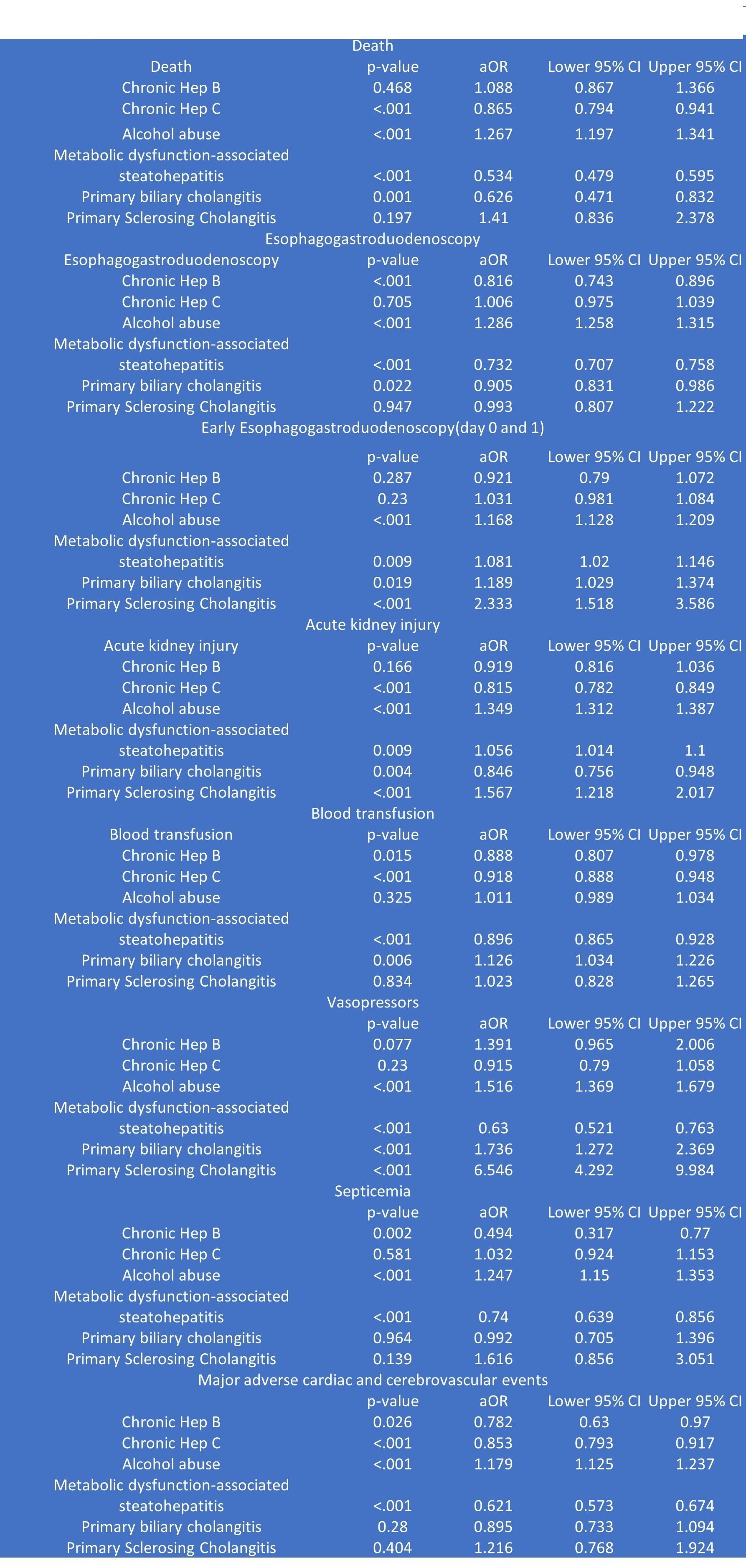
Figure: Table 1 - Management and complications in Upper GI bleed patients with different etiologies
Disclosures:
Renuka Verma indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Yassin Naga indicated no relevant financial relationships.
Banreet Dhindsa indicated no relevant financial relationships.
Nikki Duong indicated no relevant financial relationships.
Renuka Verma, MD1, Kamleshun Ramphul, MD2, Yassin Naga, MD1, Banreet Dhindsa, MD3, Nikki Duong, MD4. P5210 - Impact of Cirrhosis Etiology on Clinical Outcomes in Hospitalized Patients With Upper Gastrointestinal Bleeding: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
