Tuesday Poster Session
Category: GI Bleeding
P5209 - Healthcare Inequities in Upper Gastrointestinal Bleeding: A Study of Racial Disparities: A 5-Year Retrospective Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- CD
Chaula Desai, MD
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Chaula Desai, MD, Sweta Lohani, MD, Iyad Al-Bustami, MD, MPH, Aashay Dharia, MD, Anuj Sharma, MD
Brooklyn Hospital Center, Brooklyn, NY
Introduction: Gastrointestinal (GI) bleeding is a medical emergency that requires early diagnosis and treatment. Numerous studies have documented the influence of racial disparities in healthcare, revealing significant differences in clinical outcomes across a wide range of medical conditions. We aimed to study the impact of racial disparities in GI bleed outcomes in Black/Hispanic
patients compared to other races.
Methods: The National Inpatient Sample database from 2016-2020 was used to identify adult hospitalizations with upper gastrointestinal (GI) bleeding using the appropriate ICD-10 codes. The study population was divided into two groups - Black/Hispanic patients in one group, and all other races in the other group. Statistical analysis with chi-square test and t-test was used to compare key clinical outcomes between the two groups. Multivariate analysis was performed to account for possible confounders. A p-value of 0.05 or less was assigned statistical significance.
Results: A total of 2,926,039 adult hospitalizations with upper GI bleeding were identified, out of which 740,288 (25.3%) were Black or Hispanic and 2,185,751 (74.7%) belonged to other races. Black and Hispanic populations with GI bleed were likely to be younger (mean age 62 vs 68). Mortality rates were similar between both groups. However, Black/Hispanic populations were less likely to receive endoscopic intervention (aOR 0.86, p< 0.001). Among those who did receive endoscopy, early endoscopy (defined as within 48 hours) was performed in a smaller proportion of Blacks/Hispanics compared to other races. Black/Hispanic populations were more likely to
receive blood transfusions (aOR 1.25, p< 0.001), ventilator support (aOR 1.43, p< 0.001), and vasopressors (aOR 1.08, p=0.014).
Discussion: Our study highlights significant racial disparities in the management of upper GI bleeding. Blacks and Hispanics have an increased need for blood transfusions, ventilator support, and vasopressors in this population. This likely points to a more complicated clinical course and a delay in endoscopic intervention could potentially be one of the factors influencing these outcomes. Apart from affecting outcomes, these racial disparities also place a significant burden on healthcare costs. These findings highlight the need for further investigation into the underlying causes of these disparities and the development of targeted interventions to improve outcomes in minority populations with GI bleeding.
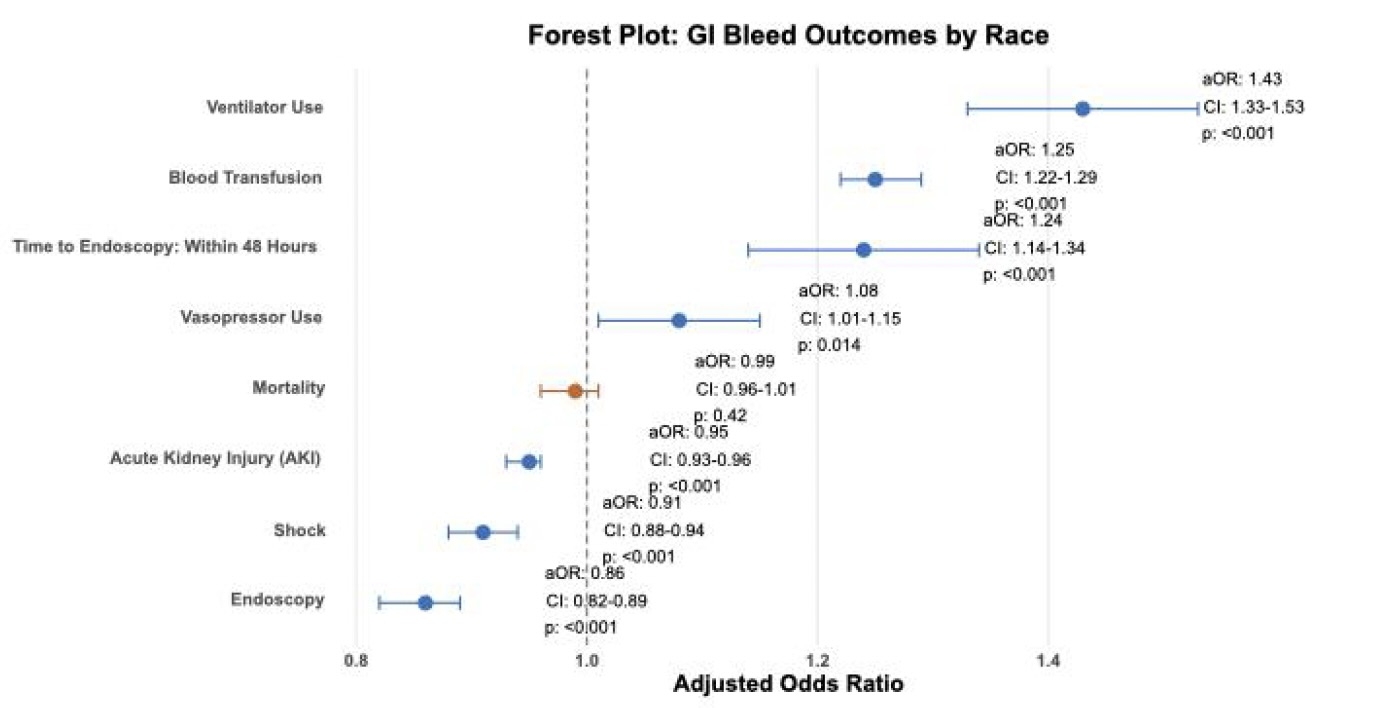
Figure: Forest Plot

Figure: Results
Disclosures:
Chaula Desai indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Iyad Al-Bustami indicated no relevant financial relationships.
Aashay Dharia indicated no relevant financial relationships.
Anuj Sharma indicated no relevant financial relationships.
Chaula Desai, MD, Sweta Lohani, MD, Iyad Al-Bustami, MD, MPH, Aashay Dharia, MD, Anuj Sharma, MD. P5209 - Healthcare Inequities in Upper Gastrointestinal Bleeding: A Study of Racial Disparities: A 5-Year Retrospective Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Brooklyn Hospital Center, Brooklyn, NY
Introduction: Gastrointestinal (GI) bleeding is a medical emergency that requires early diagnosis and treatment. Numerous studies have documented the influence of racial disparities in healthcare, revealing significant differences in clinical outcomes across a wide range of medical conditions. We aimed to study the impact of racial disparities in GI bleed outcomes in Black/Hispanic
patients compared to other races.
Methods: The National Inpatient Sample database from 2016-2020 was used to identify adult hospitalizations with upper gastrointestinal (GI) bleeding using the appropriate ICD-10 codes. The study population was divided into two groups - Black/Hispanic patients in one group, and all other races in the other group. Statistical analysis with chi-square test and t-test was used to compare key clinical outcomes between the two groups. Multivariate analysis was performed to account for possible confounders. A p-value of 0.05 or less was assigned statistical significance.
Results: A total of 2,926,039 adult hospitalizations with upper GI bleeding were identified, out of which 740,288 (25.3%) were Black or Hispanic and 2,185,751 (74.7%) belonged to other races. Black and Hispanic populations with GI bleed were likely to be younger (mean age 62 vs 68). Mortality rates were similar between both groups. However, Black/Hispanic populations were less likely to receive endoscopic intervention (aOR 0.86, p< 0.001). Among those who did receive endoscopy, early endoscopy (defined as within 48 hours) was performed in a smaller proportion of Blacks/Hispanics compared to other races. Black/Hispanic populations were more likely to
receive blood transfusions (aOR 1.25, p< 0.001), ventilator support (aOR 1.43, p< 0.001), and vasopressors (aOR 1.08, p=0.014).
Discussion: Our study highlights significant racial disparities in the management of upper GI bleeding. Blacks and Hispanics have an increased need for blood transfusions, ventilator support, and vasopressors in this population. This likely points to a more complicated clinical course and a delay in endoscopic intervention could potentially be one of the factors influencing these outcomes. Apart from affecting outcomes, these racial disparities also place a significant burden on healthcare costs. These findings highlight the need for further investigation into the underlying causes of these disparities and the development of targeted interventions to improve outcomes in minority populations with GI bleeding.
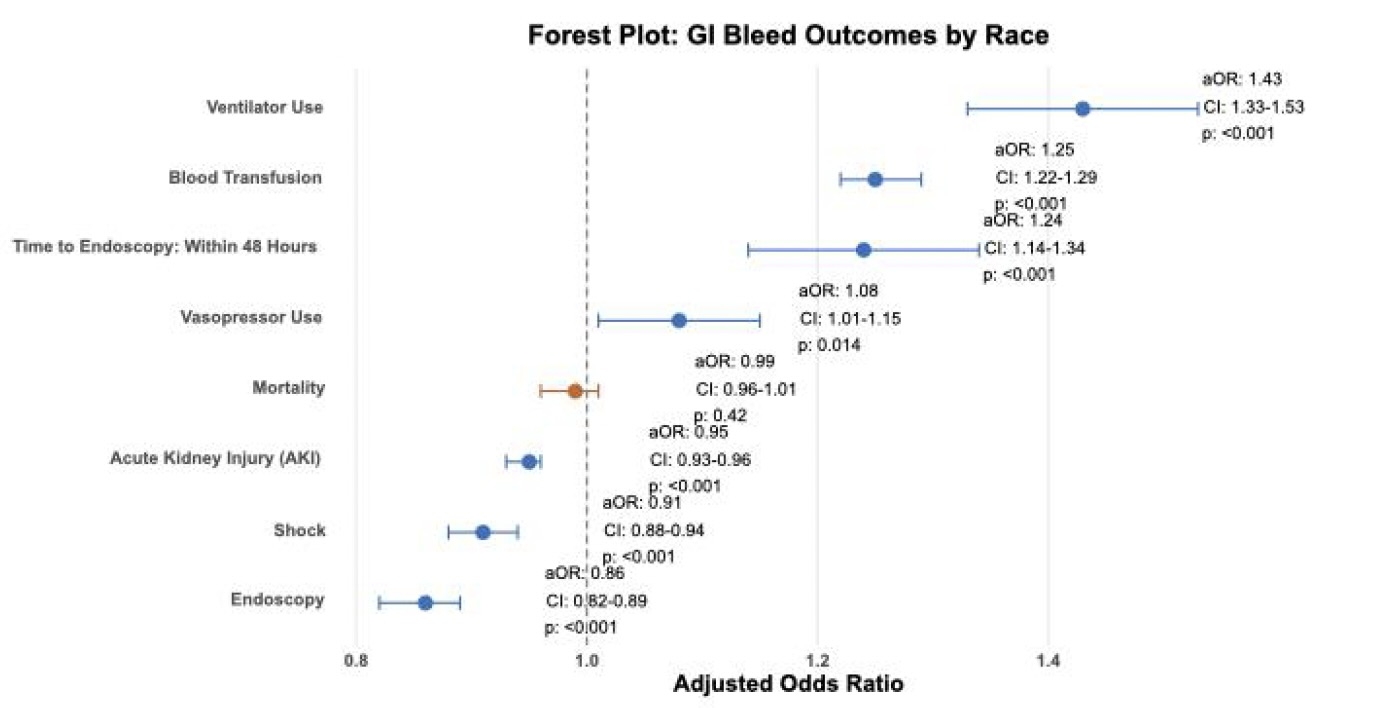
Figure: Forest Plot

Figure: Results
Disclosures:
Chaula Desai indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Iyad Al-Bustami indicated no relevant financial relationships.
Aashay Dharia indicated no relevant financial relationships.
Anuj Sharma indicated no relevant financial relationships.
Chaula Desai, MD, Sweta Lohani, MD, Iyad Al-Bustami, MD, MPH, Aashay Dharia, MD, Anuj Sharma, MD. P5209 - Healthcare Inequities in Upper Gastrointestinal Bleeding: A Study of Racial Disparities: A 5-Year Retrospective Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

